“I think, by and large, we are all finding more uses for OCT, and it has made its way into the evaluation of cataract patients,” says Samuel Masket, MD, who is in practice in Los Angeles.
Steven Safran, MD, a surgeon from Lawrenceville, N.J., agrees. “I have been advocating for a long time for using OCT to evaluate patients for cataract surgery. It used to be that high-definition OCT was a retina surgeon’s tool. I got an OCT Spectralis in 2008, and it became pretty clear to me at that point that this was something that all ophthalmologists needed to have. Without looking at the macula, you really have no idea what’s going on there. In some respects, performing OCT is more important than performing topography. Looking at the retina with a 78-D lens is like a satellite image, while performing OCT is like having a Jeep on the ground,” he explains.
OCT was shown to effectively diagnose macular changes preoperatively and postoperatively in a recent study.1 This report was conducted to assess the ability of spectral-domain OCT to diagnose macular changes pre- and post-cataract surgery and to identify changes in central foveal thickness relative to age, gender and the presence of concomitant ophthalmic pathologies for six months following surgery.
In this prospective study, patients were evaluated by OCT within five hours before surgery and at 7, 30, 60, 90 and 180 days postoperatively, with respect to central foveal thickness and presence of maculopathy.
The study included 98 eyes of 98 patients. Patients’ mean age was 71.4 years; preoperative mean visual acuity was 0.27 logMAR; and final mean visual acuity was 0.73 logMAR. Twenty-one patients had diabetes mellitus, 10 patients had age-related macular degeneration, three had epiretinal membrane and four had glaucoma. Sixty eyes had no other ophthalmic-related pathologies, with a mean preoperative central foveal thickness of 222 μm, which progressively increased up to postoperative day 60 when it reached a mean of 227.2 μm. No pseudophakic cystoid macular edema was seen. Mean central foveal thickness was statistically significantly different between patients with no other ophthalmic-related pathologies and diabetic patients, from 30 days postoperatively. Four eyes had a preoperative diagnosis of age-related macular degeneration as measured by ophthalmoscopy. OCT was performed within five hours before surgery, and six additional patients were found to have age-related macular degeneration. Of the 98 total eyes, 10 were diagnosed with maculopathy only by OCT exam. Binocular indirect ophthalmoscopy was unable to detect such changes.
In this study, OCT diagnosed preoperative maculopathies in 21.4 percent of the patients and was found to be more effective than binocular indirect ophthalmoscopy, which
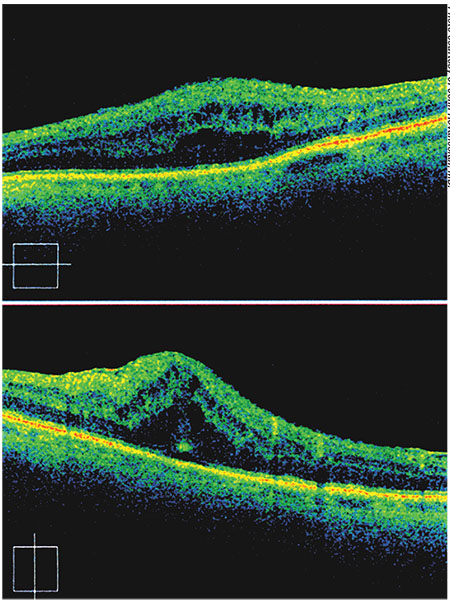 |
| OCT image showing cystoid macular edema in a patient with diabetic retinopathy. |
Premium IOLs
While OCT can be helpful in all patients, it’s especially important in patients considering a premium IOL. “You are flying blind without having an OCT. I think that every patient who is going to undergo cataract surgery can potentially benefit from having a preoperative OCT evaluation of the macula, particularly if he or she is considering a so-called premium lens,” Dr. Safran says. “I don’t know if most surgeons are routinely using OCT, but I think that’s the trend. Most surgeons who do diffractive multifocals certainly are.”
Some IOLs, such as diffractive multifocals, are contraindicated in the setting of macular disease, so it is helpful for surgeons to have as much information as possible before implanting one of these lenses. “Patients will not be happy postoperatively if they pay a premium price for a premium lens and then have a less-than-desirable visual outcome because they have an epiretinal membrane or subretinal fluid that was present prior to surgery and not detected. It’s not really defensible these days to simply say you didn’t know, when you could easily obtain this information before making a specific IOL recommendation,” he explains.
Dr. Safran also believes that OCTs are important when implanting standard lenses. “However, the stakes aren’t as high for two reasons: One is that you are not asking patients to pay out-of-pocket for an outcome that you are promising but that you will never be able to achieve if there are macular issues. The other is that some of the so-called premium lenses are actually not as good as a monofocal lens from a visual-quality standpoint. Using multifocal IOLs in patients with macular disease may actually hurt them rather than help them. In fact, they might not be able to drive or read as well with this compromised function,” he adds.
According to John Hovanesian, MD, who is in practice in Laguna Hills, Calif., today’s cataract surgery patients are much more particular than previous generations about their outcomes. “They expect normal vision like they had when they were a much younger person,” he says. “Unfortunately, these patients, whose average age is about 70 years old, often have co-morbidities that affect macular function, like epi-retinal membranes, early dry macular degeneration or other problems that can limit their visual potential. Some of these subtle findings are difficult or impossible to see when viewing the macula preoperatively through a cataract. OCT, which gives us a high-resolution cross-sectional image of the foveal region, can identify problems that would otherwise derail a satisfactory outcome for patients. This is particularly important when using multifocal lenses, where the lens itself degrades the optics of the eye to a small degree in exchange for giving multiple depths of focus.”
It’s imperative that patients understand co-morbidities that could affect their visual outcomes after their cataract surgery. “I’m a big fan of showing patients a picture of their OCT so they can see how theirs compares to a normal OCT. In my experience, patients with abnormal OCTs do not necessarily need to forgo premium cataract surgery. However, it alters their options,” Dr. Hovanesian says.
If they should forgo a multifocal lens because of their macular issue, then they may be able to consider an accommodating lens, a toric lens, or advanced monovision. “As a general rule, I won’t implant a presbyopia-correcting lens in a patient whose visual potential is less than 20/25, although there may be exceptions,” he notes.
Dr. Hovanesian says that refractive cataract surgery is very popular in his practice in southern California. “About 75 percent of our patients choose to have some type of premium refractive option. I tell patients that in order for them to have perfect vision, everything in their eye has to be perfect, not just our surgery. Often, not everything is perfect, so I use OCT in all of my cataract patients,” he adds.
According to Dr. Masket, there are two issues to consider when evaluating a cataract surgery patient. “One is determining the best lens device or the best surgical course for your patient. The other issue is what is and is not reimbursable. Many surgeons feel that before considering any type of multifocal or diffractive optic lens, which would include the new Symfony lens, one should be certain of macular health. Any disturbance, particularly to the macular surface where you might have vitreomacular traction or an epiretinal membrane, could lead to a less-than-desirable outcome. Vitreomacular traction can be missed by the anterior segment surgeon on routine examination of the posterior segment. I think many of us agree that, when considering any diffractive optic lens, it’s a good idea to study the macula region with OCT,” he says.
Dr. Masket says that he’s not sure whether OCT is necessary in routine cataract surgery cases. “However, we know from the literature that, in dry macular degeneration, the condition will not be worsened by cataract surgery. However, if an occult neovascular membrane is missed, cataract surgery can worsen the course of wet AMD, so I always use OCT in any patients with macular degeneration to make certain that we are not missing a choroidal neovascular membrane. In these cases, we refer patients to a vitreoretinal specialist for the treatment of that lesion prior to cataract surgery. Treatment usually consists of an anti-VEGF drug injection,” he adds.
The timing of cataract surgery is coordinated with the vitreoretinal specialist, in terms of giving the anti-VEGF injections at the appropriate intervals prior to the surgery. “Optical coherence tomography is of huge importance in any case of age-related macular degeneration,” Dr. Masket says. “In the consideration of a diffractive optic, I think it’s important to make sure that there is no surface disease that might be missed during the clinical examination. The reimbursement issue then comes into play because, for patients who have normal exams and are asymptomatic, obviously, the test is not and should not be reimbursable. The physician then must bear the time and expense of the test. It’s okay, though: I think it’s a very good ounce of prevention. My practice partner has taken to studying every cataract patient just to be certain that disease is not missed. We know, for example, if there is an epiretinal membrane or macular pucker, there is a greater likelihood of cystoid macular edema following surgery. We tend to pretreat these patients with steroidal and nonsteroidal agents for at least a week prior to cataract surgery,” Dr. Masket says.
Reimbursement
Unfortunately, OCT can only be billed to insurance if the patient has existing macular disease. If it is used in routine cataract patients, it will need to be billed to the patient or not reimbursed. “We recognize the value of OCT in everyone, even if we don’t get paid to do it,” Dr. Hovanesian notes. “Part of our fee for refractive cataract surgery includes the use of a screening OCT for patients without existing macular disease. In other words, for patients who have exam findings and suspicion for macular disease, you can and should do an OCT, and you can and should bill for it. For patients in whom it is being used as a screening test, where no expectation of macular disease exists and you are doing it just to make sure there’s nothing there, you can’t bill insurance or Medicare for that. We do it for no charge because we want the information. It’s part of doing the right thing for our patients and maintaining our reputation.”
He adds that the Centers for Medicare and Medicaid Services is discussing global fees for cataract surgery, although nothing has been finalized. “A ‘global fee’ means that it would cover preoperative testing, intraoperative tests, and postoperative testing and care. So, a global fee would make it so that it would be on the surgeon if he or she wanted to do these extra tests. If these changes come to pass, clinicians will need to make even more decisions like this,” he explains. REVIEW
Dr. Hovanesian is a consultant to Carl Zeiss Meditec, Bausch + Lomb, Alcon and Abbott Medical Optics. Dr. Safran and Dr. Masket do not have any financial interests to disclose.
1. Moreira CA, Moreira CA, Moreira ATR. Optical coherence tomography in patients undergoing cataract surgery. Arq Bras Oftalmol. 2015;78:4.



