Classifying Complications
The Five-S system is an expansion of a three-level corneal classification system I devised several years ago.1 The three-level system was based on the tissue components involved in the LASIK surgery, and I assigned LASIK corneal complications to Level I (corneal section), Level II (interface) or Level III (ablation bed). This helped identify and treat a range of corneal problems.
 |
| Corneoplastique helped this PK patient overcome his cylinder and see 20/25. |
Similarly, the Five-S system addresses questions about the cornea's state in order to customize a treatment plan, but is applicable to other previous surgeries in addition to LASIK. To aid in diagnosis, I use the Oculus Pentacam and the ReSeevit imaging system (Veatch Ophthalmic Instruments, Tempe, Ariz.).
Since the Five-S method is a systematic approach, I like to think of it as "logic in action." Here are its components:
1. Sight. Is the patient correctable to 20/20 with glasses and/or hard contact lenses?
2. Site. Is the involvement central or peripheral?
3. Scar. Is the cornea clear or opaque?
4. Strength. Is the cornea thick or thin?
5. Shape. Is the curvature steep, flat or is there regular or irregular astigmatism?
Corneoplastique
Though the Five-S system allows you to reliably classify corneal surgery complications, success in treating them depends on your knowledge of not only LASIK but lamellar corneal surgery in general, and your ability to deal with the possible complications of such surgeries. Surgeons must be familiar with the wide spectrum of advanced surgical options available to provide the most appropriate way to deal with a problem.
I've combined techniques such as amniotic membrane grafts, lamellar corneal surgery, glues, synthetic devices such as Intacs, and the excimer laser in stages to provide a treatment plan I've come to call corneoplastique, a concept I first presented at the 2005 meeting of the South African Society of Cataract and Refractive Surgery. Corneoplastique has been very successful in my practice. I've used it to address a myriad of situations, such as LASIK/PRK complications, advanced pterygia removal, corneal scars from infection, trauma and surgery, and poor outcomes from RK, ALK, epikeratophakia and phakic implants. Since I've begun using it, I have yet to perform a conventional corneal transplant for a post-surgical, damaged cornea.
Following are several instances in which I employed the Five-S system to classify corneal problems and subsequently treated patients with a variety of corneoplastique.
Cases 1 and 2: Epikeratophakia
Epikeratophakia is a refractive surgical procedure in which a lamellar disc from a donor cornea is placed over de-epithelialized host cornea and sutured into a prepared groove. The technique was popular 20 years ago for the treatment of aphakia and keratoconus at a time when intraocular lenses had not yet been approved.
I occasionally encounter patients who underwent epikeratophakia years ago and, unfortunately, suffer from inadequate visual outcomes. Corneal transplants have been shown to be effective in these patients, but it's always possible that a less invasive treatment approach would benefit a specific epikeratophakia patient.
One previous patient had undergone aphakic epikeratophakia nearly 20 years earlier and presented with a decentered, scarred epilenticle with poor vision correctable only to 20/200. Using the Five-S's for classification:
• Sight: By using a hard contact lens, the patient was able to achieve 20/25 vision.
• Site: The epilenticle was decentered.
• Scar: An opaque scar was present.
• Strength: The cornea was thick, as it was partially composed of surgically added tissue.
• Shape: The patient had irregular astigmatism with hyperopia.
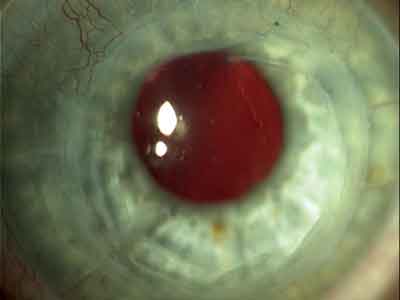
 |
| A decentered corneal lenticle is separated from the cornea 18 years post-epikeratophakia. |
Using the classification system as a guide, the plan was to first remove the epilenticle. On removing the epilenticle disc from the patient's cornea, I found that the underlying tissue was pristine. By removing the disc, I had removed the scar, corrected the center and found that the original cornea underneath had normal thickness. The surgery also addressed the shape of the cornea.
The only one of the Five-S's remaining was sight, so I performed a high-speed vitrectomy and secondary IOL placement to correct the patient's aphakia. This resulted in uncorrected vision of 20/25 in the eye. The patient was ecstatic.
Another epikeratophakia patient had a scarred myopic lenticle with pseudophakia (20/400 vision). In this case, I addressed the first four S's in the fashion described above but, since the patient was pseudophakic, instead of placing an IOL, I performed excimer laser surface ablation to address the cornea's shape. The procedure resulted in uncorrected vision of 20/30- in this eye. This second case, in my opinion, debunks the myth that you can't lift a flap after a number of years. I have lifted LASIK flaps as long as a decade after the initial surgeries.
Cases 3 and 4: LASIK Complications
Another patient was referred to me with best-corrected vision of 20/100 and an obvious corneal scar after LASIK. Using the Five-S system to classify his condition, he had central involvement and a scar, the cornea had good thickness and the shape was affected because of irregular astigmatism. With a rigid contact lens, the patient's vision improved to 20/25, and I documented his subjective response to the better vision.
In this case, I addressed his central scar and shape by performing excimer laser advanced surface ablation with mitomycin-C on the LASIK flap. This resulted in uncorrected vision of 20/15 in this eye. My goal in this instance was to clear as much of the scar as possible with my main focus being the corneal shape. My endpoint is visual acuity, even if there is a trace residual scar. It's important to remember that posterior corneal opacity is less responsible than anterior opacity for visual status.
To help understand my thought process, it's worthwhile explaining another LASIK complication case that had a similar corneal scar but also thin residual cornea and a preop vision of 20/100.
To treat this patient, I replaced the previous LASIK flap with a thicker, sutureless lamellar corneal transplant. If the transplant is thicker than
180 µm, I perform a Barraquer anti-torque, eight-bite, continuous suture. Also, remember the donor corneal lamellae will deturgesce, so account for that loss of thickness in the planning by taking a thicker lamellar flap than is removed from the recipient. In this way, you are also planning for future laser sculpting to address the cornea's shape. In this patient, this approach addressed the central site, clarity and corneal thickness. Three months later, with a potential vision test showing that 20/25 vision was possible, I proceeded with the excimer laser to address the final "S," shape, resulting in uncorrected vision of 20/20 in the eye.
In some cases, I will ablate the back of the corneal flap to address refractive error without compromising corneal integrity.2 I will also occasionally use Intacs to treat ectasia, depending on the presentation.
Cases 5 and 6
One patient I treated was a deputy sheriff. In his occupation, good vision is important but he had been made legally blind by 8 D of astigmatism that resulted after a corneal transplant. On the Five-S classification, he had a clear cornea without a scar, and the corneal thickness was fine, as well. The cornea was just thick because of the transplant. His main problem, then, was an abnormal shape resulting in irregular astigmatism. Having confirmed the posterior wound healing of the transplant, all I wanted to do was reshape the anterior cornea.
To treat him I performed planned operations in two stages, and eventually reshaped the cornea with the excimer. The patient now sees 20/25 uncorrected and has gotten back to his profession and life with renewed vigor.
Another patient was referred to me with a long-standing chemical injury that resulted in legal blindness in his left eye. He had a history of PRK and pseudophakia (barely visible through the opaque anterior cornea) prior to the accident. He had extensive conjunctival scarring, a central diffuse corneal scar and corneal pannus in two quadrants.
As stage one, I cleared the ocular surface and corneal pannus, including the superficial corneal scar, using amniotic membrane graft with glue. The patient was thrilled with both his improved appearance and also his better vision of 20/80-.
As stage two, potential vision testing with a contact lens trial showed the potential for 20/40-, and the corneal clarity had improved. Now, however, I could see that the posterior capsule was opacified. I performed a YAG-laser capsulotomy and the patient achieved a potential vision of 20/20 with a hard contact lens. I then addressed the residual corneal scar and irregular corneal surface with the excimer laser. The patient now sees 20/15 uncorrected in the eye. Obviously, as an ophthalmologist you can still see the patient's previous corneal scar through the slit lamp, and the qualitative vision isn't comparable to a postop LASIK patient. However, the fact that he's gone from legal blindness to 20/15 uncorrected using staged, topical, brief procedures rather than extensive interventional surgeries such as corneal transplant represents something of a paradigm shift in my practice and probably for other kerato-refractive practices.
Wavefront-guided surgery and technological advances continue to move us closer to our ultimate goal of "super vision," but safety must be our first responsibility along the way. Everyone talks about technology and technique, but there is one more "T" to consider—tissue. When you understand the ins and outs of the cornea, the proper selection of technology and technique will flow from that. This knowledge, combined with tools such as the Five-S classification system and corneoplastique, will let surgeons be more responsive to patients' needs and give them more options if complications arise.
Dr. Gulani is a consultant for Bausch & Lomb. He wishes to acknowledge Lee Nordan, MD, for his contributions to the article.
1. Gulani AC. LASIK Corneal Complications: A New Stratified Classification. Ophthalmology 1999;106:1457-58
2. Gulani AC. New Instrument For Revision Lamellar Refractive Surgery. J Cat Refract Surg 1998;24:595.