Combined vs. Staged Procedures
Several surgeons say they're not doing as many combined procedures as they used to, because clear-corneal phacoemulsification is very effective, and can have a modest pressure-lowering effect by itself.
"I think there's been a sea change in how surgeons approach patients with cataract and glaucoma," says Mary Fran Smith, MD, associate professor of ophthalmology at the University of Florida School of Medicine. "This is because phaco is a different animal from extracap, which involved 11-mm wounds with removal of the lens in toto. A third of these extracap cases were associated with increased pressure afterward, and in as much as half, the pressure was unchanged. This was a real point of discussion, because a even a short-lived pressure spike could snap the optic nerve.
"In these days, with phaco, you use small self-sealing incisions and a high flow of irrigation. The irrigating fluid can't go anywhere but through the trabecular meshwork because the incisions are so small when you insert the phaco probes." She says that, because of these factors, she and her colleague William Doyle, MD, have found that phaco is associated with lower intraocular pressure postop in about 90 percent of their cases. She'll also sometimes perform selective laser trabeculoplasty preop in some cases. She'll still do a combined procedure, though, for eyes with very sick-looking nerves, very high pressures and significant cataract.
Robert Fechtner, MD, director of glaucoma at the University of Medicine and Dentistry of New Jersey, doesn't think a cataract procedure alone can reliably control the pressure, but says there is often merit to staging these procedures.
"You can do a nice, uneventful clear corneal cataract operation, and, within a few months when the eye is quiet, you can do a trabeculectomy that's uninfluenced by the inflammation of cataract surgery," he says. "Trabeculectomy alone is quite likely to be more successful than doing a combined procedure." He says he'll stage the procedures in an eye in which the pressure is reasonably well-controlled and may be on one or two glaucoma medications.
For patients on multiple IOP-lowering medications, with advanced optic-nerve damage that may not tolerate a pressure spike, damage that's occurred at IOP levels that aren't very high, or moderate to advanced visual field loss on white-to-white perimetry, Dr. Fechtner will perform a combined procedure.
 |
| Diffuse filtration bleb following combined trabeculectomy with mitomycin-C/phacoemulsification surgery. James Tsai, MD |
Surgical Insights
Surgeons prefer to perform their combined procedures in different ways, with different approaches to certain aspects. Here are their thoughts on the main steps:
• Two-site procedures. Surgeons say that two-site combined surgeries, which usually involve clear-corneal cataract surgery at the temporal location and a glaucoma filtering procedure at a superior spot, are probably the most popular.
Adam Reynolds, MD, clinical assistant professor of ophthalmology at the Dean McGee Eye Institute at the University of Oklahoma, explains why.
"The more you keep the glaucoma procedure the same as it is when done on its own, the more predictable things will be," he says. "The advantage of a two-site approach is that you're not altering your glaucoma filtration technique, which you do if you perform a single-site surgery, because you'll be doing both procedures through the same incision."
In Dr. Reynolds's technique, he starts the glaucoma surgery and gets it to the point at which he applies the antimetabolite, either 5-fluorouracil or mitomycin-C. Then, he does the phaco and instills Miochol to bring down the pupil, and finally finishes the trabeculectomy.
"Some people feel pretty safe doing the phaco completely up front," explains Dr. Reynolds. "But with that there's the risk of possibly getting mitomycin in the eye, because of the incisions you've made. I was trained that it's always important not to give mitomycin the slightest chance of exposure beneath the endothelium.
"Other surgeons would argue that doing the cataract completely beforehand is better, because with the 2.5-mm incision, small paracentesis and the viscoelastic you put in the eye, there's no way mitomycin is going to get in. Done that way, it becomes more efficient and faster because you only have to change locations once during the procedure rather than twice, which involves resetting your feet and microscope."
Sacramento, Calif., surgeon Richard Lewis prefers two-site surgery, as well. "I feel as if I have more control over each of the wounds," he says. "You want the cataract wound to be non-leaking, so, even though I use a clear-corneal incision, in combined procedures I will put a suture in the wound because I don't want that wound to leak, whereas in normal cataract surgery I won't. Yet, I want the other [filtration] wound to leak, maybe not immediately, but later. I think the components of wound healing and construction are very unique, and should be separated."
Dr. Lewis wonders about the impact wound architecture could have on a one-site procedure. "I think the architecture has an impact on the surgery," he says. "I believe that when a cataract incision is under a scleral flap, there's thinner sclera there, so you don't have as much support and have more potential for wound leakage during phaco as it leaks around your phaco port. That leakage can lead to some fluctuation of your anterior chamber depth and could compromise the cataract surgery. I think the first goal of this procedure, if you're taking out a cataract, is that the patients see well afterward."
• One-site procedures. "I think the results of a one-site combined procedure can be just as good as those of a two-site," says James Tsai, MD, director of the glaucoma division and associate professor of ophthalmology at Columbia University in New York City. "I prefer one-site surgery because it's not much different from my standard trabeculectomy technique. With the two-site technique, if you perform a temporal corneal wound for the cataract incision, you will probably need to place a temporal suture to allow for ocular massage and other bleb manipulation techniques. But with a one-site approach, I feel very comfortable with performing my standard postoperative techniques, including ocular massage and laser suture lysis."
 |
| Postop day one after combined surgery. Note releasable suture at 11 o'clock. James Tsai, MD |
In Dr. Tsai's approach, he instills topical anesthesia, makes an initial fornix-based conjunctival incision approximately 1-mm posterior to the limbus, then supplements the anesthesia with a subconjunctival anesthetic injection. He then extends the fornix-based conjunctival incision for approximately two clock hours. He also cauterizes any vessels to prevent oozing. He makes a limbus-based, rectangular scleral flap (3 mm wide by 2 mm long), dissecting down to half thickness, but not really going anterior. He then applies 0.2 mg/ml of MMC (soaked in half corneal light shields) for two minutes in the subconjunctival region. He rinses off the sponges, performs his standard phaco procedure and places the lens.
After he places the lens, Dr. Tsai will leave some viscoelastic in the chamber to protect against intraoperative hypotony. He'll constrict the pupil with Miochol and use the Kelly-Descemet's punch to make the fistula, following that with a small peripheral iridectomy. He places one interrupted 10-0 nylon suture in the rectangular flap and one releasable 10-0 nylon suture with a loop in the cornea.
"What I particularly like is because I have made the fornix-based conjunctival incision 1-mm behind the limbus, I can perform a conjunctiva to conjunctiva running, intermittently interlocked closure using a 10-0 vicryl suture on a CS 160 needle." He appreciates that the one-site approach allows him to operate efficiently, which makes it possible for him to use topical/subconjunctival anesthesia in almost all of his combined cases.
|
Dr. Fechtner also performs phaco through a scleral tunnel. However, he applies his MMC after the lens is in place and the chamber is filled with viscoelastic rather than before the phacoemulsification.
"Applying the mitomycin before the phaco step, and then having the huge volume of irrigation fluid that tends to leak out of the cataract surgery wound wash over the mitomycin area doesn't give me the mitomycin effectiveness I would like," says Dr. Fechtner. After he irrigates away the mitomycin, he uses a punch to remove the posterior lip of the incision, creating the filter. Then, he removes the viscoelastic, tests for flow and closes the sclera, with several sutures for possible future suture lysis.
• Fornix- or limbus-based flaps. Surgeons have developed affinities for certain conjunctival flap incisions, based on different surgical factors that are important to them.
Dr. Tsai prefers a fornix-based conjunctival flap. "One of the reasons that surgeons perform a two-site technique is that they prefer to use a limbus-based conjunctival flap to reduce their rate of wound leaks," he says. "In my opinion, for enhanced ease when doing a one-site procedure, it's preferable to make a fornix-based conjunctival incision. However, many surgeons are concerned that if they do this they'll get a lot of leakage because they're suturing conjunctiva to limbus and cornea, which isn't a very predictable closure.
"However, I have found that if one performs a fornix-based incision slightly posterior to the limbus, leaving a 1 to 1.5 mm conjunctival skirt at the limbus, then the incision apposes nicely with a conjunctiva-conjunctiva running closure. In this manner, I get minimal risk of wound leak and a predictable closure." He says these conjunctival flaps help produce the diffuse, low-lying, less-ischemic blebs that surgeons are looking for. "Because the running closure is set about 1-mm back from the limbus, anterior fibrosis develops that's slightly posterior to the limbus, thereby directing flow from the trabeculectomy flap posteriorly," he explains.
Dr. Smith does her one-site combined surgeries using a flap that she estimates only about 5 percent of surgeons use for them: limbus-based. She says this allows her to perform postop ocular massage, which she feels is key to ensuring the success of the filter.
"With this approach, you make an incision posteriorly in the conjunctiva, then dissect your way forward, with the big wad of conjunctiva making your view, and the rest of the surgery, somewhat difficult," she says. "But, if you have enough experience, and luck, you can complete the phaco. Then, after you've finished the trabeculectomy, sutured it down and closed the conjunctiva, you have the option of doing ocular massage when the inevitable postop healing response occurs. I have yet to have one of these eyes fail."
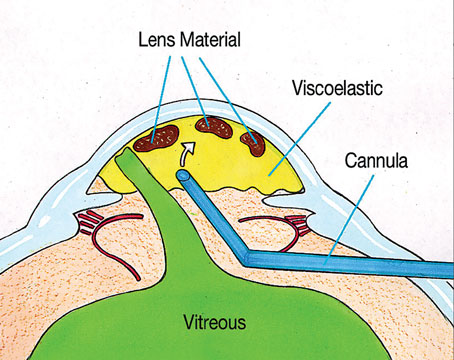
 |
| A surgeon begins converting a scleral-tunnel cataract wound into a filter. Mary Fran Smith, MD |
For his two-site procedure, Dr. Reynolds says he has always been an advocate of limbus-based flaps, but has recently begun to change his way of thinking on the subject.
"I've been studying [Moorfield's Eye Hospital surgeon] Peng Khaw's work in this area, and have realized I haven't been thinking outside the box enough to give fornix-based flaps a better chance," he says. "So, I'm in the process of converting my flap incision location, but it also involves a change in my trabeculectomy technique.
"There are subtle things you can do to automatically direct the flow posteriorly, such as using a square flap with a small ostomy, which is probably better than a triangular flap with a relatively large ostomy that's sewn tighter. It also involves not dissecting the edges of the flap right up next to the limbus. With a wider flap, you can't dissect the edges as far forward and undermine the central part of the flap forward and anteriorly, where your ostomy is, preventing the fluid from egressing anteriorly.
"The other trick is to stitch these flaps in such a way that the flow goes out the back rather than the sides," Dr. Reynolds explains. "The way to do that is, when you sew back the corners of the flap, buckle the flap slightly so it doesn't lie completely flat and creates a channel where the aqueous will go."
• Antifibrotics/special cases. Surgeons agree that, since the combined surgery involves cataract surgery in addition to a filtering procedure, there will be more anterior-chamber inflammation to deal with, which has the potential to cause the trabeculectomy to fail. To counteract this, most advocate using a bit more of an antifibrotic agent, or increasing the time of exposure.
"Every one of these combined patients deserves mitomycin-C," says Dr. Smith. "If I normally use 0.2 mg/ml for a duration dependent upon the condition of the conjunctiva, for combined procedures I'll use 0.3 mg/ml concentration and base the duration of exposure on the condition of the tissue."
There are also special cases to consider, such as high myopes.
"I'm really concerned with high myopes and their wound leakage and flat chambers," says Dr. Lewis. "In those patients, with thinner sclera, I might leave some viscoelastic in the eye, and have access to a paracentesis postop so I can reform the chamber if it becomes shallow or flat." Surgeons say they'll probably decrease the strength of their MMC application in a high myope, as well, due to thinner than normal sclera in those patients.
In the end, the surgeons to whom we spoke think the technique one uses for a combined procedure isn't necessarily right or wrong.