|
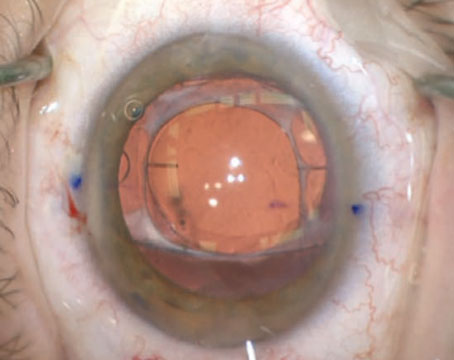
| Regular astigmatism is amenable to treatment with a toric lens. (Photo courtesy Uday Devgan, MD) |
Toric Pearls
Though toric IOLs from Alcon and Staar have been a boon to patients and surgeons, physicians say they call for a different approach to implantation that takes some getting used to.
“I think the biggest change that most cataract surgeons have to make when they begin implanting toric lenses is making sure they do the preop testing before eyedrops are placed in the eye,” says Boston surgeon Bonnie Henderson. “Traditionally, before toric lenses came out, the process would proceed like this: First, the tech would see the patient and test intraocular pressure, instill drops, etc., and then the doctor would see the patient and determine if he needed cataract surgery. If surgery was necessary, the surgeon and the staff would then get the K reading, axial length and so on. The problem with doing things this way with toric lenses is that if you try to do the biometric testing after the drops, the accuracy of the tests is thrown off because the corneas will become dry and areas will be desiccated. The measurements of corneal curvature or the topography map may not be accurate.
“Also, if the patient is a soft contact lens wearer,” Dr. Henderson continues, “the lenses must be removed for at least two weeks before the preop measurements are done, and at least three weeks prior for those who wear rigid gas permeable lenses. This is because the lenses flatten the cornea, and, even if someone comes in not wearing their lenses, the corneas may be artificially flattened, causing the Ks to be inaccurate.”
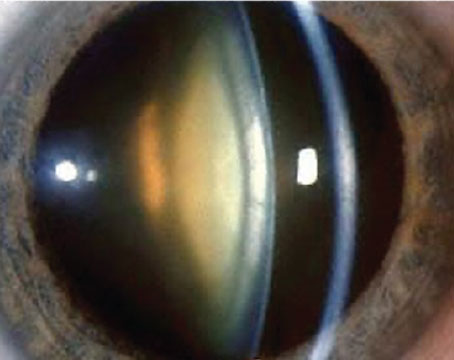
It’s also important to identify the sources of the astigmatism, to ensure that a toric lens will indeed be necessary to correct it. “You want to make sure you’re measuring the corneal astigmatism, and that you have good topography preoperatively in order to measure the magnitude and the axis of the preop astigmatism,” says Nick Mamalis, MD, of the Moran Eye Center at the University of Utah. “There have been patients in whom the refraction shows a higher amount of astigmatism than topography does, which means it’s lenticular or from another source in the eye, and you don’t want to implant a toric lens for that.”
Conversely, surgeons warn about patients who show no astigmatism on refraction, but who actually have corneal astigmatism that’s being masked by offsetting lenticular astigmatism. “Patients have been referred to me after having worn spherical spectacles for their entire lives,” says Robert Osher, MD, professor of ophthalmology at the University of Cincinnati College of Medicine. “Then, when I image them with a device such as Tracey’s iTrace, which differentiates between the various sources of astigmatism, I find 2 D of astigmatism on their cornea as well as 2 D from the lens that is neutralizing the corneal astigmatism. They’re very surprised when I tell them that they’d benefit from a toric lens to correct their astigmatism.” A good topographic map will also find corneal astigmatism in patients who have offsetting lenticular astigmatism, says Dr. Mamalis.
Surgeons also take care in marking the patient’s eye to ensure that the toric lens is properly aligned with the axis of astigmatism. “Surgeons have to make sure to mark the cornea while the patient is sitting upright,” says Dr. Henderson. “This is because some patients have a significant amount of cyclorotation when they lie down. One study found that the average positional cyclorotation is 4 degrees, though 8 percent of the study’s 240 eyes rotated by 10 degrees.1 Because the toric lens relies on accurate placement with regard to the axis of astigmatism, if patients are rotating and the surgeon incorrectly marks the eye, the surgeon would end up placing the lens on the wrong axis. And, with the toric lens, one degree of misalignment equals a decrease in astigmatic effect of 3.3 percent.
There are many ways to make these reference marks; some use handheld markers while some use high-tech approaches that capture iris or conjunctival vessel patterns in digital images. If you use a manual system as I do, after the reference marks are placed on the eye with the patient sitting up, we then lay the patient supine and I mark the steep axis of astigmatism using a bimanual system that consists of an open degree-gauge marker in one hand and a marking instrument in the other.” Dr. Osher prefers to use dot cautery to mark the astigmatic axis. “The dot will be there after you’ve performed the phaco, irrigation/aspiration and implanted the lens,” he says. “It will not have bled away, diffused or disappeared as an ink mark might.”
Technological Innovations
As Dr. Henderson noted, there are now technologically advanced ways to help get a toric lens properly positioned. Here’s a look at some devices that are either available or soon will be.
• Accutome’s Devgan Axis Marker. Developed by Los Angeles surgeon Uday Devgan, who has a financial interest, this marker mounts on the slit lamp’s tonometer housing. With the patient at the slit lamp, the surgeon dials in the axis to be marked and looks through the instrument to center the marks. The instrument has a hollow center to allow it to be centered over the pupil. “I mark the eye by inking the device,” says Dr. Devgan. “But then, after I ink it with the device, I get a disposable needle and make non-full-thickness puncture marks in the cornea.”
• Geuder Tomark. This device fits on a slit lamp and has both a degree gauge and a marker. The sur---geon sets the axis in degrees on the marker’s outside ring, and then briefly presses the Tomark against the patient’s eye to make two indentations and ink marks.
 |
Mr. Smith says Micron Imaging is currently developing an upgrade to the system that would give the surgeon the ability to lay the guidance image over an image of the patient’s eye postop in order to ensure that the lens is indeed on the correct axis “to make sure the lens hasn’t moved since surgery and was aligned properly during the surgery.”
• Carl Zeiss Meditec’s Callisto and Z-Align. The Z-Align video system is part of Carl Zeiss Meditec’s Callisto Eye digital surgical data system. After manually marking the eye, the surgeon uses a touch screen to mark the astigmatic axis on a video image of the eye, which is being filmed through the surgical microscope. The company says the system can be used with nearly any video camera that’s normally used in the operating room. The system also has an eye tracker that will ensure the axis line stays with the eye as it moves. The Callisto and Z-Align are currently only available outside the United States.
 |
Mr. Kersting says one of the benefits of the system is that it’s fully automatic, registering the eye and steep axis automatically based on keratometry and anatomical features of all types, rather than just iris features. “This is helpful because once the pupil is dilated there usually aren’t enough iris features available,” says Mr. Kersting. “Or, if it’s a special case that requires the use of iris hooks or expanders in the pupil, if you relied only on iris features you might not get a good correlation with them because they wouldn’t be in the correct locations.” He adds that since the registration image and the keratometry are done at the same time, the system avoids any problems with cyclorotation that could occur between an initial image of the patient’s eye and a later marking of it at a slit lamp.
• TrueVision Systems’ 3D guidance overlay. The TrueVision 3D Surgical system has made inroads in ophthalmology and neurosurgery as a viewing device, allowing surgeons to see their surgery on a high-definition 3D monitor rather than through the microscope. The company plans to build on the viewing system by adding a feature that lets surgeons view a toric axis overlay, too.
“Basically, the system uses a 3D camera at the slit lamp to capture a preoperative 3D image,” explains David Friess, OD, TrueVision’s director of clinical and regulatory affairs. “And that image is registered to the live 3D view the surgeon sees using the 3D flat screen. The system then tracks the registered images, with the toric alignment overlay appearing on the tracked image based on axis information entered preoperatively. The surgeon can then manipulate the lens and align it according to the marks on the lens and the graphical overlay.” The toric overlay system has been submitted to the Food and Drug Administration and the company is awaiting 510(k) approval for it.
• WaveTec ORange. The ORange system is an intraoperative wavefront aberrometer that a surgeon can use to get feedback on the patient’s refractive error during surgery to help guide lens implantation. It consists of an imaging unit attached to the surgical microscope and connected to a computer with a touch-screen monitor. Toric lens implantation is one of the situations the system was designed for, since the surgeon can get an idea of how accurate his lens placement is as he’s doing it.
“When you’re implanting toric lenses, you try to be as accurate as you can be, but there is some inherent variability with ink marking devices,” says Farrell Tyson, MD, an ORange user from Cape Coral, Fla. “And all that preop data is based on the preoperative cornea. But, when you make your cataract incision, you’ve changed the eye’s keratometry. Also, the incision will induce a different amount of astigmatism depending upon whether it’s a steep or a flat eye. So although your average induced cylinder is
0.2 D, it will be different in a flat or a steep eye.
“ORange allows you to get a true reading of the corneal astigmatism, not only on the front surface but also how much the posterior cornea is inducing,” Dr. Tyson continues. “Sometimes, with corneas that have a very low amount of cylinder in which you’d use, say, an Alcon T3 lens, I’m finding that in 5 percent of these cases I don’t have to implant a toric lens at all, because on the table I’m reading with the ORange that there’s no astigmatism in the system, even though my corneal topography clearly showed there was anterior corneal astigmatism. On the other hand, the toric calculators for both Alcon and Staar are very conservative. I’m finding that about a third of the time on the table I’m actually using a higher cylinder power lens than the calculators predicted because the ORange showed that the true corneal astigmatism was actually higher and a higher cylindrical powered lens would get me more correction.”
Dr. Tyson says the system also aids with getting an accurate axis alignment. After taking an aphakic reading to get an idea of the proper lens power and axis, Dr. Tyson injects the lens and has the patient look at a fixation light and takes a series of aberrometry readings. “The system will, in effect, say, ‘You’re pretty good, but maybe you should rotate it clockwise or counterclockwise to get the ideal position,’ ” says Dr. Tyson. “Then I rotate it and take another reading, which might show that I have to nudge it a little more. Then I take another reading and it confirms that I’ve got it. I can watch the cylinder slowly track down on the screen.” The ORange system costs $30,000, plus $3,000 per month for unlimited usage.
 |
• Clarity Medical System’s HOLOS. This is an intraoperative wavefront system in development that aims to differentiate itself from other technology based on the rapidity of its measurements. “The HOLOS intraoperative aberrometer is designed for use during cataract surgery,” says Barry Linder, MD, Clarity Medical System’s chief medical officer. “It will be attached to the surgical microscope. The key differentiators between this system and others is that it’s truly real-time, continuous data acquisition and display. There’s no concept of having to acquire the data and then process, analyze and display it before making a decision based on it. It’s there on a real-time basis.”
In addition to confirming that a target refraction has been achieved during cataract surgery, Dr. Linder says another major application will be the manipulation and placement of toric IOLs. “Specifically, it can assist in the placement of the axis of the toric IOL and/or assist with identifying the axis of astigmatism and treating it with whatever form of corneal incision the surgeon wants to use,” he explains. “The surgeon will have real-time data to identify the axis without having to mark it. This is better than using a mark be--cause he will have the data.”
The device is currently being studied at three clinical sites and has been used in more than 50 patients with a variety of needs, from toric to multifocal IOLs. Dr. Linder says the data is still being analyzed, but he says he can confirm that the surgeons “were able to see very clearly when the astigmatism was neutralized” during surgery.
Dr. Osher is excited about the potential for toric lenses and the technology that helps surgeons implant them, and says it’s imperative for surgeons to overcome any hesitancy about adjusting their surgical technique to use torics. “Unless you move to toric lenses, you can’t go to the next step,” he says. “And there are a lot of exciting next steps down the road.”
1. Swami AU, Steinert RF, Osborne WE, White AA. Rotational malposition during laser in situ keratomileusis. Am J Ophthalmol 2002;133:561–562.