The use of toric intraocular lenses in cataract surgery is steadily increasing, and as happens with any new technology, plenty of “tricks of the trade” are still being discovered. (For example, a study just published in October found that if you can’t exactly match the cylinder-correcting power of the toric IOL to the corneal astigmatism, better outcomes are achieved by using a lower rather than higher cylinder value.1)
Here, seven experienced surgeons share their insights into every aspect of implanting toric lenses, from measuring, marking and patient management to implanting the lenses on the correct axis and correcting any problems that turn up postop.
Measuring and Marking
Possibly the most crucial part of the procedure is determining the axis of astigmatism as accurately as possible. This is scarcely a foolproof process, but a number of strategies can help:
|
Stephen S. Lane, MD, medical director at Associated Eye Care in St. Paul, Minn., and adjunct clinical professor of ophthalmology at the University of Minnesota, notes that his team takes as many as five different measurements to determine the magnitude and axis of the astigmatism. “We use manual and automated keratometry and topography, including measuring with the Lenstar and IOLMaster,” he says.
• Remember that not all K-readings are created equal. John Berdahl, MD, corneal, refractive and glaucoma surgeon at Vance Thompson Vision in Sioux Falls, S.D., and assistant clinical professor at the University of South Dakota, agrees that using multiple sources for your measurements is crucial, but emphasizes that topography is especially important. “The tricky part with toric IOLs is getting reliable keratometry measurements,” he says. “Anterior topographers do the best job of quantifying the axis and magnitude of anterior corneal astigmatism.”
“The IOLMaster is a great product, but may not be the best for identifying the exact orientation of the axis of astigmatism,” notes Dr. Davison. “It’s great for determining the average K-value and the power of the implant, but you shouldn’t use the IOLMaster for determining the axis. That’s one reason Alcon’s instructions say to use manual keratometry for that purpose.”
Dr. Berdahl agrees. “The IOLMaster takes six data readings and extrapolates from that data,” he says. “It wasn’t designed to provide incredibly accurate astigmatism measurements. So you should probably put a little less weight on that device than on something like a topography unit, which will give you much more precise astigmatism readings.”
• Be wary of disagreement between measuring instruments. “Part of the goal of taking multiple readings with different instruments is to see whether all of the readings are within 10 degrees of each other,” says Dr. Davison. “I like to see whether the manual Ks are close to the Pentacam Ks. If they’re not within 10 degrees, we go back and take the Pentacam picture again and do the manual Ks again. We may end up having to do this on a different day, because by the time I see everything the patients usually have had drops in their eyes. But it’s really important to get the axis right.”
“If there are discrepancies between the readings, I tend to rely on manual or automated keratometry for the magnitude of the astigmatism, and topography for the axis,” says Dr. Lane. “Usually three or four of the five measurements will agree. If only one disagrees, I treat it as an outlier and exclude it.”
“If the measurements we get with different instruments are out of agreement by more than 10 degrees, I start to be leery about using a toric lens, especially if the patient has a large amount of astigmatism,” says Dr. Berdahl. “If the alignment of a toric lens is off by 10 degrees, it loses 30 percent of its effect. That’s not a big deal with low-power toric lenses, but in a large diopter lens like a T-9, that’s almost 1.5 D of cylinder.”
• Use the most comprehensive topographic algorithm. David F. Chang, MD, clinical professor at the University of California, San Francisco, and in private practice in Los Altos, Calif., notes that he uses the topographic function that computes the astigmatic axis and magnitude from the entire area within the 3-mm optical zone, rather than the function that uses the simK measurements taken only at the edge of the optical zone. “Looking only at the keratometric points on the edge of the 3-mm optical zone might cause you to underestimate corneal toricity that is greater closer to the visual axis,” he explains.
|
• Consider manually checking the Pentacam numbers for further confirmation. “I learned this strategy from Warren Hill,” explains Dr. Davison. “He looks at the Pentacam numbers, but he also puts the Pentacam picture up and draws a line through the picture identifying the axis based on what he sees, to make sure it’s close to what the Pentacam’s numbers say.”
Pitfalls to Avoid
Many factors can interfere with an accurate measurement. A few to watch out for:
• Mark the eye while the patient is upright. “If you don’t, the eye may rotate when the patient lies down, and you’ll end up not aligning the lens to the intended axis,” says Dr. Berdahl.
• Be on the lookout for dry eye. “Dry eye can alter the keratometry value,” notes Dr. Berdahl. “Usually you can see on topography that the corneal surface isn’t pristine, and there are plenty of other clues that the ocular surface isn’t as stable as it should be. For example, if a person is blinking a lot and having a hard time when you do the manifest refraction, that a clue. If there’s a difference between your IOLMaster Ks and your topography Ks, that’s a clue. We need to be diligent about investigating these signs to avoid ending up placing the toric lens on the wrong axis.”
• Ask whether the patient wears contact lenses. Dr. Davison notes that a patient may wear contact lenses part-time and neglect to mention it. “Contact lenses change the shape of the corneal surface,” he points out. “When a cataract patient comes in, you may not be thinking about contact lenses as you would with a LASIK patient. But if you don’t ask about contact lenses, you might proceed and get the wrong numbers, leading to a poor result because the cornea was deformed from the contact lens wear. So be sure to ask.”
• Make sure your technicians have the patient’s head aligned correctly when they record the topography or keratometry. “After identifying the axis for the toric IOL from our keratometry or topography, we take a lot of effort to properly mark the axis prior to surgery,” says Dr. Chang. “Typically, we sit the patient upright and make ink marks denoting a reference such as the 180-degree axis. However, we’re trusting that the patient’s head was properly aligned when our technicians recorded the topography or keratometry. This is another potential source of error.”
• Even if you use advanced intraoperative technology, take preop measurements. Dr. Lane uses WaveTec’s ORange system, as well as other high-tech systems like the Surgery Guidance System from SensoMotoric Instruments in Germany, which takes a preop photograph of the eye and then overlays a digital reticle during surgery that moves with the eye. Nevertheless, he says he still takes preop measurements in the traditional way. “In theory it isn’t necessary,” he notes, “but I have to be prepared to finish the case if the power goes out or an instrument suddenly fails to work. Additionally, when the measurement from the intraoperative instruments agrees with the preoperative measurements it’s very reassuring that we’ve chosen the proper IOL.”
• Remember that the spherical component is important, too. “Even if you place the correct lens exactly on-axis, missing the spherical component will produce a poor outcome,” says Dr. Davison. “Let’s say you have a patient with a T-7 lens who starts off with 4 D of astigmatism. If you get it down to 0.25 D, that’s great—unless the final spherical equivalent is -0.75 D.
In that case, the patient still won’t see very well at distance.”
• Make it your goal to minimize all variables. Dr. Davison notes that while a single variable being slightly off might not have a serious impact on the visual outcome, multiple variables being slightly off all in the same direction could add up to trouble. “Let’s say you had a poor K-reading from your technician,” he says. “Then suppose you had a poor reference mark because the patient’s head was tilted. Then let’s suppose your axis marker was slightly bent, or you didn’t have your circular degree marker in the center of the eye. Then let’s say you put the lens in and it wasn’t quite perfect because of parallax; the eye wasn’t looking exactly at the microscope filament and it was off-center a little bit.
“If you take all those errors and add them up, that’s a lot of opportunity for things to be off,” he says. “In some cases, those kinds of errors might cancel each other out. But if they all happen to shift in the same direction, the cumulative effect could result in a substantial error in your placement.”
• Make sure patient expectations are reasonable. “We make sure our patients understand that with toric lenses—and even with monofocal lenses—we try to get a perfect result, but we hardly ever hit the center of the bull’s-eye,” says Dr. Davison. “Even with all of these technologies, these are still imperfect procedures. So, our focus is on getting as close to perfect as possible. We even put that in the consent form.”
Is This Eye a Good Candidate?
When an eye is not average in some respect, a toric IOL could be contraindicated or require special consideration.
• If you choose to use a toric when a topographic bow tie is regular but asymmetric, warn the patient that the correction won’t be perfect. “In this situation you’re going to get some correction of the astigmatism, but because of the asymmetry the result may not be perfect,” says Dr. Davison. “Unfortunately, patients are expecting perfection more and more, even if you don’t charge them very much.”
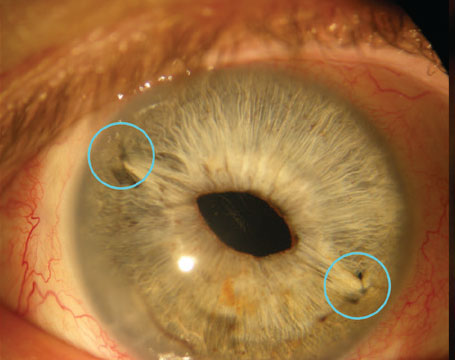
• Think twice if a patient has corneal anterior basement membrane dystrophy. “These patients can have variable vision and variable astigmatic axes,” notes Dr. Davison. (See example, facing page.) “They’re not only irregular but asymmetric as well. That’s a problem you can’t make better with a toric IOL.”
Dr. Berdahl notes that in some cases, however, a toric lens might be a worthwhile option. “If the anterior topography looks good, even though the patient has ABMD, I’d consider a toric lens,” he says. “If the anterior topography is irregular, then I’d do a PTK first to smooth it out.”
Dr. Davison notes that if the patient has a substantial toric surface underneath the corneal anterior basement membrane dystrophy, he might consider a toric. “A toric might actually be able to make the patient’s vision a little bit better,” he adds. “But I’ve spent half an hour talking to patients like this, and they still don’t appreciate that their result would have been worse without the toric lens. All they care about is whether they see well; if they don’t see well, they don’t care why—especially when they’ve paid extra money. So it’s best not to promise something that you won’t be able to deliver. For that reason, I’m not likely to recommend the toric for one of these patients, unless he really, really understands the situation.”
• If the patient has keratoconus, consider waiting for cross-linking availability. “I’m worried that the keratoconus will progress,” says Dr. Berdahl. “I’d prefer to cross-link the cornea first to get it stabilized. Without that, the astigmatism could change, or the patient could end up needing a corneal transplant. If he does, you’ll be doing a corneal transplant on top of a lens that has astigmatic correction built in, and things will get complex. I would consider implanting a toric in specific cases, but I’d prefer to do corneal cross-linking first. At this point, it looks like cross-linking will be approved in the United States soon, so I’d advise the patient to wait for that.”
Choosing the Lens
Power and axis aren’t the only considerations to weigh when making your final lens choice.
• Consider slightly undercorrecting with-the-rule keratometric astigmatism and fully correcting—or slightly overcorrecting—against-the-rule keratometric astigmatism. “We’re not measuring posterior corneal astigmatism, which probably accounts for the astigmatic discordance between the pseudophakic keratometry and refraction that we often see,” notes Dr. Chang. “Typically, in our cataract population, posterior corneal astigmatism adds against-the-rule cylinder. This would explain why many pseudophakic patients with 0.75 D of with-the-rule cylinder have no astigmatism in their refraction, and why some patients with spherical keratometry have 1 D of against-the-rule astigmatism in their refraction.
“For this reason, with toric IOLs I slightly undercorrect with-the-rule keratometric astigmatism and fully correct, or slightly overcorrect, against-the-rule keratometric astigmatism,” he says. “For example, if the patient has 1.75 D of with-the-rule astigmatism on keratometry, I’d implant a T3 Acrysof toric, but for 1.75 D against-the-rule, I’d probably use a T5. We definitely don’t want to flip the axis with our toric IOL.”
• Factor in lens asphericity when dealing with patients who’ve had hyperopic LASIK. “Surgeons are careful about using the Alcon toric IOL in patients who’ve had hyperopic LASIK because the Alcon torics introduce negative spherical aberration to compensate for the positive spherical aberration of the normal cornea,” explains Dr. Davison. “Hyperopic LASIK also introduces negative spherical aberration, so using the Alcon toric adds the two negative asphericities together, creating a greater negative spherical aberration than would otherwise be intended.
“However, if you don’t use the toric IOL in that situation, you’ll be leaving the patient with the far more significant lower-order astigmatism aberration,” he continues. “That residual will be a lot more obvious to the patient than the less-significant residual higher-order spherical aberration. In general, I think it’s more important to fix the lower-order aberrations than the higher, so if someone has had hyperopic LASIK but has substantial keratometric astigmatism, I’d offer him a toric lens because his uncorrected vision will be much improved with the astigmatism corrected.”
• Know how much surgically induced astigmatism you’re creating. Dr. Berdahl notes that having accurate data about this can make a difference in your outcomes. “The bigger the incision you use, and the more centrally located that incision, the more astigmatism it will induce,” he points out. “That may alter your surgical plan, and perhaps the outcome.” (All of the manufacturers’ calculators ask the surgeon to enter the expected amount of surgically induced astigmatism.)
|
In the OR
Placing the toric lens correctly can be as challenging as measuring the axis. These strategies can help:
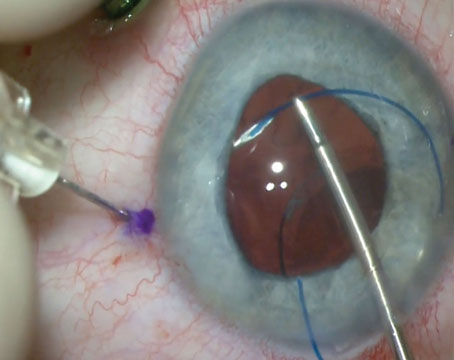
• Mark the axis of astigmatism twice; once in the exam room, and again in the OR prior to surgery using a surgical keratometer. “This is a simple way to ensure the accuracy of your reference marks,” says Dr. Gills.
Dr. Davison agrees. Preop, he prefers to simply mark the 6 o’clock axis at the limbus. “Once in surgery, I use a two-part axis determiner to place the astigmatic axis at the correct orientation,” he says. “I also reinforce the marks using a Weck-Cel sponge that I mark with ink, so the marks don’t fade away during the surgery.”
• Consider using bimanual surgery. “When implanting a toric lens, we maintain the anterior chamber with an irrigation cannula through one paracentesis and position the lens with a hook through the other paracentesis,” says Dr Lane. “There are other approaches favored by different surgeons, such as positioning with one hand using the irrigation/aspiration tip. But I find this method to be the fastest, easiest and least invasive way to do it.”
• Try alternate methods for locating the axis. Hyo-Myung Kim, MD, PhD, at the Korea University College of Medicine in Seoul has developed a method for identifying the axis for toric IOL implantation on the eye that requires no special instrumentation. Dr. Kim takes a photograph of the anterior segment; he uses the photograph to identify the desired axis marking points, as well as nearby conjunctival blood vessels that can be used as reference points. He then calculates the precise distance from the reference points to the axis marking points. Once in the OR, he uses calipers to locate the axis marking points on the eye relative to the reference vessels.
In a recent study involving 40 eyes of 20 patients, researchers compared Dr. Kim’s method to two conventional techniques in which the patient was marked while seated at the surgical table or in front of a slit lamp. Dr. Kim’s method was more accurate than either conventional method by a small but statistically significant amount.2
“This approach has several advantages,” says Dr. Kim. “We don’t need any special instruments to mark the axis, and we don’t have to spend time marking the eye before surgery. Taking the photograph is a very simple process. And, our method appears to give us more accurate results.” (Dr. Kim notes, however, that mydriatics mixed with vessel constrictors can make identification of the reference vessels more difficult. He suggests preoperatively selecting an additional landmark near the limbus as an alternative reference point in case any problem arises.)
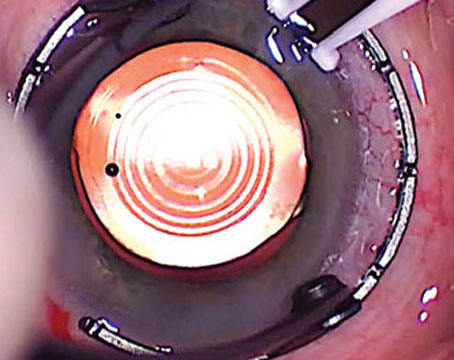
• When initially implanting the lens, leave it about 20 degrees shy of the final orientation. This will allow you to very carefully move it to its precise alignment as a separate step, say our surgeons.
• Try to rotate the lens after insertion to identify potential postop rotation problems. “A technique I follow is to try to rotate the lens both clockwise and counterclockwise immediately after insertion,” says Catherine T. Fitzmorris, MD, who practices at Gulf South Eye Associates in Metairie, La. “This helps me identify cases which are more likely to rotate postoperatively.”
• Be sure to remove all of the viscoelastic from behind the lens. “This enables the lens to tack itself down to the capsular bag, making it less likely to rotate,” says Dr. Berdahl.
• Take special care with long eyes receiving low-dioptric-powered lenses, especially with vertical orientation. In this situation, Dr. Davison notes that postop rotation is more likely because the lens is standing on one haptic. “In that situation, gravity wants to rotate the lens so it’s not standing on a single point,” he explains. “It’s inherently more stable when it’s supported by two horizontal points.
“A few years ago I published a paper with Art Weinstein,” he continues.3 “We found that for powers from 6 to 10.5 D, 3.4 percent of the lenses fell off the vertical axis and rotated significantly; 1.4 percent of 11 to 15.5 D lenses, and 0.5 percent of 16 to 20.5 D
lenses also rotated significantly off their intended axis. In contrast, lenses with a power of 21 D or higher didn’t rotate at all. So when the eye is really long, postoperative rotation is more of a concern, especially when the lens is oriented vertically.”
To proactively prevent that rotation, Dr. Davison suggests two strategies. “First, consider making the standard 2.4-mm-width incision’s shelf a little longer,” he says. “Usually my shelf is about 1.7 mm; in this situation I might make it almost 2 mm. I want to make sure that I can stromal hydrate the incision without overinflating the eye and the capsular bag. Second, make sure you remove all viscoelastic from in front of and behind the lens. If you leave any viscoelastic and you overinflate the eye, the lens is more likely to rotate afterwards, especially in really long eyes when the lens is placed vertically.”
• In the case of a radial capsule tear, you can probably leave the lens in. “Many surgeons believe that an anterior radial tear is a contraindication for a toric lens, so if a tear occurs, they might not implant one; or, if implanted already they might try to remove the lens and replace it with something else,” says Dr. Davison. “Even if a posterior tear is discovered after the lens is in, you don’t have to remove it; you can leave it in as long as you orient it properly and capture the optic anterior to the anterior capsule remnant created by an intact capsulorhexis. In fact, if you try to take it out, you’re probably going to make the situation worse. You’ll create more tears or other problems. Then where do you put the next lens? Even if you’re forced to leave the lens with an imperfect alignment, leaving it may still be better than trying to take it out. You can correct some residual problems from an imperfect alignment with LASIK—assuming that the cornea has enough tissue.”
|
Dr. Berdahl adds that this technology is also helpful when implanting a Crystalens. “Sometimes the Crystalens has a tendency to vault a little anteriorly,” he says. “If you have a more myopic reading with the ORange device after implanting the lens, you can go back in and tap the lens posteriorly. I’m now getting much more appropriate and consistent results with the Crystalens.”
• In some situations a capsular tension ring may help. “If the patient is a very high myope with a large capsular bag, I’ll occasionally use a capsular tension ring to try to prevent any lens rotation and make sure the lens is in the best possible location,” says Dr. Berdahl. “I haven’t seen clinical data proving that this helps, but anecdotal reports suggest that it does.”
• Triple-check everything at the end of surgery. “Once the eye is returned to normal pressure, it’s important to confirm that everything is correct with at least two other people who are present in the OR,” says Dr. Davison. “Everybody looks at the paper and the video screen one last time. We make sure we used the right lens. And it’s especially important to confirm the axis, because believe it or not, you can get tired or mixed up and put the lens on the wrong axis. We sometimes even get the axis marker out again to inspect, just to make sure. If you triple-check and confirm with others, it’s almost always fine.”
Resolving Problems Postop
Lens rotation after surgery only happens in a small percentage of cases, but when it does, these steps can help ensure an appropriate remedy.
• If the postop refraction isn’t perfect, use trial lenses and a lensometer to determine whether lens rotation is to blame. “With the use of toric IOLs that correct large amounts of astigmatism, even a small amount of rotation can cause an unusual refraction,” notes Dr. Fitzmorris. “One way to verify that the refraction is secondary to rotation of the lens is to use trial lenses and an auto lensometer.
“For example,” she continues, “suppose you were trying to correct 4 D of cylinder at 90 degrees. Take a +4-D lens and place it on the automatic lensometer, aligned at the 90-degree mark. Now, suppose the toric lens you implanted actually oriented at 95 degrees, postop. Take a -4 D cylindrical lens from the trial lens set and orient it at the 95 degree meridian over the +4-D lens already on the automatic lensometer. The resulting neutralization of the two lenses will tell you what your postop refraction should have been as a result of the rotation.
“You can compare this reading to your actual postop refraction,” she concludes. “If it matches, the lens rotation is the source of the imperfect outcome. If not, something else is amiss, and an IOL exchange may be necessary.”
• If the eye has residual astigmatism postop, consult the calculator at
astigmatismfix.com for advice on the best way to proceed. Use of this calculator, created by Dr. Berdahl, is free. “You can put a lens in exactly where you want it to be but have residual astigmatism because of posterior corneal curvature, or because you have more surgically induced astigmatism than you expected, or because the preop Ks weren’t good enough,” explains Dr. Berdahl. “What should you do? Our calculator takes the patient’s manifest refraction and the current lens and location and tells you how much effect rotating the lens will have. This will give you a good sense of whether it’s worth it to go back in and rotate the lens or not.”
• If you have to rotate a misaligned implant, you don’t need to mark the patient preoperatively. “Make a note of the rotation axis at the slit lamp and use that exact axis as a reference point intraoperatively,” advises Dr. Fitzmorris.
|
An Option Worth Offering
“Toric intraocular lenses are a fabulous technology,” says Dr. Davison. “It amazes me that people are still reluctant to use it. I think they may have had negative experiences with multifocal lenses, which are much more finicky and require everything else to be perfect to achieve good results. With toric lenses, if you simply follow the cookbook and do the right thing, you’re going to get good results and have happy patients.”
Dr. Davison is a paid consultant for Alcon; Dr. Lane is a consultant for SMI in Germany, Alcon and WaveTec Vision. Dr. Chang is a consultant for Alcon; his fees are donated to the Himalayan Cataract Project and Project Vision. Drs. Berdahl, Gills and Fitzmorris have no financial ties to any technology discussed.
1. Felipe A, Artigas JM, Díez-Ajenjo A, et al. Residual astigmatism produced by toric intraocular lens rotation. Journal of Cataract & Refractive Surgery 2001;37:10:1895-1901
2. Cha D, Kang SY, Kim SH, Song JS, Kim HM. New axis-marking method for a toric intraocular lens: mapping method. J Refract Surg. 2011;27:5:375-9.
3. Davison JA, Weinstein AJ. Three strategies for reorienting AcrySof toric IOLs. Cataract & Refractive Surgery Today 2010;10:1-4.
4. Visser N, Berendschot TJM, Bauer NJC, et al. Accuracy of toric intraocular lens implantation in cataract and refractive surgery. J Cataract Refract Surg 2011; 37:1394-1402.