A 66-year-old male presented to the Wills Eye Hospital Cornea Service with a complaint of two years of worsening “dark spots” on his sclera and decreased vision in his left eye, along with chronic irritation and intermittent pain in both eyes.
Four years prior to presentation, the patient had undergone an “eye-whitening procedure” due to displeasure in the cosmetic appearance of his eyes, with a goal of correcting the chronic hyperemia and injection of the conjunctiva in both eyes. Over the past two years, he has required multiple additional procedures including Tutoplast graft and an amniotic membrane graft on the left eye. At the time of presentation to Wills Eye he was on prednisolone acetate 1% eye drops four times per day in the left eye.
Medical History
The patient’s past medical history was significant for hypertension, asthma and a five-year smoking history. The patient had an ocular history of cataract extraction with intraocular lens implantation in both eyes in addition to the procedures previously discussed. Medications included aspirin, amlodipine, enalapril and a montelukast inhaler. Social history and family history were unremarkable. Allergies included penicillin G and neomycin.
Examination
The patient’s uncorrected visual acuity was 20/20 in the right eye and 20/400 in the left eye, with pinhole improvement to 20/200. Pupils were equal, round and reactive to light, and confrontational visual fields were full to finger counting. Motility was full in both eyes. His intraocular pressure was measured at 16 and 9 mmHg in right and left eyes respectively. Mild blepharitis was present bilaterally. Anterior segment examination of the right eye revealed a calcified plaque with overlying epithelial defect nasally, and areas of absent conjunctival vessels. Remaining conjunctival vessels were engorged. The left eye contained large areas of scleral thinning with uveal show, absent conjunctival and scleral vessels, and a scleral patch graft overlying the nasal sclera. No epithelial defect was present in the left eye on presentation. Three exposed sutures were present around the scleral patch graft. Trace cell was seen in the anterior chamber of the left eye. Dense inferior superficial punctate keratopathy was found in both eyes, worse in the left. The remainder of the anterior and posterior segment examinations was significant only for multifocal posterior chamber intraocular lenses in both eyes.
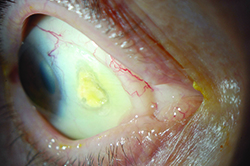 |  | 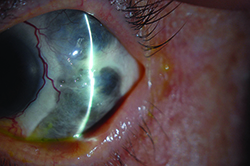 | ||
| Figure 1. Slit-lamp photo of the right eye, showing a calcified scleral plaque with overlying epithelial defect nasally. | Figure 2. The left eye shows Tutoplast graft nasally with exposed sutures, with adjacent areas of scleral thinning. | Figure 3. Slit-lamp photograph of the left eye showing severe scleral thinning temporally. |
Please click this link for diagnosis, workup, treatment and discussion.



