Define the Problem
Before you attack the astigmatism, surgeons say it’s important to find out the exact nature of the cylinder first. Also, don’t proceed with corrective refractive surgery until the sutures are out and the vision has proven to be stable.
“Is the astigmatism the result of the sutures being strong in one section or has the graft slipped in another area?” asks London surgeon Sheraz Daya. “If it’s slipped, then that needs to be fixed first. This is because, if you decide to do laser surgery, invariably, the area that’s slipped is the area in which you’re going to have to do laser to reshape it by doing a lift. That could be a problem, because it’s probably a weak spot in terms of how the graft has adhered. If you start thinning that area out further, it will keep lifting off and you can get ectasia in that area.
 |
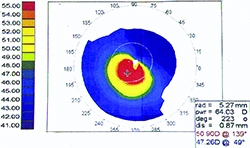 |
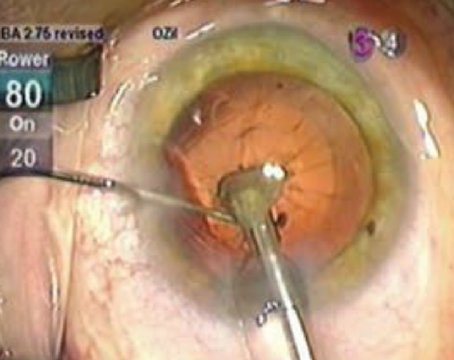
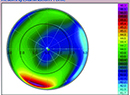
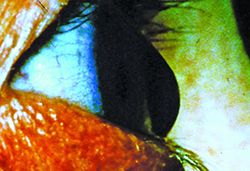
| Some surgeons say patients who have undergone PK for keratoconus (top) or ectasia (bottom) may do better with a PRK for their postop astigmatism. |
The Excimer Approach
Surgeons say PRK or LASIK can be helpful in many patients, even if it only “debulks” their astigmatism down to a normal level.
Majid Moshirfar, MD, co-director of the cornea and refractive surgery division and professor of ophthalmology at the University of California, San Francisco Medical Center, says he alters his approach based on the level of astigmatism. For high astigmatism post-PK, in the range of 8 to 12 D or more, he will consider performing a wedge resection and placing compression sutures. “But for patients with lower levels of astigmatism, I think an ablative procedure is a good option,” he says. “With LASIK, we now have the ability to make flaps inside the diameter of the donor graft, a capability we didn’t have with the microkeratome,” he says. “Now, we make a 7.3- to 7.5-mm flap inside the donor. To perform LASIK in such a patient, I’ll usually mark the donor-host interface so I know where the edge of it is. Then I center the procedure not necessarily on the apex of the cornea or the center of the pupil. Often it’s the center of the donor. Then I dock the femtosecond laser and program a very thin flap located within the graft. We’re very happy with the results from this.”
If the surgeon chooses to go the surface-ablation route, surgeons say to be sure to use mitomycin-C in these patients. “You need to use mitomycin-C in the post-PK patient undergoing PRK because he’s at a higher risk for haze and scar formation,” says Charleston, W.V., corneal specialist Heather Skeens. “Also, they’re at risk for regression of the treatment, so the mitomycin is critical. The other aspect that’s important is to note that the topographic astigmatism and the astigmatism in the refraction are often different. If you treat the patient based on the refraction only, you will usually end up with an undercorrection. So, take into account the topographic astigmatism, because it will usually be higher, and understand that you may need to fudge a little toward the topographic astigmatism when planning the treatment.” In her PRK protocol, Dr. Skeens debrides the epithelium with alcohol in a corneal well for 20 seconds, with a treatment zone of about 6 mm. For the mitomycin application, she soaks a corneal pledget in 0.02% mitomycin-C and then applies it to the cornea for 20 seconds. She then removes the pledget and rinses the eye with a bottle of balanced salt solution.
In terms of the limits of PRK and LASIK, surgeons say you can usually correct, at most, 5 to 6 D. However, they’re quick to add that going from something like 8 D down to 2 D can make a big difference for these patients. “Even though we’d like to, we don’t often get 20/20 vision in these patients,” says Dr. Daya. “There are too many variables involved. But if you can reduce the refractive error to a low level where they can get into thin spectacles, that’s a success. You also want to make sure that they stay stable.”
Dr. Skeens says one of the biggest limitations is that these laser interventions aren’t usually covered by insurance. “The patient’s physician can send a letter to the insurance company to try to get preapproval to get it covered,” she says. “Initially, the physician has to demonstrate that the patient either doesn’t do well with a hard contact lens, or can’t put the contact lens in his eye because of dexterity issues. You also have to demonstrate that the rest of the eye is healthy, the retina’s healthy, et cetera, and that there will be a positive change in vision. Even with these being satisfied, it’s hard to get an insurance company to cover it, and often ends up being a cash-pay procedure.”
The Femtosecond Alternative
Surgeons are getting more comfortable with nomograms for corneal incisions created by a femtosecond laser, and say these can be a good option in certain post-PK patients.
“For levels of astigmatism in the 6- to 8-D range, where the myopia component is equivalent or less than the astigmatism, I think the excimer laser doesn’t give that good of a result,” says Dr. Moshirfar. “This is because at that level of corneal astigmatism, in most cases, the irregularity and non-orthogonal nature of the astigmatism is such that ablative procedures won’t be good enough. For this middle range of astigmatism—greater than 4 D but not more than 8 D—I think femtosecond relaxing incisions can be very useful to the surgeon. The key with these incisions is that you need to know how to place them correctly. You can’t make them concentric with respect to the limbus or to the graft. You need to place them relative to the corneal apex. For these cases, I determine the steep axis, then mark the apex of the cornea with a marking pen. I then dock the cornea with the femtosecond laser platform, then place the arcuate incisions. I determine the number of degrees for the incisions based on the anterior keratometry of the topography. I usually bring these incisions all the way to the epithelium so that, later on, I can go in with my Colibri forceps and open them. I don’t usually open the incisions in the OR; instead I will wait a day or two, see the patients in the clinic and decide if opening them is necessary. Ninety-nine percent of the time, I open them.”
Dr. Daya says the post-PK patient is one instance where intrastromal femtosecond incisions can actually have a significant effect. “If there’s not that much fibrosis in the graft-host interface, I’ll do one clock hour per diopter,” he says. “So, for 6 D, it will be two quadrants of three clock hours—that’s the maximum incision size and number you can do on the hardware. However, in these corneas you will get more than 1 D per clock hour; because when you’re in the middle of the cornea or in the graft, there are no vessels, the wound healing is poor and the magnitude of effect is quite high. Often, it doesn’t look like it’s had much of an effect on the first day. But wait a month and it will have changed a lot.” REVIEW