Surgeons on our National Panel still view custom LASIK as their go-to procedure for most of their refractive surgery patients. Most wish they could go to it more often, with 73 percent saying their refractive surgical volume has either decreased (33 percent) or remained flat when compared to last year’s numbers. There is some optimism, however, in the realm of ectasia and keratoconus treatment, with most of the surgeons saying they’re very interested in performing corneal cross-linking if it ever arrives in the United States.
Surgeons’ preferred procedures and their treatment patterns are some of the topics covered in this month’s National Panel Report on refractive surgery. For this installment of the survey, 27 surgeons, or 5 percent of the 500-surgeon sample, responded.
LASIK Update
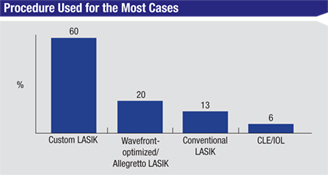
Surgeons say that when it comes to the procedure that they choose for the majority of their cases, custom LASIK gets the nod, being chosen by 60 percent of the respondents.
Wavefront-optimized LASIK, the kind performed by Alcon/WaveLight’s Allegretto excimer laser, is the next most popular option, preferred by 20 percent of the respondents. Thirteen percent like conventional LASIK and 6 percent say they use clear-lens extraction/presbyopic lens implantation the most. “Custom LASIK has the least risk and offers good outcomes,” says a surgeon from Utah. A surgeon from Illinois agrees, saying, “Custom has the best vision, excellent safety and long-term effectiveness.” Greensboro, N.C., surgeon Karl Stonecipher says he uses the Allegretto for about 70 percent of his cases. “We’re doing really well with wavefront-optimized,” he says. “The point that Guy Kezirian, MD, and I have been making for a while now is that if a patient doesn’t have enough higher-order aberrations, we think a wavefront-guided treatment is not necessary.”
|
Mirroring an overall trend in refractive surgery, LASIK surgeons say their average flap thickness has decreased, from an average of 121 µm on last year’s survey to 118 µm this year. Sixty-four percent of them use a femtosecond laser to create the LASIK flap. Whether the remainder decide to give the femtosecond laser a chance is still up in the air, however, with 60 percent saying they’re “unlikely” to start using the femtosecond for LASIK in the coming year, and the rest stating that they’re “somewhat likely” to do so.
In terms of what they charge for their refractive procedures, the average price on the survey for LASIK (one eye) is $2,495. The surgeons who have to pay a facility fee say the average fee is $691. The average charge per eye on the survey for other procedures is $2,300 for PRK; $3,500 for phakic lens implantation and $4,800 for clear lens extraction/IOL implantation.
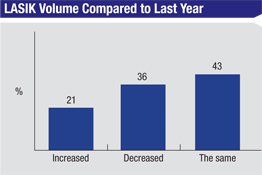
In terms of trends in surgical volume, only 26 percent say that they’re doing more refractive procedures this year than last, with an average increase on the survey of 8 percent.
Forty percent say their volume is the same as last year and a third say it’s decreased. The average decrease in volume on the survey was 28 percent. Dr. Stonecipher says that though his practice’s volume is up from last year, it’s still down compared to previous years, and this has a lot to do with the general economy. “In our area, unemployment is 11 percent, the highest in 80 years,” he avers. “And in West Virginia, it’s 20 percent.”
|
In recent years, there’s been a controversy in refractive surgery over the best way to approach a LASIK enhancement. On this year’s survey, half of the respondents say they’d lift the flap and ablate, 29 percent say they’d avoid doing another LASIK and perform a surface ablation on the top of the flap, and 21 percent say their approach would depend on factors such as the time elapsed since the original surgery. “I’ll lift the flap for the enhancement if it’s been less than two years since the original LASIK,” says a surgeon from Arizona. “After two years, I’ll ablate the flap.” A surgeon from Florida says he’s seen firsthand what can happen if the wrong enhancement method is chosen in this instance. “I like PRK over the flap,” he says. “But recently, I saw a disaster in which a patient had a recut LASIK flap that went really bad: There was an incomplete flap with exit of the microkeratome through the center of the cornea.”
Focusing on Lenses
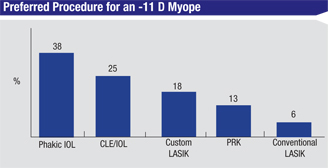
Though LASIK is the surgeons’ primary procedure for their refractive cases, a number of them turn to intraocular lenses, both phakic and in conjunction with clear-lens extraction, to solve some patients’ visual issues.
A third of the surgeons on the survey say they use phakic lenses.
“I use both the Verisyse and the Visian in my practice,” says a surgeon from Minnesota. “I like them both. The advantage of the Verisyse is that it sits farther from the crystalline lens so there’s less incidence of cataract, but there’s a larger incision and, occasionally, the lens is visible to patients. For the Visian, the advantages are faster recovery and the fact that the lens is invisible to the patient, but there’s a slightly higher risk of cataract and more sizing issues. However, sizing is better now with high-resolution ultrasound and Pentacam images of the anterior chamber. Ultrasound is also easier with newer technologies such as the Clearscan bag that makes it less of a mess.”
|
Surgeons also weighed in on the use of presbyopic intraocular lenses for clear-lens extraction/IOL implantation procedures. Thirty-nine percent use the Tecnis multifocal lens, 29 percent use the ReSTOR +3 D lens, 18 percent use the Crystalens AO and 4 percent use the Crystalens HD (some surgeons chose more than one lens). Seven percent of the panelists say they don’t perform CLE/IOL at all in their practices. Of the surgeons who do perform CLE, 4 percent say they will sometimes mix different varieties of presbyopic lenses to enhance the effect for certain patients’ visual needs.
Bloomington, Minn., surgeon Elizabeth Davis says she primarily uses the Tecnis multifocal when she performs clear-lens extraction. “It gives an excellent quality of vision and predictable refractive outcomes,” she says. “My patients are very satisfied, and a high percentage of them can go without glasses.” Another surgeon from Minnesota feels similarly, saying, “The advantage of this particular lens is that it has accurate lens powers, unlike some lenses that can shift in the eye and have a more variable lens position. There’s also minimal glare and halo associated with it.”
|
Though the therapeutic procedure known as corneal cross-linking—which combines riboflavin with an ultraviolet light treatment in an effort to strengthen the cornea—isn’t approved in the United States, some surgeons, especially those who have been involved with cross-linking trials, say they’re eagerly awaiting its arrival. Fifty-three percent of the panel respondents say they’re very interested in performing corneal cross-linking, 41 percent are somewhat interested but 5 percent aren’t interested in the procedure.
“I’d love to be doing corneal cross-linking,” says Dr. Stonecipher. “I’ve probably referred at least 20 cases to have it done.” A Florida surgeon with experience in corneal cross-linking thinks surgeons will appreciate the procedure if it’s eventually approved in the United States. “We are in an ongoing clinical trial of the technique known as epithelium-on cross-linking,” he says. “And the results have been great.”
“I am doing cross-linking as the principal investigator in a single-practice, FDA-monitored clinical trial,” says a surgeon from Illinois. “This treatment is currently curing a potentially blinding keratoconus condition in young people. The treatment also gives these keratoconus patients the chance to undergo supplementary laser vision correction. This is the kind of thing that I went into ophthalmology for.”
REVIEW