An overview of MACRA’s requirements follows (with an emphasis on the Merit-based Incentive Payment System, or MIPS); the president of the AMA and two ophthalmologists comment on the pros and cons of the government’s attempt to reward quality of care over volume of treatment.
The Quality Payment Program
The Quality Payment Program (QPP) is the cornerstone of MACRA. Most providers who participate in Medicare Part B are relegated to one of the QPP’s two tracks: Advanced Alternative Payment Models (APMs) or the Merit-based Incentive Payment System (MIPS). Advanced APMs are a subgroup of Alternative Payment Models that reward clinicians for assuming some risk tied to patient outcomes. They include Next Generation ACOs; Comprehensive End-Stage Renal Disease Care and Oncology Care Models with two-sided risk; and Shared Savings Program ACOs-Track 2
 |
MIPS is the relevant branch of the QPP for the vast majority of ophthalmologists right now, but a major goal of MACRA is to foster a shift to advanced APMs. “Certainly, the most well-developed APMs are centered on primary care,” says David O. Barbe, MD, president of the American Medical Association, via email. “Private industry insurers, and the primary-care specialties themselves took the lead in developing these models in the private sector many years ago. Most specialists, including ophthalmologists, do not fit neatly into the relatively few APMs that fit the QPP criteria for being designated as ‘advanced’ that would provide an exemption from MIPS. This is something that specialists are working to remedy, with new models being proposed to the Physician-Focused Payment Model Technical Advisory Committee (PTAC) [chartered by the U.S. Department of Health and Human Services] for review of potential recommendation to the secretary of HHS for further development and adoption by Medicare,” he says.
While most ophthalmologists
 |
Only one dimension of MIPS reporting is new (Improvement Activities); the other three are legacies of the system that it replaces. “To the extent that ophthalmologists were comfortable with the old Physician Quality Reporting System (PQRS), they will be comfortable with the same measures being applicable to them under the Quality component of MIPS,” says Dr. Barbe of the AMA. Brock K. Bakewell, MD, FACS, partner at Fishkind, Bakewell & Maltzman Eye Care in Tucson, Ariz., and adjunct associate professor of ophthalmology at the University of Utah, agrees, adding, “All of the previous quality elements from the PQRS have morphed into the MACRA system.”
MIPS scoring replaces and consolidates the PQRS, the MU, and the VBM, while adding a new measure, Improvement Activities:
Quality (replaces PQRS): The Quality component accounts for 60 percent of the composite MIPS score for the 2017 reporting period. Providers must select at least six quality measures approved by CMS to report: One of the six must be an outcome or high-priority measure. Practice groups of 16 or more providers can earn 70 points; smaller groups can earn 60. Each can earn a 10-percent bonus score.
Advancing Care Information (replaces Meaningful Use): ACI is weighted at 25 percent of the total MIPS score for the 2017 period. There is a 50-point base score achievable only by having an electronic health records system in place, with 90 more possible performance points and 15 bonus points thereafter.
Resource Use (replaces VBM): This measure of costs is weighted at zero percent for 2017. Since CMS tabulates Resource Use from Medicare Part B claims, providers don’t need to do any reporting. The proposed rule for CY 2018 would keep this component from factoring into the MIPS composite score for the 2018 reporting period as well.
Clinical Practice Improvement Activities: Weighted at 15 percent of the composite score, this new metric requires providers to report on up to four CMS-approved activities. Measures to choose from include patient safety and practice assessment, coordination of care and emergency preparedness. They are worth up to 20 points apiece. The scoring on this domain offers some leeway for small or solo practices and providers in rural or designated HPSAs (health-professional shortage areas): Those providers can earn double points in this category, earning their 40 possible points by completing a single 20-point measure.
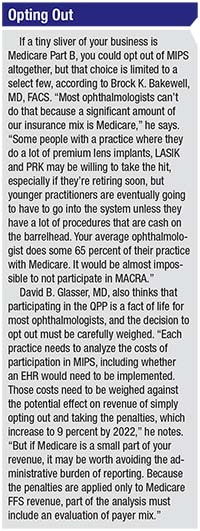
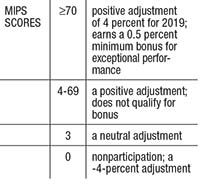
CMS set the 2017 “performance threshold” score for MIPS at 3 points, meaning that it takes a composite MIPS score of 3/100 points to avoid a downward adjustment in 2019 Medicare payments. Here is an outline of the scoring thresholds:
By 2022, the upward and downward
 |
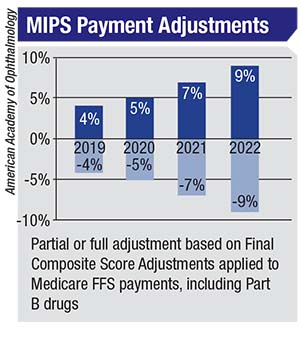 |
As Dr. Bakewell notes, even good ophthalmologists could find themselves among the losers because of the budget-neutral nature of MACRA. “You have to do better than the average, or you’re potentially going to get cuts under MACRA that are not insignificant,” he says. “If someone’s getting a 9-percent bonus [in 2022], someone else is getting the same penalty. I think that configuring it so that there are winners and losers will create a hardship. We’re already performing at a very high level. Our outcomes are excellent, so I think it’s problematic to try to differentiate a specialty such as ophthalmology that is already at such a high level across the board.”
That competition is further underscored by Physician Compare, which will list providers’ MIPS scoring online sometime after the March 31, 2018 deadline for 2017 data submission. CMS describes Physician Compare as “a website designed to help consumers make informed choices about the health care they receive through Medicare.”1
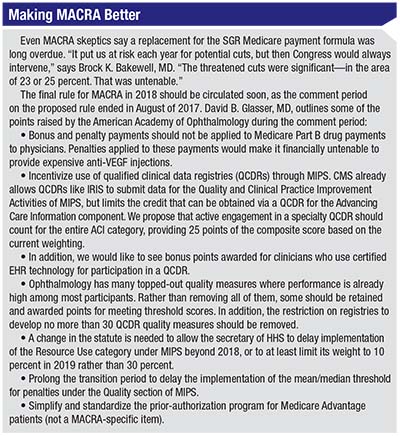
Could concerns about potential reputational damage from a surgeon’s published score prompt him or her to shy away from higher-risk Medicare patients? “Quality measures do have the potential to disincentivize reporting on complications, or to encourage referring out cases with a higher probability of a poor outcome,” acknowledges David B. Glasser, MD, assistant secretary for health policy, American Academy of Ophthalmology, and assistant professor of ophthalmology at Johns Hopkins University School of Medicine. “But I have to believe that physicians place the welfare of their patients above a number that makes up a small percentage of another number that may affect a percentage of their payments. On a more practical level, this risk can be mitigated by excluding high-risk cases from the denominator or by risk-adjusting for comorbidities. We have advocated for excluding all of the high-risk cases that were excluded under the old PQRS system,” he says. (For more proposals on how to improve MACRA implementation, see sidebar.)
Role of the IRIS Registry
The Intelligent Research in Sight registry is the first comprehensive clinical data registry for eye-disease cases. It’s also a Qualified Clinical Data Registry (QCDR) for 2017 MIPS reporting, capable of optimizing MIPS quality reporting when IRIS is integrated with qualified EHR software. IRIS Registry use is worth MIPS points in the ACI and Improvement Activity domains. Practitioners with a certified EHR integrated with the IRIS Registry enjoy automatic quality reporting to CMS, and IRIS will optimize the measures reported to maximize their MIPs point values. IRIS Registry users without an EHR may enter quality data manually using the IRIS Registry web portal, and may be able to earn MIPS points in Improvement Activities performance.
For Advancing Care Information points, you must have a qualified EHR: This is an all-or-nothing proposition worth either 50 or zero points. Iris Registry participation will net EHR users an additional five-point bonus in this category.
Dr. Glasser believes that making IRIS Registry use more valuable in MIPS scoring would create a more specialty-specific snapshot of what constitutes a high-quality clinical outcome in ophthalmic care. “More relevant outcomes like postoperative visual acuity and accuracy of IOL power selection cannot be extracted from claims data,” he says. “That data does exist in the IRIS Registry. We would like to see CMS allow IRIS data to play a larger role in determining MIPS quality scores that are relevant to ophthalmology,” he says.
MIPS and Smaller Practices
Lack of an EHR effectively prohibits solo providers and practices from earning any of their MIPS points from the ACI domain. “Small practices, particularly those without electronic health records, face a larger administrative burden in trying to achieve the maximum bonus under MIPS,” says Dr. Glasser. “In 2017, only three points are necessary to avoid the penalty. Reporting a single quality measure or clinical practice improvement activity makes it very easy for any practice to avoid the penalty in 2017. For 2018, the penalty threshold is expected to increase to 15 points if the recommendations put forth by CMS in their proposed rule are carried forward in the final rule. Fifteen points remains an easy threshold to meet. After 2018, the penalty threshold is expected to increase substantially. That will be a more difficult hurdle to clear.”
The proposed rule for 2018 speaks of small practices in supportive terms. “The support of small, independent practices remains an important thematic objective for the implementation of the Quality Payment Program and is expected to be carried throughout future rulemaking,” it states.2 The document outlines some measures intended to provide relief to solo practices, practices of 15 or fewer providers and those in rural or medically underserved areas. Chief among those is the proposed raising of the low-volume threshold from up to $30,000 in Medicare Part B allowed charges to a maximum of $90,000, and the Medicare Part B beneficiary patient volume from a maximum of 100 up to 200. CMS estimates that this measure would exempt an additional 390,000 providers from MIPS reporting requirements.
The proposed rule also contemplates offering small or solo practices a way to avoid penalties to their composite score via “significant hardship exemptions,” since not having an EHR, for example, cuts a provider’s potential “perfect” score from 100 to 75 right off the bat.
 |
MIPS reporters can also see whether they qualify for technical assistance from CMS in on-ramping to the QPP. Priority goes to rural practitioners, those in medically underserved areas and those with low MIPS scores from CY 2017. More information on the technical assistance support available to small practices can be found at https://qpp.cms.gov/docs /QPP_Support_ for_Small_Practices.pdf. A provision allowing virtual groups may also let smaller practices separated geographically pool their data for more robust scores.
Value and Motivation
The switch to value-based care is meant to reward efficient providers who document good outcomes, in an effort to phase out Medicare’s longstanding fee-for-service environment. But this effort begs the question of what kinds of care and outcomes are valuable. “It is extremely difficult to measure quality through claims data alone,” Dr. Glasser acknowledges. “A few things, like return to the operating room after cataract surgery, can be quantified by claims alone. But these events are extremely uncommon,” he says.
Value-based care is the new law of the land, but whether pay-for-performance improves processes of care or health outcomes remains unclear.3 Dr. Bakewell suspects that MACRA’s more-stick, less-carrot approach will force physicians to focus on data entry over patient care, and will not inspire the best possible outcomes. “I’m not quite sure how you do this with ophthalmology because we do a lot of procedures, and you’re going to end up captitating doctors if you move from fee for service. Capitation doesn’t work because it’s not a good motivator. It’s like putting a doctor on a salary, where it won’t matter if they do 100 cataracts or 1,000 cataracts—they’re still going to be paid the same salary,” he says.
“You’re not free to charge what you feel you’re worth. You could be the best doctor in the world for doing a certain procedure, but you’re paid the same as everyone else in the Medicare system, unless your outcomes are superior; then maybe you get a little bonus, contingent on how well you document it,” he continues.
“Doctors are very tired of regulatory burdens,” Dr. Bakewell adds. “Physicians and their staff spend way too much time inputting data to EHRs. It’s taking away from patient care and it’s not emphasizing the right thing. The right thing is for doctors to be taking care of patients, not entering data.”
Dr. Bakewell advocates gradual implementation to allow ophthalmologists to initiate MIPS reporting without penalty. “We want this to be eased in gradually. We want to keep the Resource Use element out of the final MIPS score for another three years, so that people can start to participate in MACRA without being penalized,” he says. REVIEW
Dr. Bakewell and Dr. Glasser report no financial interests in connection with the topic discussed.
1. Centers for Medicare & Medicaid Services. Physician Compare Initiative web page. https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/physician-compare-initiative/.Accessed 8 October 2017.
2. Centers for Medicare & Medicaid Services. Medicare program; CY 2018 updates to the Quality Payment Program. Fed Register 2017;82:125:30010-30500.
3. Mendelson A, Kondo K, Damberg C, Low A, et al. The effects of pay-for-performance programs on health, health care use, and processes of care. Ann Intern Med 2017; 166:341-353.



