DMEK has earned its reputation as a tricky transplant procedure for good reason. “Every case is very different,” says Jack Parker, MD, of Parker Cornea in Birmingham, Alabama. “When you’re doing other challenging eye surgeries, they typically proceed algorithmically. You may be faced with a difficult scenario, but there are published steps and tactics for each of those potential challenges. With DMEK, it’s not always obvious what to do next, even for experienced DMEK surgeons, and you need to have a feel for how the tissue behaves in the eye. It’s problem solving on a timer, and it’s not easy to develop a sense for how to solve that problem without lots and lots of practice.”
In the absence of virtual simulations and eye models, Dr. Parker recommends watching DMEK videos. “You can to some extent recapitulate the process using tissue obtained from an eye bank to practice in a wet lab, but probably the best way to learn the dynamics of the graft behavior is to watch videos, especially your own,” he says. “Play them back and observe how the tissue responds to various stimuli and manipulations.”
 |
|
Figure 1. Starting out with the graft in the correct orientation will help to ensure smooth delivery and unfolding of the graft. |
The learning curve for DMEK is long and takes commitment, surgeons say. “DMEK presents one of the steepest learning curves among eye surgeries,” says Ahmed Bardan, MSc, MD, PhD, a consultant ophthalmic surgeon at St. James University Hospital in Leeds, United Kingdom. “The tissue involved is fragile, and numerous anatomical, surgeon-related and patient-related factors must be considered.”
Here, Dr. Parker and Dr. Bardan share tips for when graft unfolding doesn’t go as planned, and discuss how they handle the graft in complex cases with variable eye anatomy.
Eye Anatomy
The depth of the recipient anterior chamber plays a key role in the success of DMEK graft manipulation during surgery. “In a shallow anterior chamber, everything is mashed together and it’s difficult to unfold the edges of the DMEK tissue,” Dr. Parker says. “In a hyper-deep anterior chamber, such as an eye that’s been previously vitrectomized, the chamber can be so deep that the graft just spins around in the eye, and it’s difficult to unfold because there’s no compression between the back of the cornea and the front of the patient’s iris. Each of these extremes presents challenges.”
“We advise surgeons about to start doing DMEK to choose ‘standard’ eyes,” Dr. Bardan says. “A standard eye won’t be extremely myopic or hyperopic. The anterior chamber won’t be too deep or too shallow. Avoid vitrectomized eyes, aphakic eyes that had previous complicated surgery, eyes with previous glaucoma surgeries or eyes with any device in the anterior chamber such as an AC IOL. These additional factors make the surgery more complicated.”
 |
|
Figure 2. Shallowing the anterior chamber after graft delivery encourages the graft to flatten out. |
He adds that patients on antiplatelet medications for cardiac disorders are more likely to bleed and have fibrin released during surgery. “Once you get fibrin, it makes the graft adhere to itself, and it’s very difficult to unfold,” Dr. Bardan says. “Fibrin is your enemy when you do DMEK.”
DMEK Technique
Striving to establish a degree of standardization in the DMEK technique—acknowledging the inherent variability of each case—can assist surgeons in developing a robust foundation and gaining confidence in this sophisticated keratoplasty procedure, Dr. Bardan explains. “The complexity of certain eyes, particularly those affected by conditions such as peripheral anterior synechiae, prior glaucoma surgeries, aniridia or vitrectomy, renders it nearly impossible to fully standardize the procedure, as there will invariably be additional complicating factors.
“I believe in standardization in general for corneal and refractive surgeries,” he continues. “With DMEK, one way to handle the steep learning curve and meet each challenge is to minimize deviation from the steps you perform each time. This also helps minimize the surgery time.”
Dr. Bardan says that taking the time to carefully inject the graft in the proper orientation will help the rest of the procedure go more smoothly. “For surgeons just starting DMEK, the injection technique is a common delivery approach. When delivering the graft into the anterior chamber, ensure it’s in the correct orientation, facing the correct way with the endothelium side down and the Descemet’s side up towards the cornea (Figure 1). Delivering the graft in the correct orientation into the center of the anterior chamber, using gentle insertion rather than a gush insertion helps maintain its correct orientation.
“At the end of the graft delivery, I intentionally shallow the anterior chamber (Figure 2). This shallowness provides no room for the graft to remain scrolled and it encourages the graft to become flat and open up. If it’s not a tight scroll—since today we use donor tissue from older donors—the graft should open up with gentle tapping on the center of the cornea.
“Centration before unfolding is important,” he notes. “Once it’s unfolded, the graft becomes more difficult to mobilize inside the eye because all or part of the graft will be touching the corneal stroma.”
Graft Configurations
Certain graft configurations call for unique unfolding approaches. “One of the things you don’t want to do is just bang aimlessly on the surface of the cornea,” Dr. Parker says. “This can be deleterious to the outcome because you’re wasting time and washing some of the trypan blue off the back of the graft, making it more difficult to unfold.”
He notes that though every case is different, there are actually only a few possible graft configurations. “The graft is a circular sheet of cells that tries to curl in on itself,” he says. “For the most part, it curls into a handful of more or less identifiable configurations that have names.”
These names include:1
- single roll;
- double roll;
- bouquet;
- jib;
- paper airplane;
- taco;
- folded edge;
- rolled edge;
- open plaster;
- bulge;
- tricorne hat; and
- square.
“It’s useful to name these various configurations because there are different strategies that you can employ depending on how the graft is curled,” continues Dr. Parker. “So, if you’re struggling to unfold the graft, it can be useful to take a step back and ask yourself, ‘What is the name of this configuration?’ After you’ve named it, then ask, ‘What are some of the effective strategies for this particular configuration?’ ”
 |
|
Figure 3. To encourage a double-scrolled graft to open up, tap gently on the center of the cornea, parallel to the axis of the graft scroll. |
Two common configurations can be addressed like this: For a double-scrolled graft, which is the standard way the graft scrolls, Dr. Bardan recommends gentle tapping on the center of the cornea, parallel to the axis of the scroll to encourage it to open up (Figure 3). If one side is scrolled and the other is flat, Dr. Parker and Dr. Bardan say the Dirisamer technique can be employed, which involves pressing one cannula on the cornea over the flat part of the graft to keep it flattened, and tapping with a second cannula over the folded part until it unfolds.
Other techniques include bubble bumping for peripheral inward folds; the help-yourself technique, which involves using a single cannula to poke over one edge of a folded graft; and small air bubble-assisted unrolling or the Dapena maneuver. “There are lots of different techniques,” says Dr. Parker.
Common Obstacles
Here are a few common roadblocks and pearls for how to handle them:
• The patient has atypical anterior chamber depth. “For eyes with a deep anterior chamber, you almost always need an air bubble to help unfold [the graft],” Dr. Parker says. “That air bubble supports the graft from the top or from below and artificially shallows the anterior chamber. It gives you a helping hand in unfolding the graft in an eye that it would otherwise be very difficult.
“For an eye with a shallow anterior chamber, one solution to deepen it involves doing a pars plana vitrectomy,” he continues. “It can be limited, but often just removing some vitreous from behind the IOL or the limbus can deepen the chamber enough for you to unfold the graft easier.”
• The graft is upside-down. “In a situation in which you feel like you’re struggling, one effective strategy instead of randomly tapping the corneal surface is to deepen the chamber with saline and flush the graft in the anterior chamber into a more friendly configuration,” Dr. Parker says.
For a crumpled graft or an upside-down graft, Dr. Bardan recommends “injecting BSS behind the scroll through one of the side ports and directing it in a way that creates a current in the anterior chamber that encourages the scroll toward the correct orientation. Once you achieve this, shallow the anterior chamber to preserve that orientation and start using one of the tapping techniques to unfold it.”
• The graft still isn’t unfolding as it should. Sometimes, the graft still refuses to unfold, and then the surgeon must figure out what’s causing the problem. “If it’s a combined phaco-DMEK, for example, there could be some residual viscoelastic that’s stopping it from unfolding,” Dr. Bardan says. “There could be microscopic fibrin in the anterior chamber that’s started to entangle parts of the graft—which will prevent it from opening up. It could also be that the space within the anterior chamber, such as a certain part of the angle, doesn’t have enough room for the graft to unfold. An arcus senilis or corneal cloudiness could obscure your view. The surgeon should think about what’s causing the problem and then have a plan of action to deal with it.”
If fibrin is present in the anterior chamber, the situation becomes tricky since it can be challenging to clear the fibrin. “We have access to tissue plasminogen activator or tPA, which you can inject into the anterior chamber to cause fibrinolysis,” says Dr. Bardan.
 |
|
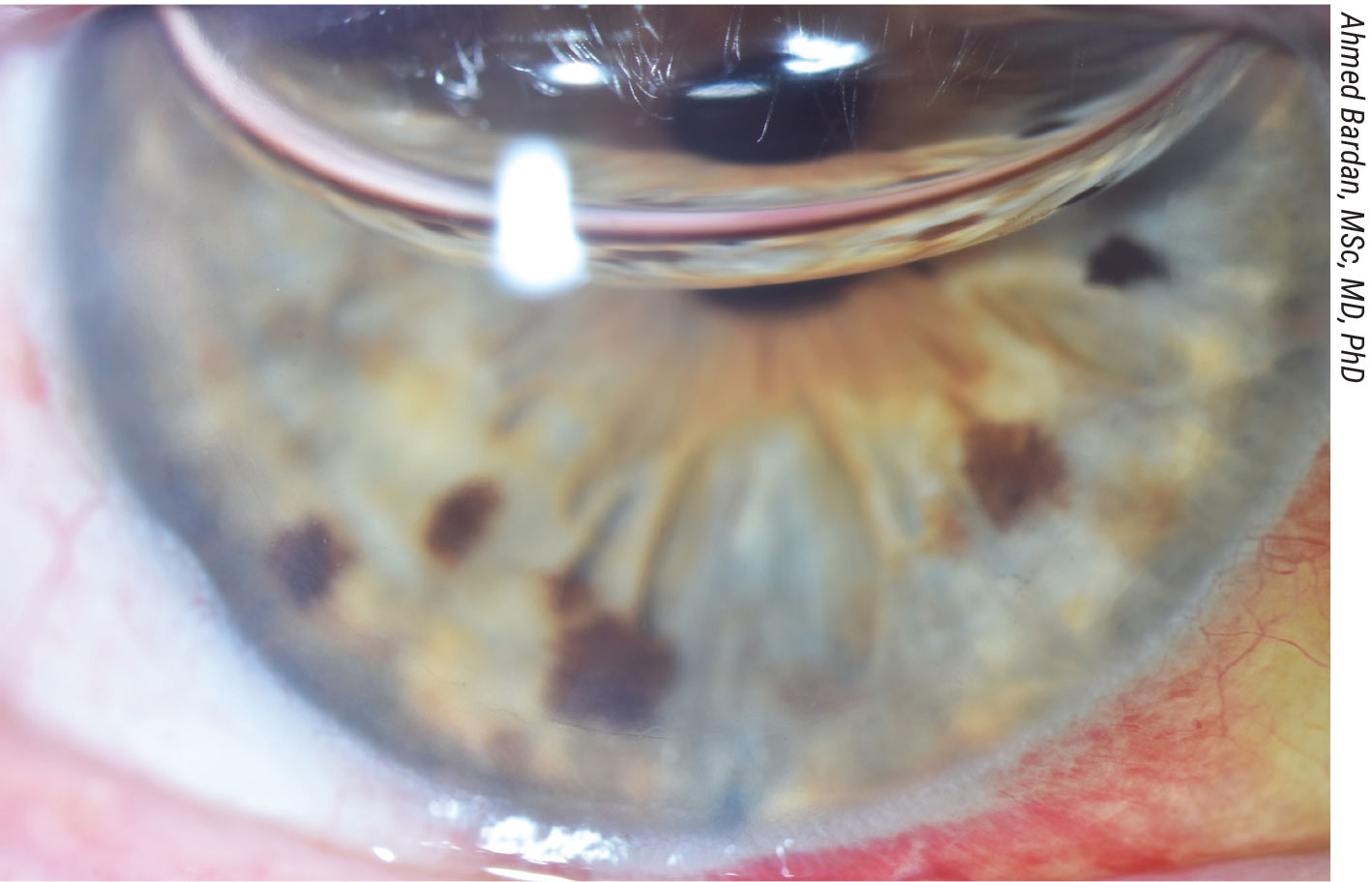
In this photo taken on postoperative day four after a combined phaco, IOL and DMEK procedure, the cornea is clear, the graft is attached and the bubble size is approximately 50 percent of the anterior chamber volume. |
Unfolding Grafts in Complex Eyes
New variables in the mix complicate DMEK surgery, but there are steps you can take to ensure a successful outcome. Here are some tips for the following scenarios:
• Previously vitrectomized eyes. In an eye that’s undergone vitrectomy, the iris-lens diaphragm is pushed backwards, making the anterior chamber much deeper and the DMEK unfolding more challenging. “If you try to unfold the graft in a previously vitrectomized eye, every time the anterior chamber reforms, the graft scrolls back on itself,” Dr. Bardan says. “I inject a small air bubble underneath [the graft]. This air bubble occupies part of the anterior chamber volume and leaves no big space in the anterior chamber for the graft to scroll back on itself.”
• Narrow angles. For eyes with narrow-angle glaucoma with PAS, Dr. Bardan says he sizes the DMEK graft based on how much room there is in the anterior chamber rather than cutting the graft and pre-sizing it based on the white-to-white preoperative dimensions. “I don’t cut the graft in these cases with complex anterior chambers until I go inside the eye and do the Descemetorhexis,” he explains. “I put an air bubble inside the anterior chamber to test for the dimensions. Sometimes there’s a very fixed adhesion between the iris and cornea, and that prevents the bubble from expanding to the angle of the anterior chamber. If this bubble is, for example, 7.5 or 7.25 mm, then I adjust the graft size to match and be slightly smaller. This approach can help make these challenging cases easier.”
• Eyes with a device in the anterior chamber. Glaucoma drainage devices and anterior chamber IOLs can complicate DMEK surgery. “If there’s a device in the anterior chamber, I’ve found that the best way is to try to get the procedure done as quickly as possible,” Dr. Bardan says. “This is best done by an experienced surgeon who knows how to get the graft to unfold as quickly as possible.”
• Aphakia. In aphakic eyes, the surgeon faces the possibility that the graft might fall into the posterior segment. “If the patient is aphakic, I try to use the iris as a shelf,” Dr. Bardan says. “I inject the graft toward the iris shelf to keep it in position to avoid flushing it toward the posterior segment. I use an iris repositor ‘spatula’ to encourage the graft to open up quickly before tapping, as tapping initially may cause the graft to drop through the pupil.
“It’s challenging to get a decent gas bubble or air bubble fill for the anterior chamber in these eyes, since the air or gas keeps escaping toward the back of the eye,” he continues. “One thing I do, if the eye has been vitrectomized, is to try to get a gas bubble fill in both the posterior and anterior segments. Leave the tamponade on the table intraoperatively for 10 to 15 minutes and then release it.”
Aphakic eyes that are also aniridic or have significantly deficient iris tissue are more challenging. “There’s a greater chance of the graft dropping to the posterior segment,” Dr. Bardan notes. “Our colleagues at Moorfields Eye Hospital have described a technique using Prolene suture to create a scaffold mesh that replaces the iris diaphragm. If you manage to insert the graft flat on top of these suture lines, then once the graft is unfolded and gas is injected, you can remove the Prolene sutures.”
• Phakic eyes. “Our standard technique for all DMEK procedures, whether or not the eye is phakic, involves creating a preoperative YAG laser inferior peripheral iridotomy to avoid iris bleeding and fibrin release,” Dr. Bardan says. “This is a must for phakic eyes because there’s a higher chance of postoperative pupil block with the air [tamponade] used.
“For phakic eyes, I use preoperative pilocarpine drops to keep the pupil constricted,” he continues. “I insert the graft, similar to as I would in aphakic eyes, onto the iris shelf. So, the graft will go to the side rather than the center. Once the graft is in the eye, avoid crossing over the pupillary area with instruments or fluid irrigation to avoid causing any lens trauma or inducing an early cataract.”
He says he performs the Descemetorhexis under Healon cohesive viscoelastic to protect the lens and then aspirates it before insertion of the DMEK graft. “Once the graft is unfolded, we use air instead of SF-6 gas to tamponade the graft because SF-6 will have a higher chance of causing pupil block and angle closure, and a higher chance of inducing cataracts,” he says. “At the end of the case, be sure to check that the bubble isn’t occluding both the pupil and the peripheral iridotomy.”
Though DMEK is a challenging procedure, Dr. Parker points out that it’s also a very forgiving operation. “It’s difficult for things to go horribly wrong,” he says. “Surgeons are afraid of starting with it because it’s challenging to problem-solve on a timer. But the way to learn is to start. Once you start, you’ll pick up insights along the way.”
Dr. Bardan and Dr. Parker have no related financial disclosures.
1. Parker J, Parker J, Melles G. DMEK Unfolding Manual. Published September 6, 2019.



