As physicians managing patients with glaucoma, we face numerous practical challenges. One of them is accurately monitoring intraocular pressure. Most of us only get to check our patients’ pressures every few months in the clinic, which is far from ideal, since we know that pressure fluctuates over time.
It’s no secret that researchers are striving to make 24/7, high-tech IOP-monitoring a reality. That technology will bring us new challenges, inclding figuring out what to do with the enormous amount of data it will produce for every patient. But in the meantime, it’s possible to improve on our current, sparse supply of data by asking selected patients to monitor their pressure at home. This offers the possibility of getting several readings each day over a period of weeks or months—enough information to make us aware of what’s happening to our patient outside of the office without drowning us in data points.
Home monitoring of IOP is still in its early stages, but as a pediatric glaucoma specialist, I now have several years of experience using rebound tonometry in clinic and at home with young patients. I believe my experience with childhood glaucoma can help to shed some light on the challenges and benefits that lie ahead when this technology becomes more widely used—hopefully in appropriate adult glaucoma patients as well as children.
Benefits of Home Monitoring
The theoretical advantages of having IOP measurements taken outside the office are not hard to see:
• A more accurate measurement of peak IOP. The variability of IOP over time sometimes surprises us; occasionally, the pressure we measure in the office is very different from the previous visit. So it shouldn’t be a surprise—and it has been my experience—that multiple measurements taken outside of the office frequently reveal much higher pressures than we measured in the office.
• Catching pressure fluctuations. It’s been shown that pressure fluctuations—even those measured during periodic office visits—are associated with progression in adult open-angle glaucoma. (This stands in contrast to patients whose IOPs are at target and stable.) We also know that pressure fluctuations can happen outside of office hours. Measuring IOP over a larger range of time offers the possibility of catching those fluctuations.
That raises another point:
• Some fluctuations caused by surgery can be dangerous when they’re not carefully monitored. Sometimes the treatments we pro-vide—including surgery—cause dramatic IOP fluctuations. In the pediatric world, situations prone to such fluctuations might include doing angle surgery and having a little blood in the eye; putting the child on steroids; or putting in a Baerveldt drainage device where we purposely tie the tube off, knowing that it’s going to open when the stitch dissolves. In the latter situation, the pressure may be very high until the stitch dissolves; then it may drop very low. In the adult world, some MIGS procedures are also associated with pressure spikes.
If IOP is being monitored at home during such high-risk times in vulnerable patients, we’ll know when there’s an abrupt pressure change that needs to be addressed.
• Fewer concerns about patients missing office visits. Patients who need to have their pressure checked sometimes can’t come to the office when, or as often, as we’d like. For a patient measuring IOP at home, some office visits purely for IOP checks might actually be unnecessary.
• A single in-office diurnal curve measurement may not tell the whole story. It’s helpful to measure a diurnal pressure curve over the course of a day in the clinic (if the patient can manage this), but some studies have shown that in adults the diurnal fluctuation may not be exactly the same from one day to the next.
 |
| IOPs tended to be higher in the mornings and lower in the evenings for both normal and glaucoma patients. (Flemmons, Hsaio et al. 20111) |
What’s Taking So long?
Despite the promise of home IOP monitoring, a number of obstacles have caused this idea to get off to a slow start. The first obstacle has only recently been overcome: Having available technology that can safely be used by patients at home.
Most tonometers aren’t suited to home tonometry because they require anesthetizing the cornea. Any physician will be reluctant to let a patient use an anesthetic at home, because if the eye is anesthetized for a home-based reading, there’s a risk that the person taking the pressure will injure the cornea. Neither person would know anything had happened until the anesthetic wore off.
Tonometers that can accurately measure IOP at home without topical anesthetic are not common. In theory, parents could use an air puff device of some type to take the readings, but most patients—young or old—don’t enjoy that experience. In fact, the lack of multiple FDA-approved options for home IOP monitoring is largely the result of the fact that most IOP-measuring technologies don’t lend themselves to home use.
In my experience, the only technology that can easily be used to measure pressure without an anesthetic at home—at least for now—is rebound tonometry, because it touches the eye so gently. I first be-came interested in this technology when a colleague mentioned a new tonometer that didn’t require a topical anesthetic. In the pediatric world, that’s huge; by the time you put in the topical anesthetic and the child has had a meltdown, you’re starting from scratch, convincing the child to let you check the pressure. Even the Tonopen, which has been the standby for pediatric patients, often proves challenging to use in young children for the same reason.
The first rebound tonometry I tried was the TAO1i from Icare, the company’s first model; our early studies were conducted using that device. It provides a reliability index with each reading and it’s pretty easy to use, but it doesn’t store any data. The next model, the ic100, has a display on it and a few extra bells and whistles. The Icare Pro version (not commercially available in the United States) has storage capability and can be used upright or flat, so you could use it on a patient lying down, making it feasible for use in the OR.
Recently, the Food and Drug Administration approved the Icare HOME model, designed specifically to allow an older patient to use it on himself, thus making home IOP measurement feasible. The device knows whether you’re measuring the left or right eye, and it has a red-light-green-light display that lets patients know when they’re at the right distance from the instrument and the device is angled correctly. When the patient is finished taking a reading, it shows either a repeat indicator or a checkmark, so the patient knows when it’s time to do the other eye. (Notably, it doesn’t let the patient see the pressure reading.)
If the reading was reliable, the machine will store the data, including which eye was measured, the date and the time, the reliability index and the measured pressure. Currently, the device has to be plugged in to a computer to upload the data, but the company plans to upgrade the software to allow the device to wirelessly upload data to the cloud, where it would theoretically be downloadable by anyone with appropriate permission to access it.
Obviously, there will be other technologies that can be used by the patient at home—including high-tech options such as contact-lens-based monitors like the Triggerfish—in the future. I chose to study rebound tonometry because it was available and well-suited for this type of application.
 |
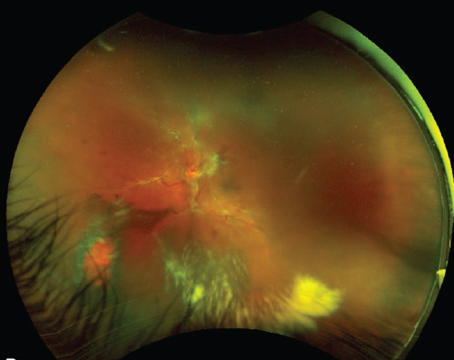
| This patient’s left eye had already undergone successful Baerveldt implantation. Surgery in the right eye during the home measurement period caused a short-term increase in pressure; a few weeks later when the ligature opened, pressure dropped. Being able to identify the actual timing of the ligature opening made it possible to manage the sudden pressure drop without guesswork. (Bitner et al. 20163) |
Getting Our Questions Answered
Because the idea of home IOP monitoring was relatively new, we set out to answer some key questions. Initially, we wanted to find out what rebound tonometry could and couldn’t do when used in the clinic, so we conducted a study in the clinic involving 71 children with known or suspected glaucoma.1 All of these children could tolerate Goldmann applanation, allowing us to compare the applanation and rebound tonometry IOP readings in a masked fashion. We found that the TAO1i usually read higher than Goldmann, by a little more than 2 mmHg. Occasionally the readings would be significantly different, for reasons we couldn’t determine; we never found one specific thing, such as corneal thickness, that might explain this. We also noted that the device didn’t hurt the cornea. When we stained the cornea, we couldn’t even tell that it had been used.
Next, we set out to see whether families could use the Icare (original model) for home tonometry in children. We studied it under a research protocol with 17 affected children (17 eyes) and 11 normal siblings.2 We found that caregivers obtained reliable readings 70 percent of the time. The data showed that daily IOP fluctuation occurred in both groups, and the pressures tended to be higher in the morning and lower in the evening. (See graph, p. 26.) Perhaps most significant, peak IOPs were sometimes much different from those measured in the clinic. In five subjects (31 percent) the peak IOP measured at home was more than 6 mmHg higher than that measured in the clinic. This caused us to alter our management of several of these patients, meaning we either performed surgery or changed medications.
Long-term Use at Home
Next, we wanted to know how long we needed to send a device home in order to catch pressure spikes. To get an answer, we examined data from seven children (average age: 9) enrolled to do home rebound tonometry three times a day for more than 30 days.3 On average, the monitoring lasted for about six months. The parents entered the data into an Excel spreadsheet or used our online entry form. Ultimately, we found that two weeks of monitoring in the children caught more than 90 percent of all pressure spikes, so we concluded that two weeks might be a good minimum length of time to have a child’s pressure monitored if the goal was specifically to find a pressure spike on a given treatment regimen.
We also were able to monitor the impact of our treatment, especially relating to surgical intervention in this small group of childhood glaucoma patients. On average, surgery lowered pressure by 10 mmHg. Perhaps most interesting, we found that the mean variation in pressure over the course of a day decreased when we improved aqueous outflow. Before the intervention, the average daily pressure fluctuation in those eyes was 8 mmHg; after surgery it was 5 mmHg. So not only did we lower the pressure by an average of 10 points, we also decreased the amount of daily pressure fluctuation.
One situation in which we found ongoing monitoring at home to be especially useful was following the implant of a Baerveldt drainage device, when we ligated the tube to prevent early hypotony. That turned out to be valuable for several reasons:
• First, we found that if we added steroids or surgery while the tube was ligated, the pressure usually went up before it went down. (This was not a surprise, but it was useful to know that the data confirmed our expectations.)
• We saw tremendous variations in pressure while we were waiting for the tube to open, sometimes prompting unplanned therapy changes for un-usually high IOPs caught at home.
• Perhaps most useful, the parents could precisely pinpoint the moment when the tube opened because the measured pressure would drop. It’s important to know when this has happened because as soon as the tube opens and the pressure plummets, the patient needs to stop using the glaucoma drops for a while or the pressure could get dangerously low.
Knowing when the tube has opened is especially important in some patients, such as those with Sturge-Weber-associated glaucoma, where there’s a choroidal hemangioma in the eye along with the glaucoma. Kids in this situation may get choroidal effusions—leakage from the choroidal hemangioma—and even serous retinal detachments if they have a dramatic pressure drop. If we can more precisely monitor the pressure as it’s changing, we can help to mitigate some of that. For that reason I now routinely use home monitoring in this situation.
Convinced that home IOP monitoring of selected childhood glaucoma patients was helpful in their care, we were interested in exploring attitudes towards home tonometry, both from our patients and our colleagues who treat childhood glaucoma. To that end, we recently sent a survey to 83 parents (or the patients themselves, if they had been treated as children but were now adults), and pediatric ophthalmologists and glaucoma specialists who care for kids with glaucoma. Eighty-four percent of the parents said they were very interested in using this technology; most felt it would improve their physician’s ability to monitor their glaucoma. Eighty percent of the surgeons who responded to our survey indicated interest and saw the potential benefit for patient care, but only 14 percent were actually using any form of home tonometry, demonstrating that this approach to IOP monitoring is by no means widespread.4
We also asked doctors in which situations they’d use home tonometry. Most physicians said they’d use it to try to catch IOP peaks or fluctuations that they suspected were occurring, either because readings were inconsistent or they couldn’t do enough clinic visits to be sure. Some said it might help them provide better postoperative care. Overall, most physicians felt there would be a benefit to using home tonometry in selected patients.
Barriers to Use
Despite its potential, a number of barriers to widespread use of home tonometry remain:
• Managing the information. One of the challenges that comes with implementing any kind of home tonometry is processing the resulting data. How do you collect it and make sense of it? How do you make sure you haven’t missed something?
• Opening up new areas of liability. When the patient is being measured at home, who is responsible for interpreting and responding to those measurements, and by what methodology?
• Cost to the physician/practice. Physicians and offices would have to spend money to own or rent the devices, to care for the devices, to train patients to use the devices, and to process all of the data. Currently, there are no treatment codes that would allow physicians to be reimbursed for these costs, although nothing would prevent them from renting the equipment to the patient.
One related thing we discovered is that patients get very attached to using the instrument! They (or their families) often don’t want to give it back. To make home tonometry feasible, one needs to own several (or more) of these devices—at a non-trivial initial cost. Fortunately, through generous support from Saving Kids’ Sight, we’ve been able to purchase several dozen tonometers to loan out (again, under IRB protocol). We’ve now reached out to several other institutions, sharing our protocol and tonometers, to help expand the reach of our Icare Lending Library Project.
• A lack of supporting evidence, especially in adult populations. There’s some evidence in the literature that this technology can be helpful when managing children, and my own experience supports that. However, as far as I know, there’s little published in the adult glaucoma literature demonstrating improved outcomes as a result of measuring pressures at home. I think that such supporting evidence will be needed to increase interest and the use of home tonometry for adult glaucoma patients.
The bottom line is that home tonometry is not likely to sweep the field of glaucoma in the near future. In fact, I suspect most busy clinicians will not want to do this except under select circumstances.
Onward and Upward
Studies involving home tonometry are now appearing in the literature, and some doctors are already using the Icare Home. Although this is currently mostly used in pediatric populations, the studies indicate that there’s interest in home tonometry in the adult world as well. Nevertheless, I think we’re quite far from widespread implementation at this point. And that may be reasonable: Based on our experience, home tonometry is not appropriate for every patient, nor is it necessary.
In the meantime, the technology continues to improve, and I believe the future for home monitoring is bright, for many reasons. The instruments are getting more user-friendly, and cloud-based storage of data is now on the near horizon. I can imagine a situation in the future in which electronic medical record systems will be able to seamlessly download and integrate the IOP measurements, much as can be done today with home telemetry for arrhythmia monitoring. Perhaps the device could even have an alarm that would alert the patient that her pressure is high and ask whether she remembered to use her drops, thus improving adherence.
In addition, once this technology becomes easy to use and is implemented in more practices, it may actually save doctors time by eliminating the need for patient visits that happen primarily just for a pressure check. Of course, once we have proof that this technology improves outcomes, we’re going to need some kind of reimbursement. And we’ll need to do a lot more research to find out which patients it can help the most, and how best to implement it.
In the meantime, our experience and data so far relate to caring for a very tiny subset of glaucoma patients—kids with childhood glaucoma. The rest of the iceberg, of course, is the adult community. I wouldn’t presume to tell doctors dealing with adult patients how or whether to use home tonometry, but I suspect that what we’re doing with kids is of interest to those doctors who are managing adults. Yes, implementing this technology in an adult practice with a large number of patients could be more daunting than what I’m dealing with, but I’m hopeful that our experience can act as a starting point for studies involving adults. REVIEW
Dr. Freedman is a professor of ophthalmology and pediatrics and chief of the Pediatric Ophthalmology and Strabismus Division at Duke Eye Center in Durham, North Carolina. She reports no financial ties to Icare or its products.
1. Flemmons MS, Hsiao YC, Dzau J, Asrani S, Jones S, Freedman SF. Icare rebound tonometry in children with known and suspected glaucoma. J AAPOS 2011;15:2:153-7.
2. Flemmons MS, Hsiao YC, Dzau J, Asrani S, Jones S, Freedman SF. Home tonometry for management of pediatric glaucoma. Am J Ophthalmol 2011;152:3:470-478.
3. Bitner DP, Freedman SF. Long-term home monitoring of intraocular pressure in pediatric glaucoma. JAAPOS 2016;20:6:515-518.
4. Mali et al. Home tonometry in childhood glaucoma: Clinical indications and physician and parental attitudes. JAAPOS 2018;22:4:319-321.