Dry-eye disease is used as an umbrella term to capture the various signs and symptoms of ocular surface disruptions in patients. Not all patients experience the same issues. If there was an examination technique that perfected the diagnosis of all dry-eye patients, then all ophthalmologists would use it. Unfortunately, such a device doesn’t exist, and there are many questionnaires, dry-eye tests and tools that are instead employed on a case-by-case basis.
Here, physicians provide the methods they use before deciding how to treat various forms of dry eye.
Diagnostic Methods
Diagnosing dry eye can be as simple as observing the ocular surface and eyelids under a slit lamp for signs and symptoms. Sometimes, in more severe cases, ophthalmologists turn to other tests to better understand the underlying pathology. In most cases, physicians provide a routine exam for their patients before moving forward with further testing.
“We actually do a quick, but comprehensive exam to try to look at contributors of patient symptoms that fall under the umbrella of dry eye,” says Anat Galor, MD, an ophthalmologist from the University of Miami Health System in Florida. “We start with an external exam because conditions of the periocular skin can contribute to dry-eye symptoms, such as rosacea and other types of dermatitis. Then, we look at the eyelids and eyelashes because things like anterior and posterior blepharitis can impact symptoms. Then, we look at tear stability, tear production and epithelial disruption. And at the same time, we’re looking for any lumps or bumps, whether it’s on the conjunctiva, such as a pinguecula or pterygium on the cornea, like Salzmann’s nodular degeneration, because any anatomical issue can lead to symptoms of dryness.
“Overall, we call the contributors above nociceptive contributors,” Dr. Galor continues. “What that means is they can trigger corneal (and conjunctival) nerves to fire, and those nerves transmit signals to the brain that lead to a patient feeling dryness, or other unpleasant sensations, in their eyes. But the other situation is that sometimes the nerves themselves become abnormal and contribute to symptoms. And nerve dysfunction can occur in both peripheral and central nerves. If the nerve abnormality is due to a lesion or disease, we call that neuropathic and if we can’t identify a definite lesion or disease, we call it nociplastic. But it really comes down to the nerves being too sensitive. There’s a flip side though, and sometimes the nerves aren’t sensitive enough and don’t respond appropriately to signals on the ocular surface. And these patients can end up with low tear production and corneal staining, and look similar to dry eye from other causes but, in this case, the problem is in the nerves, and we call the condition neurotrophic keratitis. And if that’s not complicated enough, individuals can have a combination of nociceptive, neurotrophic and neuropathic abnormalities happening at the same time. Let’s face it, humans are really complex.”
 |
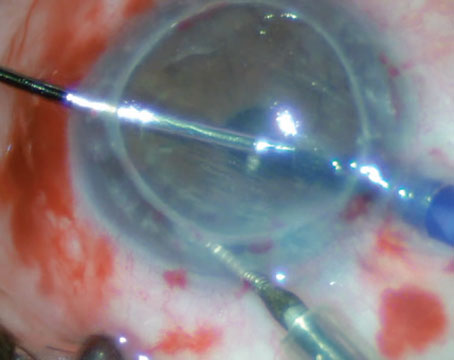
| Though not everyone uses Schirmer’s testing for ocular surface disease patients, some physicians appreciate its ability to help hone the diagosis. Creative Commons License: https://creativecommons.org/licenses/by-sa/3.0/deed.en. |
Yes, humans are complex and that’s a challenge physicians need to face when diagnosing dry-eye cases. So, in order to keep up with the complexity of human biology, it’s best to keep an armamentarium of tests and tools for dry-eye diagnosis and staging. In addition to the slit lamp exam, some physicians also still use Schirmer’s.
“During my initial exam, I like to do a Schirmer’s test,” says Sezen Karakus, MD, an assistant professor of ophthalmology at Johns Hopkins School of Medicine in Baltimore. “I know it’s traditional and not everyone really thinks that it’s necessary, but I still believe that that piece of information is helpful for different reasons. I think it’s important to know if there’s a really low Schirmer’s level and to monitor where we start from and where we move forward. My technician does the Schirmer’s testing, and it might not always be perfectly reliable if it isn’t done properly and if it shows excessive tearing from reflex tearing, or if it touched the cornea.”
In some cases, anesthetic drops are used to help perform the examination. Dr. Karakus finds this useful when conducting a Schirmer’s test as it helps her better determine if Sjögren’s disease is present. “With an anesthetic eye drop, it’s important how you perform the test,” she says. “My technicians know that it has to be placed away from the cornea with closed eyes for five minutes. I believe that piece of information is important. It’s not like I do it every single time that they come back for follow-ups. But at the initial visit, and maybe once a year or if we have further considerations or further suspicions for Sjögren’s or an autoimmune disease, then I’d like to see if it’s changing. And it might be affected by other things too.”
Dr. Galor also uses anesthetic drops in her armamentarium but checks in on her patients following the examination since pain could persist after eye-drop instillation. This assessment is a part of a nerve function test she conducts. “We check corneal sensitivity to look for increased or decreased sensitivity, we assess for persistent pain after anesthesia, which can indicate a central nerve abnormality, and we overall assess whether symptoms and signs align, whether symptoms are out of proportion to signs or whether signs are out of proportion to symptoms,” she says. “And then based on that quick, but comprehensive exam, we tell patients what we think is causing their symptoms and how to best treat it. While all these contributors can fall under the umbrella of dry eye, treatments are different for different contributors.”
Tear osmolarity and MMP-9 testing could be used to help make decisions on what treatment options to employ. Dr. Karakus doesn’t attempt to take an osmolarity measurement during every patient visit, but she finds the information quite useful in some cases. “Tear osmolarity is something I test sometimes,” she says. “Also, though I don’t believe that an MMP-9 test has to be part of a dry-eye exam 100 percent of the time, I occasionally like to use it, too. I don’t do it routinely at the initial visit. I like to have information about whether or not the MMP-9 was positive. So sometimes that helps me make certain decisions with the treatments available. And I might not do it at the initial visit, but at some point, your decision becomes based on what you see, and your experience leads you towards a certain direction in terms of what might be going on.”
Fluorescein and Lissamine
Drs. Galor and Karakus also discussed the staining methods they use and why they use them. Although rose bengal staining is an option, neither of the physicians use this routinely for dry-eye diagnosis.
“Staining is definitely used every single time,” says Dr. Karakus. “So, the slit lamp exam, fluorescein and lissamine green staining are indispensable parts of my exam. Every single patient visit I have to do a full slit lamp exam and full vital dye staining.”
“On my first evaluation, I use fluorescein and lissamine in 100 percent of my patients,” shares Dr. Galor. “Both right at the same time. Fluorescein helps me see the location and characteristics of corneal epithelial staining, highlights tear stability or instability, allows me to assess for anatomic abnormalities like conjunctivochalasis, and highlights the tear lake. Lissamine green helps me look for conjunctival epithelial abnormalities and highlights lid-margin keratopathy.”
Dr. Karakus finds that staining is beneficial for detecting the level of dry-eye severity in patients. Using the SICCA grading scale, she can observe the surface staining to better understand her patient’s condition. “There are different staining grading systems you can easily adapt in the clinic,” she continues, “Oxford and NEI might be a little complicated for day-to-day clinical exams. In clinical studies we use it. But I like to use SICCA because it’s simple, and it gives me enough information when assessing both corneal and conjunctival staining.
“There are different ways to grade using these dyes,” continues Dr. Karakus. “With them, we look for punctate epithelial erosion, which you can see with both dyes. I like to use fluorescein to observe the cornea primarily, but lissamine green gives us more than surface staining. That’s why it’s indispensable for me. So, I use the SICCA grading system to grade the surface staining, which requires both of them, and that’s one of the reasons I use both.”
Dr. Karakus expands on why she finds lissamine green staining important and finds it to be more useful than fluorescein staining: “With my lissamine green, I go ahead and check how the lid margins are stained by the lissamine green,” she explains. “First, that helps me to see Marx’s line. I like to see if we have a regular thin staining with lissamine green. You don’t see it with fluorescein, but you see it with lissamine green. So, if Marx’s line appears regular, large, thickened, and it’s dislocated behind the meibomian gland orifices, or in the opposite way, then those are important signs for us to know whether there’s cicatrizing scarring, conjunctival diseases, if an inflammatory disease might be developing, or if meibomian gland dysfunction is significantly affected.
“In addition, I like to observe the lid wiper area,” Dr. Karakus continues. “I believe sometimes without having significant ocular surface staining, meaning corneal or bulbar conjunctival staining, patients might be very, very symptomatic. And if you didn’t use lissamine green, you would miss the lid wiper epitheliopathy, which is very painful, very uncomfortable, and leads to a burning sensation. The other important thing you would miss if you didn’t do lissamine green is superior limbic keratoconjunctivitis. You have to ask patients to look down and observe the superior bulbar conjunctival area, which isn’t uncommon that you’d see this with lid wiper epitheliopathy in the upper lid, because that’s from friction. The upper lid wiper area is touching for different reasons, but in SLK, we see that the superior bulbar conjunctival area is very loose and staining with the lissamine green shows that every time they blink, they feel that pain.”
Fluorescein staining can be useful, as well. “I think [lissamine green and fluorescein] are both useful and placing them in the eye at the same time is quick and informative,” comments Dr. Galor. “For me, it’s a Venn diagram where there is some overlap in the information you get from the tests, but each gives unique information, so I prefer to do both.”
Severity of Dry Eye
Trying to understand the severity of a patient’s dry eye is difficult, since there are many interpretations on what defines a dry-eye case as mild, moderate or severe. It’s important to figure out a patient’s disease severity in order to make better judgments when choosing treatment options.
Different organizations have attempted to categorize dry eye. For instance, the TFOS DEWS II report, a comprehensive report on defining and diagnosing dry-eye disease, focused on the underlying pathogenesis of dry eye, while other reports, such as the ADES/JDES, emphasized the importance of physicians’ observations when speaking with and assessing their patients.1
“I think it’s definitely a challenge, first of all,” comments Dr. Karakus. “How to categorize dry eye using one single method has been our dream, but it’s never come true. For research studies, you have to define it very well, and you have to use certain parameters, but in my clinical practice, judgments are based on how much signs and/or symptoms are affecting the patient.”
Dr. Karakus shared broad examples of mild, moderate and severe cases of dry eye at her clinic. “If they’re not complaining about dry eye, and they’re okay with basic treatments like warm compresses and using artificial tears as needed, then that’s mild dry eye in my clinic,” she says. “If they’re still complaining, we’ve tried different prescription treatments and we can’t get anything under control, then they’re still suffering, and I ask these questions: ‘Do you think about your dry eye every day? Every day do you think that dry eye is interfering with your daily life?’ If they answer yes, that’s not mild dry eye. That has to be moderate in my case. It could be from the symptoms, it could be from the signs, but it’s affecting this person every day. Severe to me means that the patient is miserable in terms of their symptoms, and/or corneal staining is severe, or maybe they’re on the brink of developing an epithelial defect.”
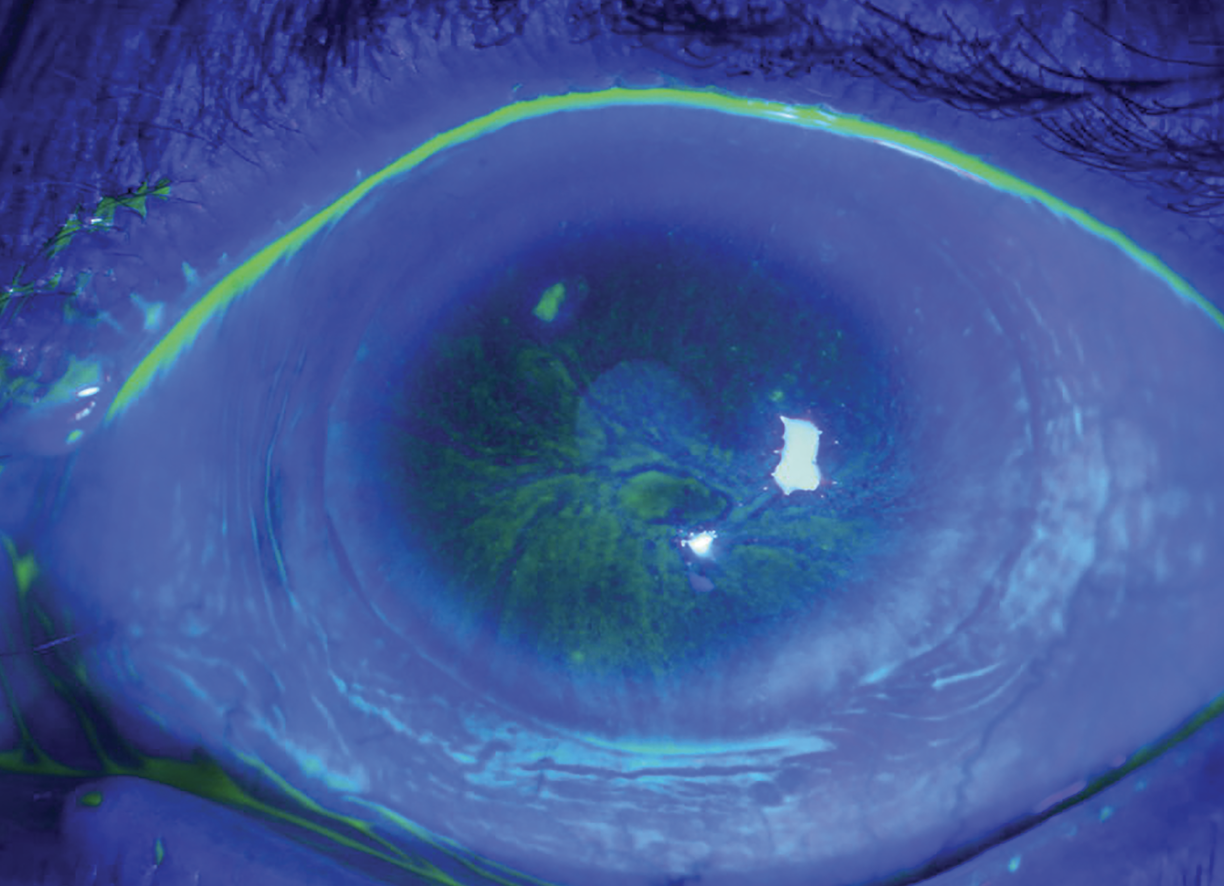 |
| Cobalt blue light is emitted to excite the fluorescein in order to view dry eye signs and symptoms. Dr. Galor uses this form of staining to locate and characterize corneal epithelial staining, highlight tear stability, assess for anatomic abnormalities and highlight the tear lake. Creative Commons License: https://creativecommons.org/licenses/by-nc/2.0/. Photo: Community Eye Health. |
Dry-eye Comorbidities
Dry eye isn’t always alone. There are several comorbidities that can mimic or lead to dry-eye disease. Sjögren’s syndrome, for example, has been mentioned before in this article and Dr. Karakus explained how she uses a Schirmer’s test to help her diagnose these cases. Dr. Galor takes it a step further and provides her patients with questionnaires.
“In patients with Sjögren’s there are some additional questionnaires that we administer, the ESSDAI and ESSPRI, which highlight systemic involvement in Sjögren’s,” Dr. Galor states. “Not all individuals with Sjögren’s look the same and we want to understand how the eye fits in with systemic disease. We work closely with the rheumatologist to deliver multi-specialty care, so understanding the eye/body connection is important.”
Another important comorbidity is conjunctivochalasis. Dr. Karakus uses her vital dyes to assist with the diagnosis of these cases. “Sometimes it’s not easy to understand this condition without using the vital dyes and just looking at the slit lamp,” she explains. “You might not notice the folds. Sometimes it’s very obvious and you’re seeing the folds piling up right in front of the cornea. Those are the easy ones. But with fluorescein or lissamine green, you could actually observe those folds piling up on the lid margin and you could make the connection whether it looks like they’re causing some of the symptoms or problems.”
Drs. Galor and Karakus shared what other comorbidities to look out for, which include inflammatory skin diseases such as psoriasis, eczema and rosacea. They noted that these diseases could set off a chain reaction that could lead to lid margin disease which would lead to meibomian gland dysfunction. It’s best to assess for these skin conditions to avoid future complications with more severe comorbidities.
If a patient were to develop meibomian gland dysfunction, ophthalmologists can inspect this simply by using a slit lamp. But there are other methods that can be used to observe this underlying condition. “Within meibomian gland dysfunction, we have about 10 different metrics that we grade,” says Dr. Galor. “We grade the amount of anterior blepharitis and where the blepharitis is located, it could be at the base of the lash suggesting Demodex as a culprit or mid-lash, suggesting a concomitant skin condition. We look for telangiectasia as a sign of ocular rosacea. We look for keratinization and plugging of the meibomian gland orifices. We squeeze the meibomian glands and look at the quality of the meibum. And then we try to evaluate gland anatomy.
“Sometimes it’s hard to see the gland anatomy with retroillumination,” Dr. Galor continues. “So, we have various devices that use infrared technology to image the meibomian gland. When we don’t see the glands, we describe it as areas of dropout. But it doesn’t necessarily mean the glands are gone. It could simply mean that they’re atrophied, and that is why we don’t see them. But certainly, it means the anatomy isn’t 100 percent. So, this is where some of the advanced imaging technologies can help us. These devices, like the Keratograph, can also help highlight other aspect of tear help, measuring tear stability non-invasively. And that gives you suggestions of whether or not having normal meibomian glands is impacting ocular surface health as a secondary effect.”
“I always pay extra attention to how the lids are closing, because [the action of] lagophthalmos not normally closing well is something you can easily observe without slit lamp examination,” shares Dr. Karakus. “But if you pay close attention, sometimes you see there’s a little bit of an opening and that’s very obvious, so I do like to use fluorescein for that. Sometimes it’s helpful to put the fluorescein in and then ask the patient to close their eyes. Then, using blue light, you could see the staining, so that might give me an idea.
“And then we see floppy eyelids,” continues Dr. Karakus. “We always ask about obstructive sleep apnea and CPAP mask use. I discuss what type of mask they use because some of them might be blowing air into their eyes. If the eyelids aren’t sealing well overnight, then the CPAP exposure is more prominently causing dry-eye symptoms in the morning.”
Patient Comfort is Key
“We’re here for patients,” states Dr. Galor. “So, if a patient tells me, ‘Every time you put a Schirmer’s strip in, I have pain for weeks.’ Then, I just don’t put the Schirmer’s strip in. There’s no reason to cause patients any more discomfort than we absolutely need to. None of these tests beyond the slit lamp are necessary, and we meet patients where they are.”
Patient satisfaction tends to be at the forefront of every clinic, and sometimes the lead up to treatment can be as uncomfortable as the treatment itself. There are many examples for why a patient might be uncomfortable with a slit lamp exam, anesthesia eye drops as well as noninvasive imaging tests.
“Let’s start with slit lamp exam,” begins Dr. Karakus. “With the lights, patients are very light sensitive and it’s really hard to avoid this. But with the compassion that you should have as a physician, I think encouraging them to have a complete exam might give them the answers they’ve been looking for. However, if it’s difficult to withstand the light, of course, you can always adjust it. That’s something you can do.
“Normally, we try to avoid numbing drops like proparacaine,” Dr. Karakus continues. “We try to avoid them because they might make the surface worse, but if they’re going to help with the exam, I might use them sometimes. For staining, patients might not really like it, but I explain it to them how important it is using these dyes to examine their ocular surface. I tell them that’s how we’re going to identify some other things that might have been overlooked.
“Tear osmolarity, for instance, I wouldn’t consider it invasive, but again, with very low tear volume, it might not be easy to collect enough tears for that test to work,” Dr. Karakus adds. “Patients may decline that and that’s okay. Also, imaging tests I wouldn’t consider invasive but, for instance, when examining inflammatory responses, you touch the palpebral conjunctiva on the side of the eyelids. Sometimes patients are very sensitive, and their nerves are probably feeling more than they’re supposed to, and it might not be comfortable to image them. But again, encouraging them, telling them how beneficial this test might be, taking breaks and talking with compassion is always achievable.”
Dry-eye disease is going to continue to affect millions, so the future is going to be focused on improving not only treatment options, but also the examination methods available. This’ll be important to ensure that every patient’s needs are met. “Everyone has to work together with the goal of delivering better care to patients,” comments Dr. Galor. “Drug companies want to sell their product to everyone, of course, but they recognize that their product may not be appropriate for everyone. And it’s in everyone’s best interest to figure out which drug is best for which patient. This way, patients get the therapy or therapies they need with less chair time, less costs and less frustration. It’s a win for everyone.”
Physicians can do everything they can to connect with pharmaceutical companies to develop the next best dry-eye testing device or treatment, but success lies with the attention they give to their patients. “It’s important to focus on the patient as a whole, and how the symptoms and signs correlate is an extra piece of information that’s very important,” mentions Dr. Karakus. “It’s important to look for the overlapping diseases and it’s important to align the patient’s expectations with yours when you talk to them.
“Part of the success of treatment is from how we present the disease to our patients, and we shouldn’t dismiss how the daily activities of patients are affected by this disease that brought them into our chair,” Dr. Karakus continues. “That’s very important, because sometimes we don’t see many signs or symptoms of dry eye, but patients are miserable. We should keep looking before something more serious develops or presents.”
Dr. Karakus is a consultant for Dompé US. Dr. Galor is a consultant for AbbVie, Alcon Vision, Dompé US, and Oyster Point Pharmaceuticals.
1. Shimazaki J. Definition and diagnostic criteria of dry eye disease: Historical overview and future directions. Investigative Ophthalmology and Visual Science 2018;59:14:7-12.