The 2004 conference of the Association for Research in Vision and Ophthalmology held in the last week of April in Ft. Lauderdale, Fla. was larger than ever, and the scientific research encompassed a broad spectrum of topics. Of particular interest to us at this year's conference were the areas of dry eye and allergy. These are two diseases that can often be seen together, or even confused for each other, and represent a large portion of the external ocular conditions we see. Because of this, we've focused this month's column on how papers presented at ARVO advanced our understanding of these diseases' causes, effects and therapies.
Dry Eye
Dry eye is a complex disease with a broad variety of causes and influences. Lacrimal gland dysfunction, lid diseases or abnormalities, Stevens-Johnson syndrome, pemphigoid, alkali burns and neural factors causing decreases in corneal sensation are just a few of the possible underlying pathophysiologies behind dry eye. Environmental conditions, activities such as computer use, and additional physiological factors also interact to result in dry-eye conditions. At ARVO, researchers presented investigations of many viewpoints of dry eye, from measurement to treatment.
• The basics. Researchers evaluated the effect of menopause on the Ocular Protection Index in pre- and post-menopausal dry-eye patients. The OPI quantifies the relationship between tear-film breakup time and the inter-blink interval, where a patient's ocular surface is unprotected when the OPI (the ratio of TFBUT/IBI) is less than 1. When OPI is greater than 1, the ocular surface is protected by the tear film between blinks. In contrast, when the OPI is less than 1 there is greater risk for ocular surface exposure to the environment, resulting in ocular surface damage (Ousler GW, ARVO Abstract #56, 2002). In this population, post-menopausal dry-eye patients have a lower OPI score, putting them at greater risk of exacerbating the signs and symptoms of dry eye (Wilcox KA, ARVO Abstract #79, 2004).
Another study showed that post-menopausal dry-eye patients blink more frequently than their pre-menopausal counterparts when exposed to an adverse environment, as evidenced in a study using the Controlled Adverse Environment model. Researchers believe that this difference in blink rate is due to the shorter TFBUT of post-menopausal women and their decreased ocular surface protection during inter-blink intervals. The higher blink rate may be a compensatory mechanism for protecting the ocular surface against further desiccation (Ousler GW, ARVO Abstract #80, 2004).
As we age, neurotransmitters and enzymes have been shown to be in short supply, decreasing the activity of the nerves and affiliated organs.1 The decrease in these factors may impact the sensitivity of the corneal surface by decreasing its ability to interact with the glands responsible for regulating tear production. Researchers evaluated tear-film stability in a group of dry-eye patients of Ashkenazi Jewish decent. The Ashkenazi Jewish population has a high incidence of familial dysautonomia, a genetic disease known for hereditary sensory and autonomic neuropathies, with effects such as a reduction of corneal sensitivity. The study showed that tear-film stability, measured by TFBUT, decreased with age. This study also showed that gender doesn't affect tear-film stability within this population. This data contrasts with other research that has reported a higher incidence of dry eye in females. Within this specific population of patients, this discrepancy may be due to deficiencies in the neural regulation of the ocular surface that supersede hormonal differences (Lipkin N, ARVO Abstract #78, 2004).
The meibomian gland secretions of infants and adults were compared in one study to determine if the lipid composition of infant meibomian gland secretions could be responsible for the observation that infants blink infrequently when compared with adults. The results of this study suggest that high levels of the triglyceride phosphatidylethanolamine and low levels of free fatty acids may be important in infant tear stability, as these differ in concentration in the meibomian secretions of infants and adults (Shine WE, ARVO Abstract #91, 2004).
 |
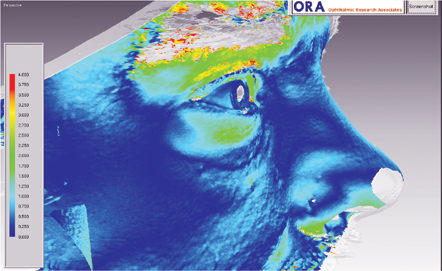 |
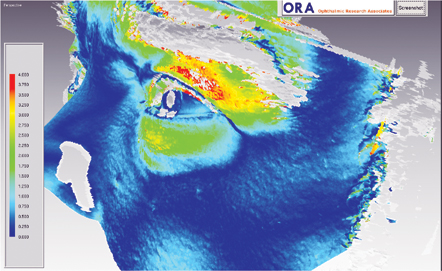
| Lid swelling 15 minutes after allergen challenge (top photo, left eye), and the decrease in swelling observed with olopatadine (bottom image, right eye). Volume increases run from 0 (blue) to 4 (red) mm3. |
Recent dry-eye research has suggested that its pathogenesis has an inflammatory basis. We know that TH2 lymphocytes may induce sustained immune or inflammatory reactions. Researchers at ARVO showed that both TH1 and TH2 lymphocyte mediators induce squamous metaplasia of corneal epithelial cells, which can cause tear-film instability and decreased vision (McNamara N, ARVO Abstract #71, 2004).
• Measurement tools. Researchers are in the process of validating a Dry Eye Quality of Life Questionnaire. The DEQLQ demonstrated the ability to significantly discriminate between a population of normals and patients diagnosed with dry eye, indicating the greatest differences between the two groups were symptoms (dryness, sensitivity to light, discomfort and grittiness) and activities (reading, watching TV/movies, computer use and driving) (Pollard S, ARVO Abstract #82, 2004).
• Therapies. Using in vitro models, researchers identified and compared physical properties such as viscosity and lubricity of various polymers commonly used in artificial tears that could be critical to the tears' performance. HP-Guar (Systane, Alcon) showed high performance in ensuring precorneal retention and reduced friction between the eyelid and corneal surface as compared to hydroxypropyl methylcellulose and carboxymethylcellulose (Ketelson HA, ARVO Abstract #70, 2004).
One study assessed the effect of a lipid-containing tear substitute (Lipovisc [containing carbopol-triglyceride], Bausch & Lomb; available in Europe) in decreasing tear water evaporation, by measuring evaporative stress. Lipovisc significantly reduced evaporative tear loss (Rolando M, ARVO Abstract #3877, 2004).
A rat dry-eye model was used to evaluate the effectiveness of D-3-Hydroxybutyrate, an anti-inflammatory agent, in the suppression of tear fluid proinflammatory cytokines.
Researchers mechanically scraped the corneal epithelium of the rats and then exposed the animals to dehumidified conditions to induce corneal erosion. They treated one eye of each rat with 10 µl of 80mM HBA drops and treated the contralateral eye with a saline drop each hour. Tear samples were collected just before topical application of the test articles.
The researchers found that the concentrations of tear fluid proinflammatory cytokines were suppressed by HBA treatment, suggesting that topically applied HBA could suppress increased proinflammatory cytokines induced by dry-eye conditions in this rat model (Sasanuma K, ARVO Abstract #68, 2004).
One study evaluated the effect of 2% Diquafosol, a P2Y2 agonist which upregulates the production of chloride, and fluid and mucin secretion, in the treatment of dry-eye patients in a controlled adverse environment, a regulated chamber developed at Ophthalmic Research Associates.
Diquafosol was effective in treating the signs, where the percentage of subjects having ocular staining scores of 0 (clear) at week four was significantly higher for diquafosol treated patients than patients receiving placebo. In all dry eyes, diquafosol decreased inferior and central fluorescein staining both pre- and post-CAE exposure. Diquafosol also showed a symptomatic effect in patients with the greatest exacerbation of ocular staining in the controlled adverse environment (Kellerman DJ, ARVO Abstract #3892, 2004).
An in vitro study using human corneal cells evaluated the ability of the ocular steroid rimexolone (Vexol, Alcon) to inhibit cytokine secretion, which promotes inflammation. This study was paired with an in vivo evaluation of the TFBUT and integrity of corneal epithelial cells with rimexolone dosing in a rabbit model of dry eye induced by lacrimal gland inflammation. These studies found that rimexolone was equally as effective as dexamethasone in inhibiting cytokine secretion from epithelial cells. In vivo, rimexolone showed dose-dependent improvements on signs of dry eye, TFBUT and corneal staining, (Gamache DA, ARVO Abstract #62, 2004), suggesting potential for low-dose rimexolone for dry eye associated with ocular surface inflammation.
One study used an interesting model in which dogs with pre-existing, long-lasting keratoconjunctivitis sicca or chronic superficial keratitis were used to evaluate topical 1% pimecrolimus, an agent that interferes with T and mast cells and inhibits pro-inflammatory cytokine production. The exploratory study revealed the potential for treatment of inflammatory eye conditions in dogs, and possibly dry-eye conditions in humans (Nell B, ARVO Abstract #131, 2004).
Allergy
Allergy also saw its share of novel research at this year's ARVO convention. Much of the research centered on the effects of mediators found in the tears of allergic patients. Scientists also presented refinements to study models and designs as well as investigations of anti-allergy therapies.
• Tear mediators. One study used tears collected from patients before and after an induced ocular allergic reaction, then incubated them with conjunctival epithelial cells. Tears from both pre- and post-challenge induced the activation of conjunctival epithelial cells and upregulation of eosinophil adhesion. However, when researchers applied the anti-allergy agent olopatadine (Patanol, Alcon) to patients' eyes before they took pre- and post-challenge tear samples, there was a complete inhibition of these effects (Stahl JL, ARVO Abstract #4839, 2004). If changes such as these, observed in vitro, were to carry over to an in vivo scenario, an anti-allergy agent may have an effect on decreasing allergic inflammation by decreasing the number of eosinophils present at the ocular surface.
Further tear-mediator study examined the differences among atopic keratoconjunctivitis, vernal keratoconjunctivitis, seasonal allergic conjunctivitis, giant papillary conjunctivitis and normal eyes.
This study examined the concentrations of many different proinflammatory cytokines and chemokines using a multiplex bead analysis, which uses a variety of beads, each coated with specific antibodies. Results indicated that specific mediators appear to be characteristic of certain disease types.
For example, IL-8, which can be preferentially secreted as a chemoattractant for migrating eosinophils, lymphocytes and neutrophils, was found to be elevated in the GPC tears. There was elevated IL-5 in VKC, a result consistent with the known recruitment of eosinophils by IL-5 and elevated eosinophils in VKC. Eosinophils also release IL-5 and have prolonged survival in its presence. This study also showed that in SAC there's a significant correlation between the level of disease activity and the measured cytokine levels (Leonardi AA, ARVO Abstract #625, 2004).
Other tear-mediator studies examined the role of prostaglandins, including PGD2, as contributors to the inflammation in severe allergies (Takano Y, ARVO Abstract #4826, 2004), and observation of significantly increased PGJ2 levels in severe allergic conjunctival diseases (Satake Y, ARVO Abstract #4848, 2004).
• Clinical study. Researchers evaluated the mechanisms inducing giant papillae formation and exacerbation of symptoms in the severe allergic conditions AKC and VKC. Excised conjunctival papillae of diseased eyes were compared to conjunctival specimens from normal eyes, revealing that inflammatory infiltrating cell numbers were more than seven times higher in AKC/VKC patients than normals, and thus may be one of the most important factors in tissue remodeling in these severe forms of allergy (Asano-Kato N, ARVO Abstract #4845, 2004).
Study of ocular anti-allergy treatment included a look at olopatadine 0.2%, a novel formulation of olopatadine for which the exhibited duration of action allows for q.d. dosing. Olopatadine 0.2% managed the itching and redness of allergic reaction and proved safe and well-tolerated with q.d. dosing in two studies.
One study was in the conjunctival allergen challenge model, which showed significant decreases in signs and symptoms at 16 and 24 hours, and the other was an environmental study in which the severity of pollen count levels was taken into account using a slope analysis (Greiner JV, ARVO Abstract #4854 2004; Abelson MB, ARVO Abstract #4824, 2004).
Studies of epinastine included a double-masked, multicenter, parallel group, environmental study that indicated ophthalmic epinastine was well-tolerated and at least as effective as ketotifen (Zaditor, Novartis Ophthalmics) (Bonini S, ARVO Abstract #4842, 2004).
Another study was randomized, masked, vehicle-controlled and performed using an allergen challenge. It showed a duration of efficacy for itching of up to 12 hours for eyes treated with epinastine (Friedlander MH, ARVO Abstract #4841, 2004).
One study assessed the three most commonly prescribed antiallergy medications through a review of citations that included these medications, either in comparison or versus placebo. It found that the most well-studied agent was olopatadine (16 randomized studies), followed by azelastine (12) and ketotifen (8). Evidence for drug efficacy was considered strong if there was a p <0.05 or >25-percent difference in responder rate or examiner score; this was the case for 13 of the olopatadine studies, 12 azelastine and five of the ketotifen studies (Potter H, ARVO Abstract #4857, 2004).
• Study design. Several designs of clinical trials were explored at ARVO as well. One model for ocular allergy employs a "cat room," in which cat dander-sensitive individuals are exposed to felines in an enclosed room to induce an allergic reaction, and then researchers assess the relative prevention or relief of the reaction. This room has been tested in studies with anti-allergy therapies including pemirolast (Alamast, Santen), nedocromil (Alocril, Allergan) and olopatadine (Monson BK, ARVO Abstract #4827, 2004; Rothman JS, Abstract #4835, 2004).
However, the cat-room data was presented in the absence of placebo control and without demonstration of clinically meaningful differences. This inhibits our ability to derive meaningful data from this model, which, since its original iteration as the Vienna Chamber,2 has been supplanted by more precise, controllable allergen challenge and environmental models.
Researchers used the conjunctival allergen challenge model coupled with a nasal allergen challenge model to evaluate the relative contributions of the nasal and ocular routes of exposure to the pathophysiology of allergic rhinoconjunctivitis. This study found that when patients were challenged via the nasal route, no meaningful ocular symptoms developed, whereas ocular challenge yielded significant ocular and nasal symptoms. The continual exposure and large surface area of the ocular surface, in addition to the drainage of mediators to the nose, were likely the explanation for the central role of the eye in the allergic rhinoconjunctivitis reaction (Gomes P, ARVO Abstract #4849, 2004).
Clinicians objectively analyzed lid swelling, historically a difficult parameter of allergy to measure accurately. They used three-dimensional scanning to establish baseline topography around the eye and followed it by scanning at set time points after they had induced an allergic reaction (See figure, above). When these two images were superimposed, researchers could calculate the difference in volume to give a measure of lid swelling in mm3. They used positive and negative controls (olopatadine and placebo), and showed significant management of lid swelling with olopatadine, indicating that changes in lid swelling can be quantified using this technology (Gagnon J, ARVO Abstract #4852, 2004).
Currently, our understanding of the allergic mechanism includes activation of ocular H1 and H2 histamine receptors, but one study presented preliminary data evaluating the presence of the H3 receptor on the eye, noting that it may play a role in the lid swelling and chemosis of allergy. Using a guinea-pig model challenged by the mast-cell degranulator 48/80, H3 antagonists resulted in decreases in redness and chemosis (Chapin M, ARVO Abstract #4850, 2004).
Other clinicians also used objective techniques in the evaluation of ocular redness (Ritter MR, ARVO Abstract #486, 2004; Friedlander M, ARVO Abstract #2199, 2004). These computer-assisted redness evaluations present a concept with interesting potential, but are limited at their current stage of development. Future study with such tools will need to address the fact that they only examine a small section of the conjunctiva, rather than the entire surface. In addition, patterns in the location of redness or the vessel beds in which it occurs cannot yet be recognized as well by these computer programs as by human observers.
The ARVO conference, this year more than ever, gave us a chance to appreciate the volume of work being done in dry eye and allergy, leaving us with renewed enthusiasm to continue our explorations in 2005. We hope to see you at next year's meeting.
Dr. Abelson, an associate clinical professor of ophthalmology at Harvard Medical School and senior clinical scientist at Schepens Eye Research Institute, consults in ophthalmic pharmaceuticals. Ms. Wilcox and Ms. Fink are research associates at Ophthalmic Research Associates.
1. Kassinen V, et al. Age related loss of extrastriatal dopamine-2 receptors in women. J Neurochem 2002;81:5:1005-10.
2. Horak F, Jager S, Berger U. Onset and duration of the effects of three antihistamines in current use—astemizole, loratadine and terfenadine forte—studied during prolonged, controlled allergen challenges in volunteers. J Int Med Res 1992;20:5:422-34.



