Post-refractive surgery patients seeking multifocal IOLs may not find encouragement from many doctors. “I don’t do that many multifocal IOLs, only 2 percent of my patients. In people who have had previous refractive surgery I generally discourage it, since I try to get them the best quality of distance vision—which usually was their previous goal—rather than the convenience of decreased reading-glasses dependency,” says James A. Davison, MD, FACS, of the Wolfe Eye Clinic in Des Moines.
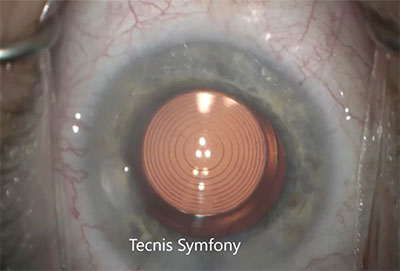 |
| The new Tecnis Symfony, the only extended depth-of-focus lens approved in the United States, is a viable option for patients with a history of refractive surgery who don’t want monofocal lenses. |
Tal Raviv, MD, FACS, associate clinical professor of ophthalmology at the New York Eye and Ear Infirmary of Mount Sinai Icahn School of Medicine at Mount Sinai, and the founder and medical director of the Eye Center of New York, is more willing to use multifocal IOLs in post-refractive patients, but still acknowledges that they are imperfect candidates. “Post-refractive patients are some of the most challenging ones we have,” he observes.
“I have done multifocals in post-refractive eyes, both post-LASIK and -PRK, and I’ll do both hyperopic and myopic previous refractive surgery,” says Daniel H. Chang, MD, of Empire Eye and Laser Center in Bakersfield, Calif. “The fact that they’ve had previous refractive surgery indicates that they obviously do value spectacle independence—or at least at one point they did.”
Since LASIK and its precursors, RK and PRK, are now decades old, the march of time portends that former patients will return to the operating suite with high expectations when cataracts develop. “This is largely an anticipatory issue, because of the certainty of aging,” observes Ming Wang, MD, PhD, of Wang Vision Institute in Nashville, and clinical associate professor of ophthalmology at the University of Tennessee. Dr. Wang estimates that cataract patients with a prior refractive history comprise well over 10 percent of his cases, and he predicts that their numbers will soon increase nationwide. “The LASIK population peaked around 2002, when today’s cataract patients were around 40 years of age. Simple math tells us that a wave of baby-boomer patients is imminent,” he says. “They will make multifocal IOL implantation popular, along with accommodative and extended-range IOLS. There will be a new surge in such procedures.”
For now, though, post-refractive eyes and multifocal IOLs remain a relatively odd couple; succeeding with them requires taking extra precautions during patient screening, workup and counseling.
Develop Exclusion Criteria
The limited literature on such eyes1 looks at small study groups,2 and suggests that while excellent outcomes are attainable, getting there often requires enhancements.3 Despite the shortage of literature on the use of multifocals in post-refractive eyes, Dr. Wang believes it’s only fair that patients seeking such procedures get checked against definitive exclusion criteria. To that end, he has developed a rough preliminary method that helps him eliminate unsuitable eyes by measuring their corneal aberrations against the amount of irregularity that a proposed multifocal lens will tolerate.4
“Multifocal IOLs are extremely picky regarding corneal irregularity, and introduction of a multifocal to such eyes creates higher demand on the cornea,” says Dr. Wang. “The high number of rings in their design corresponds with greater demand on the corneal surface.”
To help identify a potential fit between a given post-refractive cornea and multifocal IOL, he uses a numerical computation to determine the spatial tolerance (ST) of the IOL. He only considers a multifocal if the eye’s spatial precision falls within the lens’s tolerance parameters. Using a +3 D lens as an example, Dr. Wang’s calculation of its ST value (the number of microns of corneal irregularity the lens will tolerate before its performance suffers) would go as follows:
Spatial Tolerance=(diffractive zone diameter-central diffractive zone diameter)/(2 X the number of rings and intervening transition zones).
The lens in the example has a 6-mm diameter optic containing a central diffractive button measuring 0.86 mm in diameter, surrounded a larger diffractive zone that’s 3.6 mm in diameter. Its distance zone goes from 3.6 mm to the outer edge of the optic. The lens has nine concentric rings with nine transition zones between them, creating 18 distinct steps. The ST value would represent the average step size for the lens:
ST=(3.6 mm-0.86 mm)/(2X18)=.0761 mm, or 76.1 µm.
If we compare this lens to a cornea with irregularity measured to be on the order of 250 µm (the SP, or spatial precision value), the eye’s corneal aberrations clearly exceed the tolerance of the multifocal IOL. Unless treatment can decrease the patient’s corneal irregularity to less than 76 µm, the surgeon should use a monofocal or other lens with an ST greater than the cornea’s SP limit.
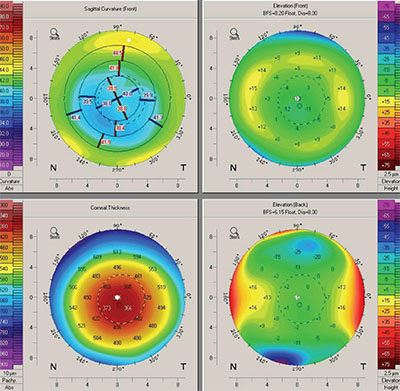 |
| Preoperative corneal topography is especially important in eyes with prior refractive surgery. This topography shows a decentered ablation zone, a contraindication for multifocal IOLs. |
Dr. Wang stresses that his computations represent a rudimentary attempt to develop objective exclusion criteria when dealing with this highly variable patient group. “This post-refractive calculation is an early attempt to match cornea to lens tolerance. There is much work to be done on this approach. It’s still a crude model,” he emphasizes.
The fit between corneal aberration and a multifocal IOL is one factor in visual outcome, influenced by the type of refractive surgery and degree of dioptric correction patients have undergone. “In my experience with hundreds of eyes, generally cases of up to 4 D to 6 D of correction with prior myopic LASIK will be suitable for multifocals,” says Dr. Wang. He notes that he generally doesn’t put multifocals into eyes with a history of RK, early PRK or hyperopic LASIK, although he makes occasional exceptions for hyperopic LASIK corrections no greater than 2 D to 3 D. “As a general concept, most of these cases won’t work with a lens so acutely sensitive to inaccuracy, but doing the calculation provides greater certainty in this assessment,” he states.
Similarly, Dr. Raviv uses multifocal IOLs in select post-refractive patients, the majority with a history of myopic LASIK. “The first thing that I differentiate is patients who have had myopic LASIK versus hyperopic LASIK and RK,” he says. “Radial keratotomy is much more challenging and much more difficult, due to the variation and fluctuation of the vision and the keratometry. I avoid multifocals in those patients at all costs.” Dr. Raviv also considers post-LASIK patients who’ve had a lot of dioptric correction poor candidates for multifocal IOLs. “I would avoid status post high myopia treatment, he says, “but people who’ve had under 5 D of treatment usually do pretty well.”
Dr. Chang, who notes that he is now trending towards Symfony extended-depth-of-focus lenses in post-refractive patients, also avoids multifocals in post-RK eyes, but doesn’t have hard limits regarding other types of previous surgery or degree of dioptric correction. “With post-refractive eyes, it’s a case-by-case basis. Not all LASIK is the same, for example, so you need to consider each case on an individual basis,” he says. Dr. Chang also says that patient response to the prior surgery is important when selecting suitable multifocal patients. “One of the things I always ask patients is, ‘How did you do after your initial LASIK or refractive surgery?’ If they respond, ‘The vision never really cleared up. I had night vision problems and never really liked it,’ that’s a big red flag, because if they had a decentered ablation or some other surgically induced problem, I’m not going to be able to fix that with a lens surgery,” he says. “If they say, ‘It was great! It stayed great for 10 years, but it’s gotten worse recently,’ then that makes me think that their problems are probably cataract-related. I can be a little bit more flexible with my IOL options.”
Rethink the Multifocal Category
“To be successful with multifocals after LASIK, we have to be concerned with some of the higher-order aberrations which are inherent to and created by LASIK, as well as the dysphotopsias that multifocals can create,” says Dr. Raviv. “We didn’t want to combine those in the past, but our lenses have gotten better. Most of our patients who’ve had myopic LASIK have positive spherical aberration in the cornea. The multifocals we have now have negative spherical aberration, so we can treat that,” he continues. “Furthermore, we’ve recently gained the ability to use toric multifocal or toric EDOF lenses. A lot of post-LASIK patients have residual astigmatism, so the newer toric EDOF lenses have allowed us to treat their residual refractive error.”
Dr. Raviv has grown more willing to implant presbyopia-correcting IOLs into post-refractive eyes with the emergence of low-add multifocals and EDOF lenses. “In 2015, we saw the advent of the low-add multifocal. I put those into post-LASIK patients and they did great, with very few nighttime symptoms and very good distance and near vision,” he says. “Now with the [Symfony] EDOF lens, we have a forgiving lens that is tolerant of some residual refractive error, something more likely to occur in a post-refractive eye. These lenses are really more suitable for post-LASIK patients.” Dr. Raviv adds that he regards EDOF IOLs as a subcategory of multifocal IOLs. “In any discussion about multifocals after LASIK, you’ve also got to include EDOFs, because those are the most user-friendly type of multifocal. It’s a subset of multifocal, and they are the lenses that I’m now primarily using,” he says.
Dr. Chang also finds the Symfony’s refractive forgiveness especially helpful in his post-refractive patients. “The jury’s still out,” he says, “but in my hands I’ve seen excellent results.”
Dr. Chang says that when considering an IOL in the post-refractive eye, the avoidance of “splitting light” is not the key factor. “The most important thing to consider is the quality of the image you’re putting on the retina,” he says. “When you look at some modeling and benchtop trials, the lenses that correct spherical aberration and chromatic aberration actually produce better image quality.”
Counsel Carefully
Dr. Chang intensifies his preoperative counseling a little when post-refractive surgery patients want presbyopia-correcting IOLs—in part because their prior results are generally so good. “With any patient, counseling is critical, but especially for post-refractive patients; their expectations may be high from LASIK, which has done well for a lot of people. You have to make sure they know what to expect,” he says. He advises patients that in addition to refractive misses, they may be at higher risk for quality-of-vision issues. “Sometimes, prior hyperopic LASIK may work against them, for example, because most of our multifocal lenses are negatively aspheric,” he says.
Although post-LASIK patients can enjoy excellent results with multifocal IOLs, Dr. Raviv is also careful to give patients a preoperative dose of realism. “We don’t promise them complete, 100-percent glasses independence,” he says. “We shouldn’t do that with any multifocal patient. I don’t mind the super type-A-triple-plus patients, because we read them the riot act, and they know what they’re getting into,” he continues. “We tell them, ‘This is the best technology we can give you: This is your eye. We’re going to match the two and do what we can. If you hate it, we’ll take it out and put in another lens, but you’re limited to this or that. That’s all we have. I’m offering you the best we’ve invented.’ ”
For patients who insist on sharp near vision for reading or other close work, Dr. Raviv will use low-add multifocals. “I’ll use the Tecnis ZKB00,” he says. “It’s one of the lowest adds of the multifocals, so there’s a very low incidence of optic phenomena with that lens.”
Measuring and Operating
Dr. Chang’s preop workup of these patients differs from that for typical cases mainly in the amount of attention to corneal topography. “I’ll always review the topography a lot more closely in my previous refractive surgery patients. I’m using the Atlas topographer right now, which allows me to assess what the refractive surgery did, to make sure that the treatment zone size is good, that the centration is good and that there’s no irregular astigmatism,” he says. His preop presbyopic workup also includes a standard eye exam, biometry with the IOLMaster 700 and macular OCT with the Cirrus SD-OCT.
Dr. Raviv also doubles down on topography. “For those patients, I’m getting two sets of topographies,” he says. “One is a standard placido disk topographer and the other is a topographer that helps me measure the posterior corneal astigmatism, and therefore the total corneal astigmatism, more accurately.”
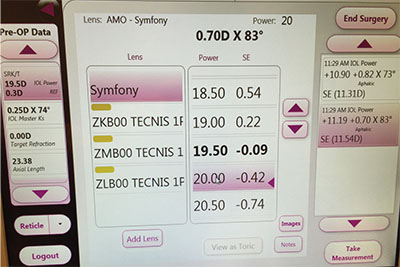 |
| Intraoperative aberrometry can aid in multifocal IOL selection in eyes that have undergone refractive surgery, which are notorious for unpredictable IOL implantation outcomes. |
The second pillar of Dr. Raviv’s lens-selection strategy is interoperative aberrometry. “You just have to check off a box on the ORA indicating post-myopic LASIK, or post-hyperopic LASIK, so it feels a little bit like cheating,” he says. “I find that by combining the formulas I use with the ORA, I get very close. I use it with all my post-refractive cases and all of my multifocal patients; so certainly, with multifocal post-refractive cases I’m using ORA.”
While he doesn’t use intraoperative aberrometry, Dr. Chang is another fan of the ASCRS calculator for post-refractive eyes for preop measurements. “Warren Hill, Doug Koch and Li Wang have done a fantastic, amazing job putting that out there as a resource,” he says. “Typically for presbyopic IOLs, I will look at multiple scans and compare their consistency. That’s obviously trickier if I’m manually entering data into the ASCRS Web site, but I do use the multiple scans to make sure there’s a fair amount of consistency among them.”
In surgery, Dr. Raviv is careful to avoid LASIK flaps when implanting any IOL. “When I’m operating, I’m always very cognizant of where the edge of the flap is. You want to make your incisions away from the flap and just stay out of its way. It’s usually not a problem, and the surgery is otherwise quite the same as it is for traditional patients,” he says.
Have a Plan B
In a patient group where both expectations and the potential for suboptimal outcomes run high, you must also be prepared to act when multifocal IOLs prove unsatisfactory. “You need to have the skills, the wherewithal and the ability to correct any unhappy patients, whether it’s because of dysphotopsia or because of residual refractive error,” stresses Dr. Raviv. “If it’s residual refractive error, you have to be ready to do one of three things: PRK touch-up or LASIK enhancement; IOL exchange; or toric rotation.” Although suboptimal outcomes are atypical if patients are carefully selected and worked up, Dr. Raviv acknowledges, “It’s much more likely for them to happen in post-refractive multifocal patients than in traditional cataract cases.”
When unhappy multifocal IOL patients present themselves, Dr. Raviv teases out the cause. “One of the simplest things to do is make sure it’s not residual refractive error. The post-LASIK eye may be more sensitive to even 0.5 D or 0.75 D of this. In the unhappy multifocal patient, is it posterior capsule opacification, or is it the lens itself? If it’s PCO, we want to address that early,” he says. “If they are immediately unhappy early on, I want to address their residual refractive astigmatism. The easiest way to do that is to put on a trial contact lens that corrects them to plano, even if it’s just -0.5 D. Some people will come back after a day or two and say it’s perfect, and then I’ll just do a touch-up on their cornea.”
“If there’s a postoperative refractive error, my patients have been prepped beforehand to understand that there’s a higher-than-normal chance for that,” notes Dr. Chang. His next step “depends upon how unhappy the patient is,” he says, adding that he offers enhancements after waiting three to six months for the refraction to stabilize. Dr. Raviv also watches and waits for the refraction to stabilize in these cases. “For patients who are still unhappy, I’m going to wait three months,” he says. “If it’s not better, then I’ve got to do something, whether it’s explantation or something else. I’m happy to wait, unless the patient is miserable. A lot of these lenses do get better in three months.”
For a carefully selected group of patients who have had refractive surgery in the past, some surgeons say that multifocal IOLs can provide customized visual results that monofocals can’t. Although it takes careful screening, a scrupulous preoperative workup and perhaps extra time in follow-up, such care can reap rewards in terms of patient satisfaction. “Post refractive surgery patients have already invested financially in their vision, and they want to continue the good-quality uncorrected vision they have already achieved when they undergo cataract surgery,” says Dr. Raviv. “We’ve come a long way, and we now have many ways of making these patients happy.” REVIEW
Dr. Davison is a consultant for Alcon. Dr. Raviv is a consultant for Abbott, Ocular Therapeutics and Glaukos, and is a paid speaker for Bausch + Lomb and Shire. Dr. Chang is a consultant for Carl Zeiss Meditec AG and Abbott. Dr. Wang reports no financial interest in any products or procedures discussed in this article.
1.Khor WB, Afshari NA. The role of presbyopia-correcting intraocular lenses after laser in situ keratomileusis. Curr Opin Ophthalmol 2013;24:1:35-40.
2.Alfonso JF, Madrid-Costa D, Poo-Lopez A, Montes-Mico R. Visual quality after diffractive intraocular lens implantation in eyes with previous myopic laser in situ keratomileusis. J Cataract Refract Surg 2008;34:11:1848–1854.
3.Muftuoglu O, Dao L, Mootha VV et al. Apodized diffractive intraocular lens implantation after laser in situ keratomileusis with or without subsequent excimer laser enhancement. J Cataract Refractive Surg 2010;36:11:1815-21.
4.Wang M. Multifocal IOLs for post-LASIK patients: Establishing clinical guidelines for patient selection. Refractive Eyecare 2012;16:6:1-4.



