The Patient’s Complaint
Evaluation of eyelid and brow position is an important part of an ophthalmologist’s external exam. The tissues of the eyebrow and eyelid are functionally linked, and changes in the position of one will affect the form and function of the other. Patients will often have concerns about their eyelids drooping, and it’s only through a careful exam that one can determine whether that complaint is caused by blepharoptosis, dermatochalasis, brow ptosis or a combination of these factors. While ophthalmologists often take note of ptosis and dermatochalasis as part of a general eye exam, brow ptosis is more likely to be overlooked.
The relationship between eyelid and brow position is complex, and it’s clear that the eyelid and brow are structurally and functionally connected. So, just as when you’re evaluating a patient’s complaint, remember that performing surgery on one without consideration for the effects on the other is a recipe for an unsatisfied patient. A review of the literature suggests that surgery to correct blepharoptosis results in brow descent,1-3 and how significant this change will be to the patient functionally or aesthetically will differ in each case. Blepharoplasty alone can also lead to a significant drop in brow position, though studies addressing this topic have reached mixed conclusions.1,4-8
If your exam determines that the patient has mild to moderate brow ptosis, and you’d like to avoid issues associated with formal brow lifts, consider the following options.
Direct Brow Lift
One option for these brow ptosis patients is a direct, or transcutaneous, brow lift.9,10 The advantages of this procedure are that it’s relatively simple to perform, gives the surgeon good control of the amount of lift and has the ability to address medial brow ptosis. The main drawback of this procedure is the resultant scar above the brow. In our experience, a lateral brow lift can be achieved with a reasonable scar, although when the incision is carried more medially the scar become significantly more apparent.
When using this procedure to elevate the male brow it’s important to pay particular attention to the contour, taking care to preserve a flatter brow and avoid a feminizing, highly arched brow. Several techniques have been described to try and improve the appearance of this scar, including beveling the incision, sutured lifting of the orbicularis to relieve tension, and postoperative scar treatments.11,12 Meticulous surgical techniques can improve the appearance of the scar, but for a portion of patients any scar can be cosmetically unacceptable. Additionally, there is also the possibility of significant paresthesia of the forehead, especially if the supraorbital nerve and vessels are not meticulously protected against damage during the procedure.
External Browpexy
This technique, first described in 2012 by Beverly Hills, Calif., surgeon Guy Massry, MD,13 provides a moderate lateral brow lift through a small incision.
To perform external browpexy, the surgeon marks the point of desired brow elevation near the junction of the tail and body of the brow, then makes a small, 8-mm incision just superior to the brow cilia. Dissection is carried through the skin and subcutaneous tissues close to the level of the periosteum. The dissection is carried superiorly to the level of desired
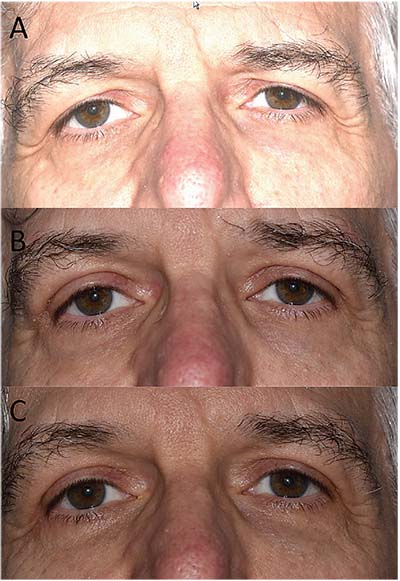 |
| Blepharoplasty and external browpexy, pre- and postop. Preoperative photo (A): Notice significant lateral brow ptosis and dermatochalasis. Postoperative photo, two weeks after blepharoplasty and external browpexy (B): Notice some redness in the area of the incisions over the lateral brow. Postoperative photo, two months after surgery (C): Notice the improved appearance of the external browpexy incisions. |
The procedures we’ve discussed so far involve an incision superior to the brow. While this type of incision results in some amount of scarring, it has the advantage of making it possible to perform these brow- lifting procedures in isolation from other periorbital procedures. This allows for correction of brow ptosis or asymmetry without making an upper-eyelid incision. The remainder of the techniques that we will discuss are most appropriately performed concurrently with blepharoplasty and take advantage of the standard blepharoplasty incision.
Internal Browpexy
The internal browpexy is an effective procedure that can provide a moderate lift to the lateral brow. It is not the ideal procedure for patients with severe brow ptosis or those with significant medial brow ptosis. The main advantage of this procedure is that it’s performed through the blepharoplasty incision, which usually heals very well with minimal scarring. It’s important to note that the browpexy will elevate the brow to a more appropriate position, causing a resultant stretching of the upper eyelid skin and less redundancy of the upper eyelid skin. Care must be taken to avoid removing too much skin from eyelids that are having a concurrent brow-lifting procedure, in order to avoid lagophthalmos and accompanying corneal complications.
In the preoperative area, it’s helpful to mark the point of desired elevation near the bottom of the brow cilia at the junction of the tail and body of the brow with the patient in an upright position. Once the blepharoplasty incision is made, the dissection is carried superiorly over the orbital rim in a pre-periosteal plane to a level 15 to 20 mm above the orbital rim. The surgeon then places a suture at full thickness through the skin and subcutaneous tissues at the mark made preoperatively; this pass serves as a marking
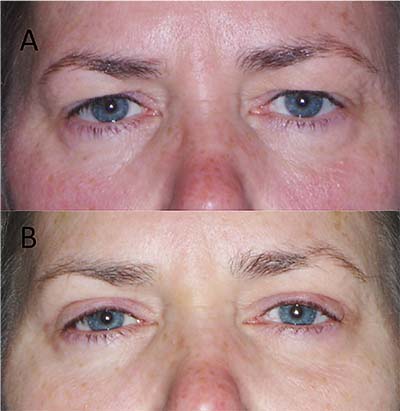 |
| Preoperative photo before blepharoplasty and brassiere suture (A) demonstrates the upper eyelid skin fold obscuring the central and lateral tarsal plate. Postop (B), note the elevated brow and preserved lateral tarsal show. |
Complications of this procedure include pain at the suture site, which usually resolves over a few weeks. There is also the possibility of creating an unsightly dimple in the brow skin if the browpexy suture is passed too superficially.
Brassiere Suture
The goal of this procedure is to use the orbicularis to suspend the brow fat pad and create a barrier to the descent of the brow tissues. As a result, this procedure can provide volumization and aesthetically pleasing anterior projection of the lateral brow and help to preserve the contour of the lateral superior sulcus. For patients who complain of skin covering their lateral tarsal plate, this procedure can produce an excellent aesthetic result.
Like the internal browpexy, this procedure also takes advantage of a previously made blepharoplasty incision. After the blepharoplasty incision has been made and the skin excised, the surgeon incises the orbicularis and divides it into roughly equal-sized upper and lower portions. Dissection under the superior portion of the orbicularis is carried to the level of the orbital rim. An absorbable suture is then used to secure the cut end of the upper orbicularis to the underlying arcus marginalis, effectively creating a sling or hammock for the brow tissues above. You can place several sutures along the lateral rim. The incision is then closed by standard techniques. This technique and several variations have been previously described17–19 and, though it can provide a lift for the brow fat pad and improved brow volume at the level of the orbital rim, in our hands it doesn’t provide a significant lift to the overall brow. Therefore, patients with more significant brow ptosis would likely be better served by a different procedure.
Small-incision brow-lifting techniques such as those discussed here provide good, minimally invasive ways to address brow ptosis. A variety of available techniques allow for personalization of the surgical approach to each patient, depending on his or her needs and concerns. REVIEW
Drs. Broadbent, Mokhtarzadeh and Harrison practice in the departments of Ophthalmology and Visual Neurosciences at the University of Minnesota. Dr. Harrison is also affiliated with the departments of Otolaryngology and Head and Neck Surgery at the University. Please address any correspondence to Andrew R. Harrison, MD, MMC 493, 420 Delaware St., SE, Minneapolis, MN 55455, or email him at aharrison@umn.edu.
1. Lee JM, Lee TE, Lee H, Park M, Baek S. Change in brow position after upper blepharoplasty or levator advancement. J Craniofac Surg 2012;23:2:434–6.
2. Moore GH, Rootman DB, Karlin J, Goldberg RA. Mueller’s muscle conjunctival resection with skin-only blepharoplasty: Effects on eyelid and eyebrow position. Ophthal Plast Reconstr Surg 2015;31:4:290–2.
3. Rootman DB, Karlin J, Moore G, Goldberg R. The effect of ptosis surgery on brow position and the utility of preoperative phenylephrine testing. Ophthal Plast Reconstr Surg 2016;32:3:195–8.
4. Prado RB, Silva-Junior DE, Padovani CR, Schellini SA. Assessment of eyebrow position before and after upper eyelid blepharoplasty. Orbit 2012;31:4:222–6.
5. Nakra T, Modjtahedi S, Vrcek I, Mancini R, Saulny S, Goldberg RA. The effect of upper eyelid blepharoplasty on eyelid and brow position. Orbit 2016;35:6:324–7.
6. Hassanpour SE, Khajouei Kermani H. Brow ptosis after upper blepharoplasty: Findings in 70 patients. World J Plast Surg 2016;5:1:58–61.
7. Baker MS, Shams PN, Allen RC. The quantitated internal suture browpexy: Comparison of two brow-lifting techniques in patients undergoing upper blepharoplasty. Ophthal Plast Reconstr Surg 2016;32:3:204–6.
8. Frankel AS, Kamer FM. The effect of blepharoplasty on eyebrow position. Arch Otolaryngol Head Neck Surg 1997;123:4:393–6.
9. Tyers AG. Brow lift via the direct and trans-blepharoplasty approaches. Orbit 2006;25:4:261–5.
10. Pelle-Ceravolo M, Angelini M. Transcutaneous brow shaping: A straightforward and precise method to lift and shape the eyebrows. Aesthet Surg J. 2017 Mar 16 (epub ahead of print).
11. Lee JW, Cho BC, Lee KY. Direct brow lift combined with suspension of the orbicularis oculi muscle. Arch Plast Surg 2013;40:5:603–9.
12. Feinendegen DL, Constantinescu MA, Knutti DA, Roldán JC. Brow reduction, reshaping and suspension by a 20-degree beveled brow incision technique. J Craniomaxillofac Surg 2016;44:8:958–63.
13. Massry GG. The external browpexy. Ophthal Plast Reconstr Surg 2012;28:2:90–5.
14. Mokhtarzadeh A, Massry G, Bitrian E, Harrison A. Quantitative efficacy of external and internal browpexy performed in conjunction with blepharoplasty. Orbit. In Press.
15. McCord CD, Doxanas MT. Browplasty and browpexy: An adjunct to blepharoplasty. Plast Reconstr Surg 1990;86:2:248.
16. Cohen BD, Reiffel AJ, Spinelli HM. Browpexy through the upper lid (BUL): A new technique of lifting the brow with a standard blepharoplasty incision. Aesthet Surg J 2011;31:2:163–9.
17. Briceño CA, Zhang-Nunes SX, Massry GG. Minimally invasive surgical adjuncts to upper blepharoplasty. Facial Plast Surg Clin North Am 2015;23:2:137–51.
18. Zarem HA, Resnick JI, Carr RM, Wootton DG. Browpexy: Lateral orbicularis muscle fixation as an adjunct to upper blepharoplasty. Plast Reconstr Surg 1997;100:5:1258–61.
19. Armstrong BK, Sobti D, Mancini R. Partial orbicularis resection for the augmentation of traditional internal browpexy: The “Tuck and Rise.” Ophthal Plast Reconstr Surg 2016;32:6:473-476.



