|
|
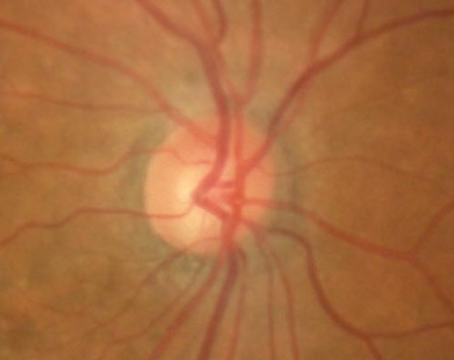
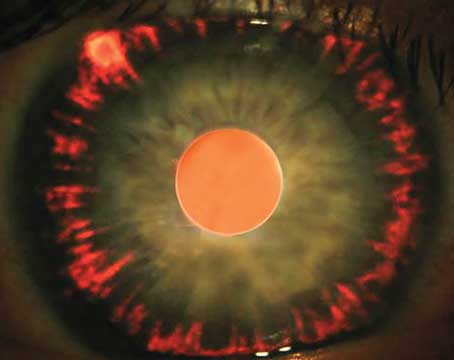
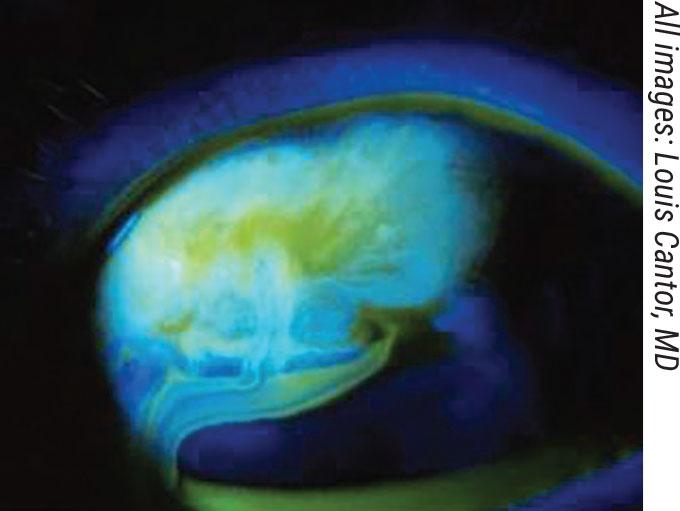
A bleb leak is a possible complication of bleb-forming procedures such as trabeculectomy, Xen and PreserFlo. |
Trabeculectomy has been performed successfully for many years to reduce both intraocular pressure and the number of medications required to maintain a healthy pressure. Newer procedures, such as the Xen Glaucoma Treatment System (Abbvie/Allergan) and PreserFlo Ab-Externo MicroShunt (Santen), are also options for managing glaucoma, but patient selection is key. In this article, glaucoma specialists explain how they decide between the procedures.
According to Louis B. Cantor, MD, who is in practice in Indianapolis, there are very limited data to help surgeons make patient selection decisions. “Patient selection for not only these but our other MIGS procedures is still evolving rather rapidly and is often done without good evidence, simply because we don’t have a lot of good data. The limited studies we have are retrospective or case series,” he explains.
“Part of the goal of the device-based procedures, such as Xen and PreserFlo, was to standardize trabeculectomy and to minimize some of the complications of a bleb-forming procedure. However, Xen has evolved to include many variations in technique. It was originally designed to be performed as an ab interno procedure through clear cornea and injected translimbally and subconjunctivally. But now, people are doing a lot of open conjunctival dissections, applying mitomycin in different ways and doing primary needling at the time of surgery to prevent or minimize the risk of tube occlusion, which is not an uncommon complication. PreserFlo is done using an external approach, so I think the techniques for doing it are more standardized. Trabeculectomy techniques can vary widely between surgeons. There are many individual techniques, and there is a lot of art to trabeculectomy,” Dr. Cantor explains.
Trabeculectomy
The effectiveness and safety profile of trabeculectomy are well-known, as it’s been a mainstay for surgeons who need a procedure that gives them a significant amount of pressure lowering and who are willing to go a more invasive route.
Data from the landmark Tube vs. Trabeculectomy study bear this out. In the trial, with follow-up at 17 clinical centers, 105 patients with a history of prior cataract extraction and/or failed filtering surgery underwent trabeculectomy with mitomycin C. They were evaluated for IOP, visual acuity, use of supplemental medical therapy and rate of failure. At five years postoperatively, their mean IOP was 12.6 ±5.9 mmHg, and they were on 1.2 ±1.5 glaucoma medications. The probability of failure during the five years of follow-up was 46.9 percent, and the rate of reoperation was 29 percent.1
Recently, researchers have taken a look at the results of these procedures in patients without a history of surgery, in the Primary Tube vs. Trabeculectomy study. As part of the study, 117 glaucoma patients underwent trabeculectomy with MMC. The researchers found that the cumulative probability of failure after three years was 28 percent in the trab group. Postop IOP was 12.1 ±4.8 mmHg at three years, and the average number of postop glaucoma medications for patients in the trab group was 1.2 ±1.5. Serious complications requiring reoperation or producing a loss of two or more Snellen lines developed in nine trabeculectomy patients (8 percent).2
According to Michael Stiles, MD, who is in practice in Overland Park, Kansas, the lowest pressures can be obtained with a trabeculectomy. “In patients who need a super-low pressure with no medication dependence, I prefer trab. I use Xen for all other patients. It’s my go-to filtration procedure for most patients because, if it scars or if it doesn’t succeed, there’s still a lot of real estate left to do a trabeculectomy. In fact, another indication for a trabeculectomy is a failed Xen procedure. Many times, I’ll perform trabeculectomy prior to doing a traditional tube shunt,” he says.
Dr. Cantor agrees. “If you do a lot of trabeculectomy, I still feel that it’s the most effective procedure overall, and you can manage the safety concerns. You also don’t have that additional cost initially, because there’s no device to pay for. For those patients at highest risk of going blind, who have refractory glaucoma that’s failed other things, and for younger patients, I certainly lean toward trabeculectomy. And I strongly lean toward trabeculectomy in patients who have a high risk of significant loss of vision, loss of quality of life, or visual impairment during their lifetime because of where they are in the spectrum of their glaucoma,” he says.
Richard A. Lehrer, MD, who is in practice in Alliance, Ohio, also believes that trabeculectomy with mitomycin-C is best for achieving very low pressures. “If a patient needs single-digit pressures reliably, the best way to get there is with a trabeculectomy. However, if a patient needs pressures in the low teens, procedures like Xen and hopefully PreserFlo will be able to achieve that. The problem with Xen in my hands is that the success rate is significantly lower than with a trabeculectomy. I explain to patients that the risk of performing a Xen is lower than the risk of doing a trab, but the chance of failure is higher,” Dr. Lehrer explains.
If he only has one chance to achieve the necessary pressure, Dr. Lehrer will most likely choose a trab. “The Xen has a 25- to 30-percent rate of needling, and of those needlings, only about 50 percent are successful in my hands,” Dr. Lehrer adds.
Xen
The Xen gel stent is a 6-mm hydrophilic flexible tube with a 45-µm lumen. It is made of porcine collagen-derived gelatin cross-linked with glutaraldehyde, which is non-inflammatory and causes minimal extraocular fibrotic or vascular response to the implant material. The Xen decreases IOP by creating a permanent drainage shunt from the anterior chamber to the subconjunctival space through a scleral channel.
The design of the Xen stent is based on the principles of laminar fluid dynamics. The Hagen-Poiseuille equation was used to calculate the required internal dimensions of a tube that would prevent hypotony at an average aqueous humor production of 2 to 3 µL/min, and would provide a steady-state IOP floor of approximately 6 to 8 mmHg.

|
|
Bleb-associated infection, or “blebitis” after a trabeculectomy. |
The FDA approved Xen in 2016 for use in POAG and pseudoexfoliative or pigmentary glaucoma in eyes with open angles that are unresponsive to maximum tolerated medical therapy.
“All-in-all, what I like about the Xen, especially with an ab interno approach, is that about 50 percent of the time you can achieve a very good long-term IOP with a quick procedure. With a trab, the healing time is longer, and the chance of early and late complications is probably a little bit higher,” Dr. Lehrer says.
Dr. Cantor adds that it can be worthwhile to consider Xen or PreserFlo in patients who are refractory to medications and laser who don’t have advanced glaucoma. “Maybe we’ve even done a MIGS procedure, such as a canal-based procedure, and we’re still not controlling pressure adequately, and the patient can’t use or can’t tolerate medications or the medications are not effective. We may not want to put that patient in the position of having a trabeculectomy at their stage of disease or at their age, so it’s worthwhile to consider Xen or PreserFlo,” he says.
According to Dr. Cantor, some surgeons suggest that Xen and PreserFlo may be contraindicated in patients with a history of angle-closure glaucoma. “You need to have somewhere to place the tube in the eye that isn’t too close to the cornea. In those eyes, you can often do a trabeculectomy because you’re doing an iridectomy. With time, we’re going to learn where these procedures work best and don’t work relative to each other. But currently, we don’t have a lot to go on other than personal experience and limited data,” he says.
PreserFlo
The PreserFlo, which is currently pending Food and Drug Administration approval, is composed of poly(styrene-block-isobutylene-block-styrene), which is biologically inert and has been used in coronary stents. The properties of this material are expected to decrease the risk of postoperative episcleral scarring and fibrosis, which are often causes of surgical failure after glaucoma filtering procedures.
The design of the device is based on assumptions of the Hagen-Poiseuille equation for prediction of pressure. The device’s maker says that as long as aqueous production is 2 µL/min or more, postoperative intraocular pressure should be maintained above 5 mmHg. When positioned properly, the distal end of the MicroShunt should filter aqueous to the subconjunctival and sub-Tenon’s space 6 mm posterior to the limbus, allowing for posteriorly directed flow and bleb formation.
This device looks promising. In fact, a recent study found that PreserFlo MicroShunt and Xen Gel Stent implantations achieved comparable results in primary open-angle glaucoma in terms of IOP-lowering and surgical success, with a similarly high safety profile.2
This was a retrospective, comparative case series of primary open-angle glaucoma patients with at least six months of follow-up after a MicroShunt or Xen implantation augmented with mitomycin C. (In terms of disclosures, one of the researchers received research grant support from Santen, one was an Allergan consultant and another was a consultant for Santen.)
Forty-one eyes of 31 patients underwent Xen implantation, and 41 eyes of 33 patients underwent PreserFlo MicroShunt implantation. Baseline characteristics were similar, except for more combined surgeries with phacoemulsification in the Xen group (37 percent) compared with the PreserFlo group (2 percent). Mean baseline IOP ± standard deviation decreased from 19.2 ±4.4 to 13.8 ±3.8 mmHg (n=26) in the Xen group and from 20.1 ±5.0 to 12.1 ±3.5 (n=14) in the PreserFlo MicroShunt group at 24 months of follow-up. Additionally, the number of IOP-lowering medications dropped from 2.5± 1.4 to 0.9± 1.2 in the Xen group and from 2.3± 1.5 to 0.7± 1.1 in the PreserFlo MicroShunt group. The researchers determined that the probability of qualified success at 24 months was 73 percent in the Xen group and 79 percent in the PreserFlo MicroShunt group. Postoperative complications were usually mild and self-limiting in the study, and the number of bleb needling and secondary glaucoma surgery procedures was similar in both groups.
Dr. Lehrer says that one advantage of PreserFlo is that it may not have the issues with hypotony that Xen has. “PreserFlo doesn’t expand as it hydrates, whereas the cross-linked gelatin in Xen does expand, so there can be leakage of aqueous around the stent. So, I think a potential advantage of the PreserFlo is a lack of early hypotony, and I always caution patients after a Xen to take it easy. There should be no lifting, bending, straining or Valsalva maneuvers for at least the first week. In a good Xen procedure, we’re typically going to see single-digit pressures for the first couple of days,” Dr. Lehrer says.
According to Dr. Stiles, experience overseas suggests that PreserFlo may achieve lower intraocular pressures than Xen. “PreserFlo may be another alternative if you’re trying to avoid a trabeculectomy in patients who need a low pressure,” he says. “I do see some early hypotony the first week with the Xen because there can be some flow around the tube. In comparison, the PreserFlo device fits into a snug pocket. I tend to avoid Xen procedures in certain patients with high opening pressures and in those at risk for choroidal hemorrhage that can occur with early hypotony.”
The hope with PreserFlo is that surgeons will be able to achieve lower long-term pressure with less medication dependence than Xen and avoid the first week of hypotony. “It also has advantages over trabeculectomy in that trabeculectomy requires many postop visits in which you are manipulating outflow by cutting or removing flap sutures to avoid failure and hypotony at the same time,” Dr. Stiles says. “There’s just a lot of postop care involved, and not all patients can make it to the office six or eight times within the first six weeks to monitor progress. Both Xen and PreserFlo have this advantage over trabeculectomy; however, I’m more likely to have episcleral fibrosis issues with Xen compared to trab, and there’s more need for some medication dependence. I’m hoping PreserFlo is an improvement upon that, but time will tell.”
Dr. Stiles has received research support from AqueSys, which was acquired by Allergan, and Santen. Dr. Cantor has consulted for Allergan and Santen. Dr. Lehrer has no financial interest in any of the products mentioned in the article.
1. Gedde SJ, Schiffman JC, Feuer WJ, et al, Tube versus Trabeculectomy Study Group. Treatment outcomes in the Tube Versus Trabeculectomy study after five years of follow-up. Am J Ophthalmol 2012;153:5:789-803.
2. Gedde SJ , Feuer WJ, Lim KS, et al. Treatment outcomes in the Primary Tube Versus Trabeculectomy study after 3 years of follow-up. Ophthalmology 2020;127:3:333-345.
3. Scheres LMJ, Kujovic-Aleksov S, Ramdas WD, et al. Xen gel stent compared to PreserFlo MicroShunt implantation for primary open-angle glaucoma: Two-year results. Acta Ophthalmol 2021;99:3:e433-e440.
Suggested Reading
Batlle JF, Corona A, Albuquerque R. Long-term results of the PreserFlo MicroShunt in patients with primary open-angle glaucoma from a single-center nonrandomized study. J Glaucoma 2021;30:3:281-286.