 |
Alpha Hydroxy Acids
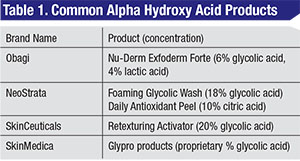
Chemicals that can be used for peels can be used at much lower concentration with daily application. As discussed in the first part of this series, “Chemical Peels Demystified,” in the October issue of Review, alpha hydroxy acids (See Table 1), including glycolic acid derived from sugarcane, cause superficial exfoliation by keratinocyte discohesion at the level of the stratum granulosum in the epidermis with resulting improvement in skin texture.1 AHAs can be combined with retinoids to accelerate skin turnover from 28 days to 10 to 12 days in preparation for subsequent chemical peels.1 Glycolic acid products can be used as daily skin-care products at concentrations as low as 5 to 15%.
Vitamin C
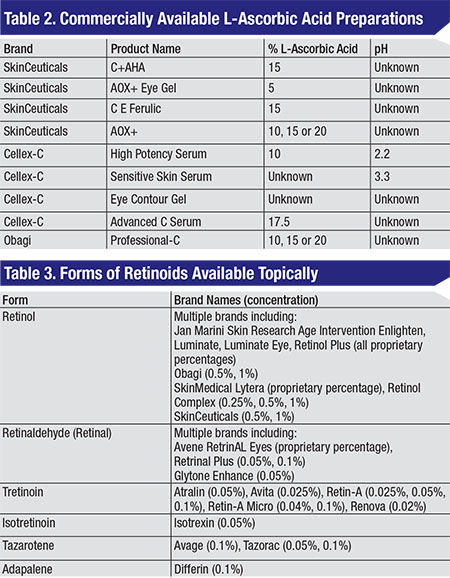
Vitamin C, or ascorbic acid, is a well-studied antioxidant for the treatment of photodamaged skin. The effects are thought to occur via transcriptional upregulation of collagen synthesis, scavenging of reactive oxygen species, and inhibition of elastin biosynthesis and tyrosinase to reduce elastin accumulation and pigment synthesis, respectively.2,3 Unlike most plants and animals, humans cannot synthesize ascorbic acid; it must be obtained via diet or topical application.3 However, oral ingestion of ascorbic acid doesn’t provide adequate replenishment of skin ascorbic acid stores. Due to difficulty in stabilization, a topically absorbed version of L-ascorbic acid has only recently been available.4 Topical L-ascorbic acid can be used to alleviate skin inflammation from ultraviolet light exposure, as well as erythema from laser resurfacing procedures.4 A porcine study demonstrated that best skin absorption of L-ascorbic acid occurs at a pH less than 3.5 and a concentration of 20%, with minimal absorption of L-ascorbic acid derivatives such as magnesium ascorbyl phosphate, ascorbyl-6-palmitate and dehydroascorbic acid. Higher percentages of L-ascorbic acid failed to increase absorption.5 The mean time to clinical improvement of skin texture is one month of daily application, and the mean time to improvement of coarse rhytids, telangiectasias, pigmentation, keratoses, sallowness and histological collagen deposition is three months.4,6
Retinoids
Retinoids are a family of vitamin A-related compounds that have been used topically and orally since the 1940s for a multitude of skin conditions, primarily acne.7 Their ability to rejuvenate photoaged skin was popularized in the 1980s.7 They are thought to reduce wrinkles by increasing type I procollagen expression and inhibiting dermal collagen degradation in the upper papillary dermis.7,8 Skin texture is improved by increasing epidermal proliferation and differentiation, compacting stratum corneum, thickening of the granular layer, and increasing epidermal and dermal glycosaminoglycan deposition.7,8 There is evidence that pretreatment with a retinoid for at least two weeks prior to chemical peels can reduce post-peel inflammation, improve peel uniformity and accelerate re-epithelialization.7 Topically applied retinol (vitamin A, all-trans-retinol) is converted into retinaldehyde and subsequently into the active metabolite retinoic acid (tretinoin) by dehydrogenases in human keratinocytes.9 Active stereoisomers 9-cis-retinoic acid (alitretinoin) and 13-cis-retinoic acid (isotretinoin) as well as adapalene, tazarotene and seletinoid G are applied in their active form.7
 |
Optimized dosing consists of balancing efficacy and side effects. The dose-dependent retinoid reaction that usually occurs early in the treatment course consists of erythema, scaling, xerosis and pruritis.7 The most important predictive feature of those likely to suffer the retinoid reaction is sensitive skin, such as Fitzpatrick type 1; historical intolerance of other topical agents; those with a tendency for skin flushing, exposure to large amounts of cosmetics; or skin with other conditions such as eczema, rosacea or seborrheic dermatitis.7 Although the retinoid reaction subsides, it’s seen in the majority of patients using 0.05% tretinoin and in approximately 90 percent of patients using 0.1% tretinoin.7 Long-term use of tretinoin (over 11 months) has shown no difference in outcomes between higher (0.05%) and lower (0.01% or 0.02%) concentrations.7,10
Given the topical instability of retinol and the side-effect profile of tretinoin, there are a slew of retinol esters and derivatives. Of these, retinaldehyde (0.05% to 0.1%) may have comparable performance to tretinoin (0.5%) with more limited side effects.7,8 There is no evidence at this point to support the use of other retinoids, including retinyl-palmitate, retinyl-propionate and retinyl-acetate.7
 |
| Classic retinoid reaction with erythema, scaling and xerosis from use of topical retinol daily for a week. This was treated by stopping the cream and starting 1% hydrocortisone until symptoms resolved. |
Dr. Kleinberg practices comprehensive ophthalmology and oculoplastics at Worcester Ophthalmology Associates in Massachusetts. She can be reached at 25 Oak Ave., Worcester, MA 01605; Tel: (508) 521-2010; e-mail: terikleinberg@gmail.com.
1. Clark E, Scerri L. Superficial and medium-depth chemical peels. Clin Dermatol 2008;26:2:209.
2. Pinnell S. Cutaneous photodamage, oxidative stress, and topical antioxidant protection. J Am Acad Dermatol 2003;48:1:1-22.
3. Farris P. Topical vitamin C: A useful agent for treating photoaging and other dermatologic conditions. Dermatol Surg 2005;31:S1:814-818.
4. Traikovich S. Use of topical ascorbic acid and its effects on photodamaged skin topography. Arch Otolaryngol–Head & Neck Surgery 1999;125:10:1091-1098.
5. Pinnell S, Yang H, Omar M, et al. Topical L-ascorbic acid: Percutaneous absorption studies. Dermatologic Surgery 2001;27:2:137-142.
6. Fitzpatrick R, Rostan E. Double-blind, half-face study comparing topical vitamin c and vehicle for rejuvenation of photodamage. Dermatol Surg 2002;28:3:231-236.
7. Hubbard B, Unger J, Rohrich R. Reversal of skin aging with topical retinoids. Plast Reconstr Surg 2014;133:4:481e-490e.
8. Fathi R, Pfeiffer ML, Tsoukas M. Minimally invasive eyelid care in dermatology: Medical, laser, and cosmetic therapies. Clin Dermatol 2015;33.2:207-216.
9. Pilkington S, Belden S, Miller R. The Tricky Tear Trough: A Review of Topical Cosmeceuticals for Periorbital Skin Rejuvenation. J Clin Aesthetic Dermatol 2015;8:9:39.
10. Manaloto RM, Alster T. Periorbital rejuvenation: a review of dermatologic treatments. Dermatol Surg 1999;25:1:1-9.
Suggested Reading:
Chen L, Hu J, Wang S. The role of antioxidants in photoprotection: A critical review. J Am Acad Dermatol 2012;67:5:1013-1024.
Clark C, Rohrich R. Skin care in an aesthetic plastic surgery practice: Indications and scientific rationale. Perspect Plast Surg 1994;8:01:159-169.



