LASIK: Time-tested and Sophisticated Technology
LASIK’s precision and customization can improve vision for a wider range of patients.
By Avneet K. Sodhi-Gaur, MD, Los Angeles
 |
Since its introduction in the 1990s, LASIK has gone through several generations. LASIK’s origins stem from the use of a microkeratome to manually cut a thin-hinged corneal flap, which was quite thick at the time—much thicker than what they are now—and an unguided excimer laser would sculpt the cornea.
The next iteration of LASIK involved the use of an Intralase femtosecond laser to create a microscopically thin flap, which helped preserve more corneal tissue and made the procedure a more viable option for many who were once deemed poor candidates. I’d say the third generation began with the Contoura (Alcon), approved in 2015, which gave us more advanced techniques for sculpting the cornea using topography to guide and customize patients’ vision. We’re moving even further in the scope of the technology now with wavefront-guided LASIK that can capture thousands of points on your eye to create a precise treatment plan.
With these advancements, the outcomes are getting better and studies prove this. In the FDA trials for the Contoura platform, 68.8 percent of patients achieved 20/16 or better UCVA at three months post-surgery, and 31.6 percent achieved 20/12.5 or better.1 The iDesign Refractive Studio (Johnson & Johnson Vision), approved in 2018, achieved a UDVA of 20/16 in 74.1 percent of eyes in one study.2 There have also been fewer postoperative complaints of light sensitivity, issues with night driving, halos, glare and other visual aberrations that were common in previous generations of LASIK.
Even with LASIK’s impressive results, surgeons and patients are always on the lookout for something new with more advantages. The newest contender is SMILE performed with the VisuMax femtosecond laser (Zeiss). Even though SMILE is in its relative infancy as a go-to refractive procedure, it can produce results similar to advanced LASIK—but it’s not without its issues and considerations. Understanding the advantages of each procedure is crucial for selecting the best patients for each procedure.
Advantages of LASIK
LASIK can be used to treat a wide variety of patients with myopia, hyperopia and astigmatism. This makes it inherently advantageous because it makes more people eligible for the procedure. Some other advantages of LASIK are:
• Proven track record. One of the advantages of LASIK is that it’s been around a long time, with tens of millions of procedures having been performed. It has had a chance to evolve and mature in its technology translating into different generations of LASIK offered throughout the years. Also, when you combine its familiarity with the solid long-term data of risk and complications and how to deal with those, it’s not surprising that the majority of refractive surgeons continue to gravitate to LASIK technology. Granted, even though SMILE was approved in the United States in 2016, it has made large, advantageous strides in the advancements in its technology since then.
• Faster vision recovery. LASIK patients are typically seeing at their full visual potential one day after surgery. When SMILE was initially approved in the United States, there were higher femtosecond energy levels used, which therefore equated to significantly slower vision recovery and took a few weeks to get patients to their visual endpoint. However, in 2018, Zeiss adjusted the energy levels to where the lenticule creation didn’t cause as much of an OBL (opaque bubble layer); therefore, allowing more ease of lenticule dissection and providing significant improvement in vision recovery. Although SMILE doesn’t provide as consistent postoperative day one vision as LASIK does, it has made significant improvement over the years since its introduction.
• Versatility is wider with LASIK. Currently LASIK can correct a wide range of refractive errors, including myopia, hyperopia and higher degrees of astigmatism. SMILE is currently only approved for patients with -1 to -10 D of myopia and -0.75 to -3 D of astigmatism in the United States, however up to -5 D of astigmatism outside the U.S. Even though SMILE can be performed in low refractions, some refractive surgeons have found the lenticule can be so thin it can easily tear when trying to remove it, leaving higher risk of lenticule debris and hindering visual outcomes.
• Refractive results/enhanced precision. Because LASIK is performed with the excimer laser which is designed for precise sculpting, versus the femtosecond laser in SMILE, designed for cutting, the excimer laser combined with wavefront technology delivers highly customized vision correction treatments coupled with reproducible results.
In a 2023 study looking at patient-reported quality of vision in a prospective randomized contralateral-eye trial comparing LASIK and SMILE, it demonstrated that, of 40 patients who underwent wavefront-guided LASIK in one eye and SMILE in the fellow eye, there were slightly better outcomes with wavefront-guided LASIK compared to the SMILE surgery. Additionally, there were greater gains of lines of best-corrected visual acuity in the wavefront-guided LASIK group compared to the SMILE group and subjectively at the postoperative month 12 visit, 17 of 37 participants preferred the vision from the eye that underwent LASIK compared with seven of 37 who underwent SMILE.3
The advanced LASIK technologies, such as wavefront-guided or wavefront-optimized treatments, allow for highly customized corneal reshaping with iris registration and adjustment for cyclotorsion, all of which improve refractive outcomes by reducing glare and starburst and hone in on reducing higher order aberrations.
However, with SMILE there were concerns with the machine’s limitation in the United States with post-docking adjustments, accounting for cyclotorsion and centration leading to decentered treatments. In response to industry and surgeon feedback, Zeiss incorporated adjustments into its next generation Zeiss VisuMax 800 that was FDA approved in January 2024. The VisuMax 800 will have the ability to center over the pupil to prevent decentered treatments and account for cyclotorsion to improve its astigmatism correction.
• Simplicity of LASIK enhancements. In LASIK, it’s easy and familiar to do a touch-up. We just lift the flap when possible and perform a retreatment. However, in SMILE, you simply can’t repeat the SMILE surgery. There are few enhancement techniques possible after SMILE, and the decision to choose which to perform is dependent not only on what can be performed but also the surgeon’s comfort. In the United States, the SMILE cap thickness is defaulted at 120 µm, so you can make an ultra thin LASIK flap between 90 to 95 µm in the SMILE cap, however, it only gives you approximately 25 to 30 µm of corneal tissue to sculpt with the excimer laser, which is very limited. Another choice is to perform a side cut and open up the original 120-µm SMILE cap and convert that into a LASIK flap.
A final choice is to perform PRK on top of the SMILE cap. We frequently resort to PRK enhancement in these situations, especially since many of our SMILE enhancement patients actually come from China where the technology differs, including the SMILE cap not having a default preset as it is in the United States. Therefore, the desire to do a LASIK enhancement becomes less straightforward in these patients.
Recognizing SMILE’s Potential
SMILE is certainly a procedure to watch. As it evolves in the future, it will find its niche in the refractive world and will have a more widespread adoption among refractive surgeons. But I think it still has some more finessing to do. SMILE is a good form of refractive surgery for simple forms of myopia and limited astigmatism. We’re more limited in the United States with it because internationally they can treat some hyperopic prescriptions and higher astigmatism prescriptions. Still, I’d say SMILE is for a certain niche of patients who might not be candidates for an ICL, don’t want to deal with the long recovery of PRK or have a history of dry eye.
One area where SMILE may outperform LASIK is with the dry eye aspect. We know SMILE patients experience less postoperative dry eye because it disrupts fewer corneal nerves and patients heal faster than LASIK, however, when followed for six months, there’s no difference in dryness symptoms in the two groups.4
In addition, the newest generation of LASIK technology, which we’re using in our practice, addresses some of the dry eye symptoms by customizing the flap size, hinge length and hinge position to disrupt fewer corneal nerves. Developed by Kerry Assil, MD, EAGLE (Elliptical flap aberrometry-guided laser enhanced) Vision LASIK incorporates iDesign wavefront technology and a customized elliptical-flap for each individual eye. Because each eye is different, we believe the flap should be different for each patient, and this allows us to customize the positioning of the flap hinge and where it’s located. Some smaller studies suggest that flap hinges positioned temporally or nasally preserve corneal nerves, and therefore decrease dry-eye rates.5 There needs to be a large study to validate this data.
While LASIK remains the dominant procedure in the United States due to its extensive history, proven outcomes and versatility, SMILE presents a promising alternative with its flapless approach and potential benefits in corneal biomechanics and dry-eye management. And as femtosecond technology continues to improve so will its refractive results with SMILE.
Ultimately, I think the adoption of SMILE in the United States has been slow due to two reasons: Firstly, the limitation of the current technology’s ability to customize treatment plans compared to outside the United States; and, secondly, because the technology is evolving rather quickly with SMILE, for refractive surgeons it’s difficult to stomach the cost of a technology that could possibly be deemed obsolete in a matter of a year.
Therefore, since SMILE is still in its infancy compared to LASIK, it’s truly not a fair comparison as it still needs to mature the way LASIK did over 30 years, with various refinements and technological advancements.
Dr. Sodhi-Gaur is a cataract and LASIK specialist and partner at the Assil Gaur Eye Institute of Los Angeles.
1. FDA Clinical Trials. Allegretto Wave Eye-Q Addendum Procedure Manual T-CAT Topography-Guided Treatments. http://www.accessdata.fda.gov/cdrh_docs/pdf2/P020050S012d.pdf. Accessed June 13, 2024.
2. Johnson & Johnson Vision Launches Next Generation of Personalized LASIK Treatment, iDESIGN Refractive Studio Now Available. Sept., 6, 2018. https://www.jjvision.com/press-release/johnson-johnson-vision-launches-next-generation-personalized-lasik-treatment-idesign. Accessed June 13, 2024.
3. Ma KK, Manche EE. Patient-reported quality of vision in a prospective randomized contralateral-eye trial comparing LASIK and small-incision lenticule extraction. J Cataract Refract Surg 2023;1:49:4:348-353.
4. Wong AHY, Cheung RKY, Kua WN, Shih KC, Chan TCY, Wan KH. Dry eyes after SMILE. Asia Pac J Ophthalmol (Phila) 2019;8:5:397-405.
5. Feng YF, Yu JG, Wang DD, Li JH, Huang JH, Shi JL, Ye T, Wang QM, Zhao YE. The effect of hinge location on corneal sensation and dry eye after LASIK: A systematic review and meta-analysis. Graefes Arch Clin Exp Ophthalmol 2013;251:1:357-66.
SMILE: Holding its Own Against LASIK
Direct comparisons of SMILE’s first-generation technology to the advanced LASIK platforms are unfair.
By Majid Moshirfar, MD, Draper, Utah
 |
Small-incision lenticule extraction is one type of refractive lenticule extraction (ReLex). It’s also the newest laser vision correction technique, and was approved by the FDA in 2016 for the correction of myopia ranging from -1 D to -8 D and astigmatism up to 3 D in individuals aged 22 years or older. The procedure involves the creation of a thin disc of tissue on the cornea with the femtosecond laser (Zeiss Visumax platform). This lenticule is then removed through a small incision.
Studies have shown that SMILE produces comparable visual results to femtosecond LASIK, as well as better outcomes in terms of dry eye, contrast sensitivity and induced aberrations at three months. In 2016, a single-center, prospective, randomized study of patients with myopia who underwent either FS-LASIK or SMILE had an equal amount of eyes in each group (84 percent) achieve a UCVA of 20/20 at three months, while 12 percent of eyes in the SMILE group and 4 percent in the LASIK group achieved 20/15. Higher order aberrations were higher in the LASIK group at three months, and postop dry eye and glare were more common following LASIK, according to the study.1
Along with my co-authors, we published a study in 2018 comparing SMILE to the different generations of LASIK.2 We looked at 68 eyes that underwent SMILE surgery and collected their preop and postop UDVA, CDVA, manifest sphere, manifest cylinder, intraoperative complications, and preop and postop visual symptoms. We compared these to three early generation LASIK platforms (1999 to 2000) and three of the most recent at the time (2013 to 2016).
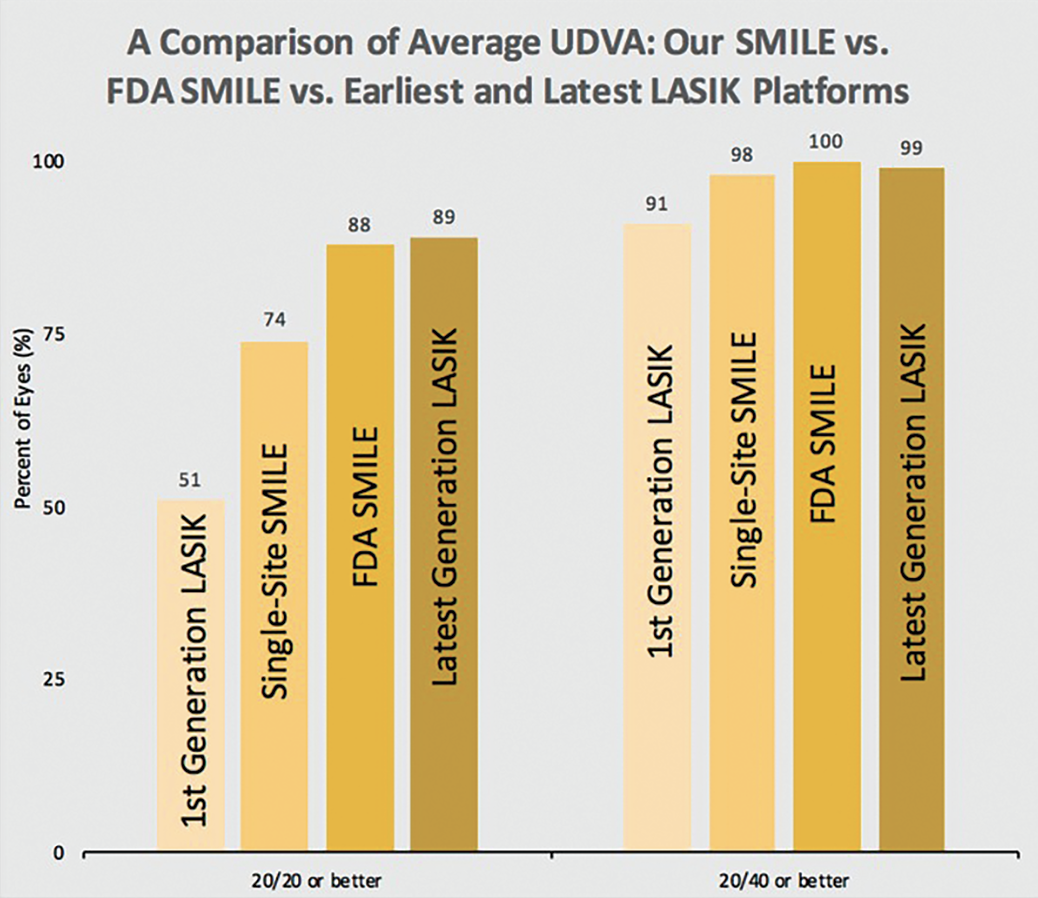 |
| We compared the average UDVA between our single-site SMILE results to the results of the FDA SMILE trial and the earliest and latest excimer platforms for LASIK. As a first-generation technology, SMILE outperformed the first generation of LASIK and overall its results were competitive with the latest LASIK platform at the time. Photo Credit: Majid Moshirfar, MD. |
SMILE had significantly more eyes seeing 20/20 or better UDVA (74 percent), and 20/40 UDVA (98 percent), compared to 51 percent and 91 percent, respectively, in the early LASIK group. The numbers were better in the updated excimer laser group, with 89 percent seeing 20/20 or better and 99 percent seeing at least 20/40. That shows how close SMILE was coming to LASIK even as a brand-new technology.
To me, this demonstrates the fault in comparing SMILE directly to LASIK, which has had further evolution into topography- and wavefront-guided technology. LASIK is a mature technology. SMILE is still young. That would be like comparing a chef who has just graduated from culinary school to a renowned and experienced chef who has received a Michelin star. It’s just not a fair comparison.
In the United States, it hasn’t even been a decade since SMILE’s approval. If someone says that LASIK is better than SMILE, then they must be talking about topography-guided LASIK, which we know has spectacular results and achieves 20/15 and 20/10 vision for patients. We know that contrast sensitivity and higher order aberrations are reduced with topography-guided platforms, but in the first- and second-generation LASIK platforms, there was a tenfold increase in higher order aberrations. LASIK can’t claim that it doesn’t induce any higher order aberrations now, but it does induce much less. It’s not quite fair to compare the latest, state-of-the-art LASIK platforms with SMILE. However, the younger SMILE is doing quite well and I believe it will surpass topography-guided LASIK in some ways in a matter of the next few years. Here’s why:
Statistical Similarities
We recently conducted a contralateral study of 42 patients who underwent Contoura LASIK (Alcon) in one eye and SMILE on the Visumax 500 (Zeiss) in the other and presented data at ASCRS Boston 2024. In terms of safety index, efficacy, three-months uncorrected visual acuity, three-months best corrected visual acuity and gain/loss of vision, SMILE and LASIK are statistically the same.
But keep in mind, this study used the SMILE Visumax 500 platform that was the only one available in the United States at the time, which has a lot of limitations. This platform can’t do centration, cyclotorsion, iris registration or pupil tracking. However, all of those capabilities exist with topo-guided LASIK, not to mention vertex compensation and 3D mapping that has the ability to correct for higher- and lower-order aberrations. LASIK can also correct for 0.25 and 0.50 of cylinder, yet SMILE can’t do any of those things. So here we have a SMILE platform that’s still at its young stage, but is going head to head with topography-guided LASIK.
Many people mention that LASIK has a faster recovery time than SMILE, and when we look at our data at one day and one week postop, it’s true LASIK patients recover more quickly. Yet there’s no difference at one month and three months. So why don’t SMILE patients recover as quickly? Well, we’ve been limited in the energy we can use in this country. The ability to optimize the energy, change the spot size or the line separation would—I believe—help SMILE surpass LASIK. Yet, my hands are tied. I can’t correct for astigmatism that’s less than 0.75. I can’t do iris registration or cyclotorsion, or track the pupil. There’s no tracking mechanism and we have to trust that the patient is looking at the light.
This past January, the FDA approved the Visumax 800. The new platform creates the lenticule in less than 10 seconds and has more energy, plus enhancements that include centration, cyclotorsion adjustment and user nomograms. We’ve been refining LASIK nomograms for years. I have close to 12,000 eyes in my LASIK nomogram, ranging from age 20 to age 55, so I can tweak the sphere, reduce the cylinder, etc., all of those factors based on years of results. We know how to treat a 40-year-old who needs a -6 D correction with 2 D of astigmatism. On the other hand, I only have about 1,200 eyes for SMILE, so there’s not as much ability to refine it with regard to regression over time, the longevity of the refractive error, etc. We need more data to create nomograms based on patients’ age and correction.
I think all of the corneal refractive technology platforms are great, and I use all of them, but when you look at SMILE, you can understand that we’ve only been using its first-generation technology. We haven’t even gone to the second generation. Imagine what’s going to happen when we have more refinement.
Advantages of SMILE
Putting all of that aside, SMILE has several advantages over LASIK.
• No flap. SMILE creates a cap that’s only about 7 or 7.5 mm, and the incision itself is only about two to three clock hours. The LASIK flap is 8 to 8.5 mm and the incision goes all the way around 11 clock hours. You’re violating the anterior corneal architecture more tangibly. With SMILE, there’s a lesser degree of protrusion into the anterior one-third of the cornea than with LASIK because we don’t create that flap with 10 or 11 clock hours of side cut with a hinge of two or one clock hours. In SMILE, we just make a cap and go underneath this cap through a very small incision to remove the lenticule.
• A better effective optical zone. When comparing the ablation of the excimer laser vs. the lenticule you create with SMILE, the effective optical zone is slightly better with SMILE. When you look at the topographies of SMILE patients weeks, months or years later, the effective optical zone area is bigger.
• Better visual outcomes for high myopia. Study after study has shown that SMILE has slightly better visual outcomes than LASIK when it comes to high myopia.3 Many of the topo-guided LASIK platforms can’t correct for high myopia, but SMILE can correct up to -13 D.
• One machine. LASIK requires a femtosecond machine and an excimer laser. SMILE just uses one femtosecond laser for both cuts. This helps save space in a surgical suite. Also, from a maintenance point of view or for surgeons in developing countries, it’s much more attractive to have one platform.
• Patient selection. Patients who are involved with contact sports such as martial arts are often not candidates for LASIK because of the risk of blunt injury and flap dislocation. SMILE is stronger biomechanically and suits that lifestyle more appropriately. Additionally, patients who have lagophthalmos do better with SMILE. There’s less risk of developing dry eyes because there’s no flap exposed by the eyelid. I’ve also treated a patient with Bell’s palsy who never recovered and I recommended SMILE in the Bell’s palsy eye.
Why Learn SMILE?
One of the things I hear people say is “I’m happy with my LASIK results, why do I need to offer SMILE?” It reminds me of when cataract incisions became smaller and people wondered why they needed to go from 3.2 mm to 2.4 mm. The fact is, we’re always refining our surgical technique and we should have all surgical options in our armamentarium. If you’re truly a corneal refractive surgeon as your primary focus, you need to advocate for ReLex procedures. If someone argues that they don’t want to use SMILE for myopic astigmatism or hyperopic astigmatism, and they only want to use LASIK, I feel that’s not a good mindset because this technology is going to influence so many facets and they need to have their hands in it.
Lenticule surgery and femtosecond lenticule creation aren’t going away. As a matter of fact, in the future we may have the ability to do corneal augmentation with this same type of platform. We may be able to take the lenticule of someone who is -6 and use it in an individual who is +6. I truly believe that the principles of lenticule removal and harvesting will not only impact corneal refractive practices, but will impact the eye-bank industry.
Ultimately, nothing is black and white. There are some patients for whom I truly believe SMILE is by far the better option, and there are some patients for whom I’ll choose LASIK. Any good clinician who wants to dedicate their practice to refractive surgery should not only be able to do LASIK, but also SMILE, PRK and other techniques that we have access to.
Dr. Moshirfar is the medical research director at Hoopes Vision Research Center in Draper, Utah, and director of the Refractive Surgery Program at the John A. Moran Eye Center, University of Utah.
1. Ganesh S, Gupta R. Comparison of visual and refractive outcomes following femtosecond laser- assisted LASIK with SMILE in patients with myopia or myopic astigmatism. J Refract Surg 2014;30:9:590-6.
2. Moshirfar M, Murri MS, Shah TJ, Linn SH, Ronquillo Y, Birdsong OC, Hoopes PC Jr. Initial single-site surgical experience with SMILE: A comparison of results to FDA SMILE, and the earliest and latest generation of LASIK. Ophthalmol Ther 2018;7:2:347-360.
3. Qian Y, Chen X, Naidu RK, Zhou X. Comparison of efficacy and visual outcomes after SMILE and FS-LASIK for the correction of high myopia with the sum of myopia and astigmatism from -10.00 to -14.00 dioptres. Acta Ophthalmol 2020;98:2:e161-e172.