Refractive technology continues to evolve, offering more options as well as the potential for improved patient outcomes. Small incision lenticule extraction, which received FDA approval in 2016, is a safe and effective procedure that achieves a refractive change by creating a lenticule-shaped piece of tissue with the VisuMax femtosecond laser (Carl Zeiss Meditec) and then removing it from the cornea with forceps rather than making a flap and ablating tissue like LASIK. Today, there are a number of new procedures in development that aim to improve upon this approach. Here, surgeons share their experiences with these new refractive surgery techniques while also discussing how they compare to currently available options and the potential impact on ophthalmic practice.
 |
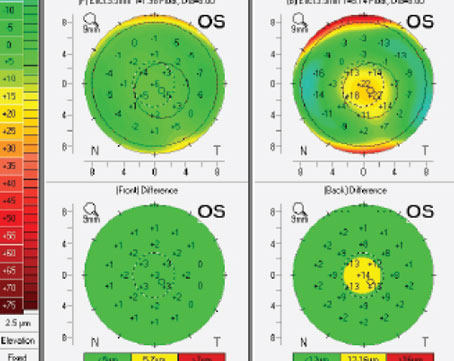
| Figure 1. SmartSight is a minimally invasive lenticule extraction procedure developed using the Schwind ATOS femtosecond laser. Pictured here is the laser making the refractive cut. (Courtesy Kishore Raj Pradhan, MD) |
Small-Incision Lenticule Keratomileusis (SILK)
SILK—a surgical procedure developed by Johnson and Johnson Vision—uses a new femtosecond laser (Elita) to treat myopia and compound myopic astigmatism by removing a thin lenticule of stromal tissue from the cornea.
The procedure, which uses a technique similar to SMILE, can treat patients with myopia and compound myopic astigmatism with up to 10 D of myopia and up to 5 D of astigmatism, according to Edward E. Manche, MD, a professor of ophthalmology and director of the Cornea and Refractive Surgery Service at Stanford University School of Medicine.
Internationally, SILK has been tested in India and Singapore with positive results. The Elita femtosecond laser system received CE Mark approval in March.1 This procedure isn’t approved in the United States; however, the FDA trial was recently initiated by Dr. Manche and colleagues. While data is limited, preliminary results are promising, with most patients experiencing excellent vision in the early postoperative period similar to results seen with LASIK surgery, he notes.
While discussing how SILK stands out compared to currently available options, Dr. Manche notes that this new procedure has a number of unique differences when compared to SMILE.
“The SILK procedure on the Elita femtosecond laser allows adjustment for centration over the entrance pupil as well as cyclotorsion control on the operating screen,” he explains. “It’s a very high-speed laser which operates at 10-MHz level compared to the kilohertz levels of current femtosecond laser systems used for SMILE surgery.
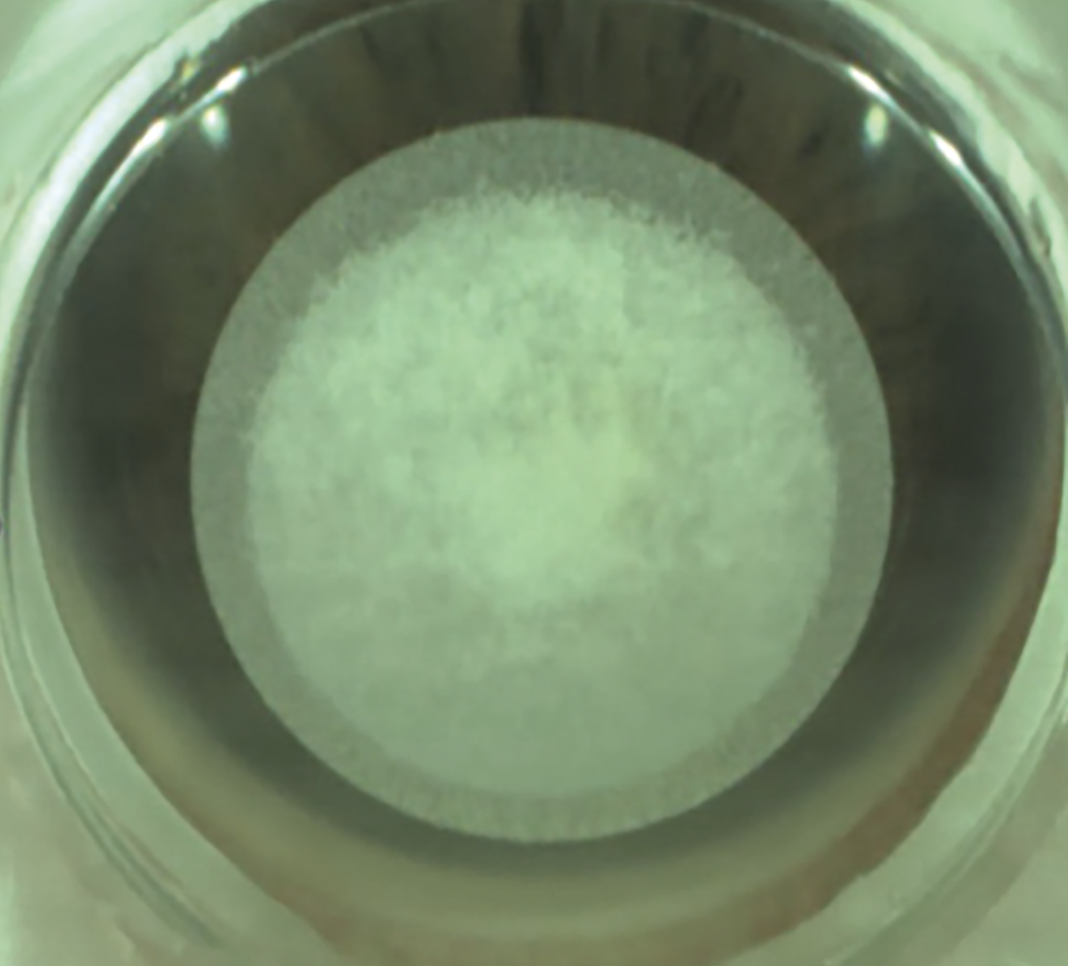
“The Elita system,” Dr. Manche adds, “also uses low energy level settings (less than 50 nanojoules) which produces a very smooth lenticule. In addition, the Elita utilizes overlapping spots, which allows for minimal dissection of the lenticule enabling nearly dissection-free removal of the lenticule.”
Patients who undergo lenticule creation have a similar experience as those who receive LASIK flap creation performed using the Intralase iFS 150 femtosecond laser, explains Dr. Manche while noting that the Elita femtosecond laser uses scleral-based suction similar to the Intralase.
“The patient will feel some pressure in their eye during lenticule creation. Once the SILK procedure is completed on the Elita femtosecond laser, the patient is repositioned under the microscope,” he says. “The superior incision is opened, and lamellar dissection is performed on the anterior and posterior lenticule planes. In most cases, there’s minimal dissection needed and the lenticule comes out very easily.”
During the procedure, patients are very comfortable and don’t experience any postoperative pain the first 12 to 24 hours. Dr. Manche reports that patients typically see quite well on postoperative day one and can return to normal activities the following day.
Dr. Manche and colleagues hope that the SILK surgical procedure will lead to even better outcomes than what is observed with the currently FDA-approved SMILE surgical procedure. “Having the ability to adjust for pupil centration as well as cyclo-rotation should, in theory, improve refractive outcomes,” he notes. “In addition, the ease of lenticule removal with minimal dissection should, in theory, lead to faster recovery of vision at postoperative day one.”
Laser-Induced Refractive Index Change (LIRIC)
This procedure, which is currently in development, is described as a minimally-invasive approach to refractive surgery, using a femtosecond laser by Clerio Vision. LIRIC is an incision-free procedure for correcting corneal refractive error, according to Scott MacRae, MD, at the University of Rochester. “Unlike refractive surgery, there’s no ablation, epithelial debridement or flap cutting,” he explains. “Also, because LIRIC doesn’t require epithelial debridement or the instillation of any dopant drugs, such as riboflavin (as opposed to corneal cross-linking). This strategy could help minimize patient postoperative recovery times both with corneal and IOL treatments,” suggests Dr. MacRae, who also notes that LIRIC would give clinicians a minimally invasive option to correct refractive error and do sequential treatments if a patient’s refraction changes.
“Currently in ophthalmology, femtosecond lasers are primarily used to ablate or cut material, such as flap cutting in laser refractive surgery or crystalline lens dissection in cataract surgery,” he says. “In these cases, every laser pulse acts as a miniature explosion, creating water cavitation bubbles, allowing the dissection of tissue.”
He explains that LIRIC spares the corneal nerves, causes much less damage to keratocytes and leaves the topography of the cornea intact, and notes, “Instead of ablation, LIRIC uses much lower pulse energies to modify the tissue’s refractive index. The change in refractive index is highly localized, like using a fine-point pen.”
Most patients are candidates for LIRIC, according to Dr. MacRae. “Since the LIRIC procedure doesn’t remove any tissue, patients with thin corneas, who otherwise would be poor candidates for laser refractive surgery, would stand to gain the most from this procedure.”
Clerio is also developing LIRIC treatment directly to implanted IOLs in pseudophakic eyes. “About a third of post-cataract patients have some residual refractive error due to healing of the capsular bag and post-implantation IOL movement,” Dr. MacRae explains. “LIRIC can correct those residual aberrations for an ‘optical touch-up.’”
In their clinical and pre-clinical work to date, Dr. MacRae and colleagues haven’t observed any induced inflammation or wound healing response. Post-treatment corneas were clear, had no scatter and no signs of inflammation. As noted earlier, LIRIC resulted in significantly less keratocyte cell death compared to fs-laser flap cutting and left the corneal nerves intact, according to histology studies.2,3
Treatment time for the first-in-human presbyopia treatment was approximately one minute. Dr. MacRae envisions that this will shorten to well below a minute as the technology matures.
Proponents say this procedure could be a game-changer for refractive surgery and help mitigate patient fears surrounding surgery. “We expect corneal LIRIC to address that limitation of laser refractive surgery,” says Dr. MacRae. “In addition to widening the eligibility criteria to patients with thin corneas, because LIRIC doesn’t remove tissue or change corneal curvature, we expect to see less impact of epithelial remodeling, and fewer instances of dry eye.”
Dr. MacRae and colleagues are currently developing a near-infrared version of corneal LIRIC and are in the midst of pre-clinical testing in collaboration with an ophthalmic company. While this approach holds significant promise, Dr. MacRae acknowledges that there are formidable technical challenges when it comes to developing a femtosecond laser system for corneal LIRIC in the near infrared.
“To allow for LIRIC, rather than flap-cutting, the laser system has more stringent specifications around pulsewidth,” he explains. “Developing clinical devices with ultrashort laser pulses is critical for LIRIC and requires careful engineering.”
Dr. MacRae and his team are excited for the future of LIRIC and their ongoing efforts to develop techniques for both refractive surgery and post-IOL implantation touch-ups. “Outside of these areas, we’re also working on advanced contact lens products where the LIRIC system will be used as a tool for embedding diffractive optical patterns into soft contact lenses,” he says. “We have programs aiming to develop such lenses for better correcting presbyopia and a therapeutic lens for the more effective treatment of myopia progression.”
Corneal Lenticule Extraction for Advanced Refractive Correction (CLEAR)
This femtosecond laser surgery is used to correct myopia with or without astigmatism. By using a low- energy laser, CLEAR maximizes precision with minimal tissue and side effects as well as less inflammatory response. The procedure, which is performed with the Femto LDV Z8 laser (Ziemer Ophthalmic Systems), received the CE Mark in April 2020 for the correction of -0.5 to -10 D of sphere and up to -5 D of cylinder.4
The CLEAR procedure is an optional software upgrade to the Z8 multipurpose laser, explains Professor Jod S. Mehta, BSc (Hons.), MBBS, PhD, FRCOphth, FRCS (Ed), FAMS, FARVO, Distinguished Professor in Clinical Innovation in Ophthalmology, SNEC. The laser platform can also be used for cataract surgery, corneal transplantation, pterygium surgery, tunnel and pocket creation for inlays and LASIK flap creation.”
The Z8 laser is based on a low-energy (<100 nJ) high-frequency (up to 20 MHz) concept, according to Dr. Mehta and colleagues, “where the miniaturized scanning optic, integrated into the handpiece, and its high numerical aperture create highly focused laser pulses.”4
Using a femtosecond laser, CLEAR creates a refractive lenticule that’s then removed through either one or two small incisions in the cornea, depending on surgeon experience, notes Dr. Mehta. He refers to it as a “second-generation procedure,” that differs from the established lenticule procedure.
These differences, according to Dr. Mehta, include lower energy, a smaller machine which makes it easy to handle, lenticule creation/centration and cyclotorsion control that’s customizable from the laser screen, and decreased patient discomfort due to the procedure’s speed.
“Following topical anesthesia, the patient is asked to fixate on a red target during applanation,” he explains. “After this is performed, there’s little else for the patient to do apart from relax. The lenticule procedure is fully customizable with the suction on, hence there’s no need for the patient to be actively involved in the refractive procedure.”
Dr. Mehta says the CLEAR procedure may be a better option for patients prone to dry eye or those who aren’t candidates for LASIK. It also provides a faster visual recovery with most patients returning to their normal routines just a few days after the procedure.
As with any new procedure, especially a refractive one, Dr. Mehta acknowledges that you want to approach it with some caution. “There will always be some optimization of the laser that’s required,” he says. “Our experience has been positive so far. We’ve had some excellent results and now we’re working to improve on this promising start. With so many different procedures, it is an exciting time to be a refractive surgeon.”
SmartSight
This minimally invasive lenticule extraction procedure, powered by the ATOS femtosecond laser (Schwind eye-tech-solutions), can be used to treat myopia as well as astigmatism. While not FDA approved, this laser platform received CE approval in 2020.
The SmartSight procedure creates a predefined lenticule in the intrastromal tissue of the cornea and makes small peripheral incisions in the top corneal layer for lenticular access. This approach uses no corneal flap and there’s no laser ablation.5
Additionally, SmartSight includes an eye tracking system, with pupil recognition and cyclotorsion compensation. “It uses very low energy and has asymmetric laser patterns that make it very easy to dissect, and it also has the least corneal swelling postop,” notes Kishore Raj Pradhan, MD, medical director, Matrika Eye Care Center, Kathmandu, Nepal.
Research has demonstrated that myopic astigmatism correction with SmartSight resulted in good efficacy, safety, predictability and visual outcomes in the first three months of follow-up. The study authors reported that spherical equivalent correction within ±0.5 D was achieved in 62 eyes (60 percent), and cylindrical correction in 90 eyes (87 percent).6 Additional research by Dr. Pradhan and colleagues found that patients treated with SmartSight lenticule extraction had positive outcomes at 12-months of follow-up.7
Dr. Pradhan has experienced the evolution of SmartSight firsthand, performing more than 1,600 SmartSight procedures already. He notes a number of strengths, including less dryness postoperatively, a strong cornea postop and very good results. “The ATOS is still evolving and the surgeries are getting faster and easier every day,” he says.
Ongoing Advances
Another interesting development is the initiation of a trial evaluating the safety and efficacy of the Technolas Teneo excimer laser for LASIK vision correction surgery for hyperopia with astigmatism (Bausch + Lomb).
The first patient was recently enrolled in this multicenter, prospective, single arm, open-label, non-randomized clinical study. It’ll include up to 334 operative eyes undergoing LASIK surgery for correction of hyperopia and hyperopic astigmatism.
“The demand for LASIK vision correction has risen significantly among our patients over the past few years, and refractive surgeons want options that meet the needs of their patients,” said Y. Ralph Chu, MD, study investigator, and founder and medical director of Chu Vision Institute and Chu Surgery Center, Bloomington, Minnesota, in a prepared company statement discussing the trial. “This study represents an exciting opportunity to evaluate new technology that has the potential to help more hyperopic patients.”
Refractive surgery continues to evolve with the addition of new and refined technologies, concludes Dr. Manche. “All of the current keratorefractive surgical procedures including LASIK, SMILE and PRK offer outstanding outcomes with excellent safety. We anticipate that new surgical procedures will continue to advance the field and improve outcomes and safety.”
Dr. Manche is a consultant for Avedro, Carl Zeiss Meditec and Johnson & Johnson Vision. Dr. MacRae has an equity interest in Clerio Vision. Dr. Mehta gives lectures for Zeiss, Ziemer, Leica, Santen and Moria. Dr. Chu is a consultant for Bausch + Lomb. Dr. Pradhan has no financial disclosures.
1. Johnson & Johnson Vision Receives CE Mark Approval for New Corneal Refractive Technology, the ELITA Femtosecond Laser System. https://www.jjvision.com/press-release/johnson-johnson-vision-receives-ce-mark-approval-new-corneal-refractive-technology. Accessed Mar 17, 2023.
2. Wozniak KT, Elkins N, Brooks DR, et al. Contrasting cellular damage after Blue-IRIS and Femto-LASIK in cat cornea. Exp Eye Res 2017;165:20-8.
3. Wozniak KT, Butler SC, He X, et al. Temporal evolution of the biological response to laser-induced refractive index change (LIRIC) in rabbit corneas. Exp Eye Res 2021;207:108579.
4. Fuest M, Mehta JS. Advances in refractive corneal lenticule extraction. Taiwan J Ophthalmol 2021;11:2:113-21.
5. Schwind eye tech solutions. SmartSight: The minimally invasive lenticule extraction. https://www.eye-tech-solutions.com/smartsight. Accessed Mar 17, 2023.
6. Pradhan KR, Arba-Mosquera S. Three-month outcomes of myopic astigmatism correction with small incision guided human cornea treatment. J Refract Surg 2021;37:5:304-11.
7. Pradhan KR, Arba Mosquera S. Twelve-month outcomes of a new refractive lenticular extraction procedure. J Optom 2023;16:1:30-41.