 “All the companies have gone through evolutions,” says Los Angeles surgeon Uday Devgan, MD. “As a result, we have lenses that are better performing and easier to use. If you tried some of the presbyopia-correcting lenses a few years ago and you were less than thrilled, if you had some unsatisfied patients, or if you had some difficulty inserting the products, don’t be discouraged because these newer generation products are certainly a lot better, and I expect the cycle to continue. Every generation just gets better and better.”
“All the companies have gone through evolutions,” says Los Angeles surgeon Uday Devgan, MD. “As a result, we have lenses that are better performing and easier to use. If you tried some of the presbyopia-correcting lenses a few years ago and you were less than thrilled, if you had some unsatisfied patients, or if you had some difficulty inserting the products, don’t be discouraged because these newer generation products are certainly a lot better, and I expect the cycle to continue. Every generation just gets better and better.”
Kevin Miller, MD, who is also based in Los Angeles, agrees. “The ReSTOR +4.0 was the very first FDA-approved diffractive lens,” he says. “It had a spherical optic, and there were complaints of waxy and poor-quality vision by some patients. This is when the majority of surgeons began implanting premium IOLs. The lenses have subsequently become much, much better, but a lot of people who got burned early on decided they were just going to forget it and not trouble themselves. However, the latest-generation multifocal lenses are quite good.”
ReSTOR +3.0
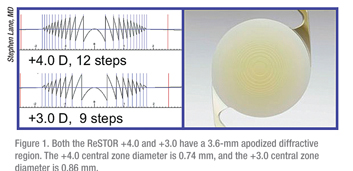
Dr. Devgan believes the Alcon AcrySof ReSTOR +4.0 provided near vision that was a little too near and lacked intermediate performance for computer users. “The ReSTOR +3.0 has addressed both of these issues by decreasing the power of the reading add and adjusting the diffractive ring pattern, which is on the anterior surface of the IOL,” he says.
Additionally, the newest generation of ReSTOR is aspheric. “The first iteration of the AcrySof ReSTOR came out as a spherical lens, as opposed to an aspheric lens, and was originally introduced as a clear lens as opposed to a yellow chromophore lens,” says Stephen Lane, MD, a surgeon from Stillwater, Minn. “With the +3.0 version, the near point is a little farther away, and patients get a better range of vision. Virtually all of the problems related to quality of vision have been improved upon by the asphericity, and the yellow chromophore may also play a role.”
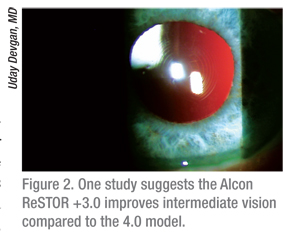 |
A study conducted in the Netherlands compared visual performance after implantation of a +3.0 AcrySof ReSTOR SN6AD1 IOL or a +4.0 AcrySof ReSTOR SN6AD3 IOL and found that implantation of the +3.0 lens resulted in better intermediate vision than with the +4.0 model, without compromising distance and near visual acuity.2 In this prospective study, the +3.0 IOL was implanted in 68 eyes, and the +4.0 IOL was implanted in 46 eyes. The uncorrected intermediate visual acuity was significantly better in the +3.0 group than in the +4.0 group at 40, 50, 60 and 70 cm. In addition, the uncorrected distance visual acuity was better in the +3.0 group, and the uncorrected near visual acuity at the preferred working distance was similar in both groups. Eyes with the +3.0 IOL also had lower mean levels of higher-order and spherical aberrations.
Tecnis
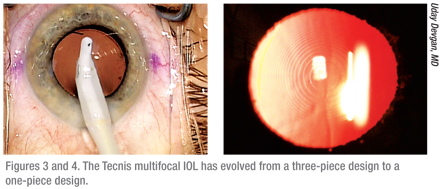
Like the AcrySof ReSTOR, the Tecnis multifocal (Abbott Medical Optics) is aspheric and has a diffractive lens design. It has evolved from a three-piece design to a one-piece design, which is much easier for surgeons because it is more resilient and forgiving, according to Dr. Devgan.
Jay Pepose, MD, a surgeon from St. Louis, adds that it has a close near point, but the near point is not as close as that of the ReSTOR +4.0. “That slight difference in the near focal point is a result of the diffractive steps being located on the posterior surface of the Tecnis multifocal versus the anterior surface of the ReSTOR +4.0,” he says.
 The Tecnis multifocal ZM900 has recently been shown in a multicenter, evaluator-masked, bilateral study to provide enhanced near visual acuity, reading acuity speed, depth of focus, and spectacle independence compared with the CeeOn 911A monofocal IOL.3 The study included 244 eyes of 125 patients who received the Tecnis IOL and 245 eyes of 123 patients who received the CeeOn IOL. Mean distance visual acuities were equivalent between the two groups; however, mean binocular and monocular uncorrected and distance-corrected near visual acuities were significantly better for the Tecnis multifocal. More Tecnis patients achieved binocular combined visual acuities of 20/25 distance and 20/32 near. The Tecnis group had excellent depth of focus, maintaining a mean of 20/40 or better for far, intermediate and near distances. Mean contrast sensitivity scores were lower for the Tecnis group, but the differences were not considered clinically significant. Halos and night glare were more common in the Tecnis group. Reading acuity (20/20 vs. 20/47) and speed (148 vs. 117 words/minute) were significantly better for the Tecnis IOL eyes, as were the proportions of the Tecnis eyes that achieved spectacle independence (84.8 percent vs. 5.2 percent) and that functioned comfortably at near without glasses (96.4 percent vs. 30.4 percent).
The Tecnis multifocal ZM900 has recently been shown in a multicenter, evaluator-masked, bilateral study to provide enhanced near visual acuity, reading acuity speed, depth of focus, and spectacle independence compared with the CeeOn 911A monofocal IOL.3 The study included 244 eyes of 125 patients who received the Tecnis IOL and 245 eyes of 123 patients who received the CeeOn IOL. Mean distance visual acuities were equivalent between the two groups; however, mean binocular and monocular uncorrected and distance-corrected near visual acuities were significantly better for the Tecnis multifocal. More Tecnis patients achieved binocular combined visual acuities of 20/25 distance and 20/32 near. The Tecnis group had excellent depth of focus, maintaining a mean of 20/40 or better for far, intermediate and near distances. Mean contrast sensitivity scores were lower for the Tecnis group, but the differences were not considered clinically significant. Halos and night glare were more common in the Tecnis group. Reading acuity (20/20 vs. 20/47) and speed (148 vs. 117 words/minute) were significantly better for the Tecnis IOL eyes, as were the proportions of the Tecnis eyes that achieved spectacle independence (84.8 percent vs. 5.2 percent) and that functioned comfortably at near without glasses (96.4 percent vs. 30.4 percent).
Crystalens
Bausch + Lomb’s Crystalens is a presbyopia-correcting IOL, but it is an accommodating lens rather than a multifocal lens. “The original Crystalens, the AT-45, was a small 4.5-mm optic, which was a little more finicky and difficult to put in than newer versions,” Dr. Devgan explains. “B+L then went to the Crystalens model 5.0, and that lens was relatively easy to use and delivered excellent distance and intermediate vision but didn’t give quite as much near acuity. Then came the Crystalens HD, which gave better reading performance and near vision, but, as a result of its design, required a much more exacting postop target. That lens doesn’t tolerate any residual refractive error above 0.50 D for both sphere and cylinder, so if the surgeon left a little bit of astigmatism, the lens wouldn’t perform as well. Now, there is the Crystalens AO, which has an aspheric optic, a wide range of vision, and a tendency to be forgiving of small residual refractions.”
According to Dr. Pepose, the Crystalens HD has a bispheric modification. “The center of the lens implant had a little bump that they call a bispheric modification,” he says. “That increased the depth of field but it also made it a little bit more important to hit the target exactly. It was a little less forgiving if you didn’t get exactly to emmetropia. If you wound up a little bit on the plus side, the vision was better than if you wound up on the minus side. The AO has a symmetrical defocus curve, so it’s a lot more forgiving, and it has a higher image quality. It provides the best intermediate vision of the available presbyopia-correcting lenses.”
 Michael Colvard, MD, a surgeon from Encino, Calif., also finds the AO to be an improvement over the HD. “The HD had an element of multifocality to it, and I didn’t care for that lens,” he says. “The level of refractive predictability with the AO is extremely high. Our rate of touch-ups is down to around 5 percent with this lens. If you can prevent the secondary intervention, it is a great help to the patient, and it is also good for your practice.”
Michael Colvard, MD, a surgeon from Encino, Calif., also finds the AO to be an improvement over the HD. “The HD had an element of multifocality to it, and I didn’t care for that lens,” he says. “The level of refractive predictability with the AO is extremely high. Our rate of touch-ups is down to around 5 percent with this lens. If you can prevent the secondary intervention, it is a great help to the patient, and it is also good for your practice.”
While no studies have been published on the Crystalens AO, the Crystalens HD has been found to restore distance visual function and improve near vision.4 A recent study included 40 eyes of 20 patients who ranged in age from 50 to 87 years. Twenty-four eyes were implanted with the Acri.Smart 48S monofocal IOL, and 16 eyes were implanted with the Crysta-lens HD. In both groups, the uncorrected and corrected distance visual acuities improved significantly from preoperatively to postoperatively. The distance-corrected near visual acuity also improved significantly in both groups. The uncorrected near visual acuity was significantly better in the Crystalens group, and the defocus curves showed significantly better visual acuity in the Crystalens group at several levels of defocus.
Managing Expectations
Surgeons agree that the key to patient satisfaction with presbyopia-correcting IOLs is managing patient expectations. “All of the companies may be promising a bit too much,” Dr. Devgan feels. “One current ad says, ‘see near, far and everything in between.’ There is no way you can truly see near, far and everything in between unless you are 22 years old. There are simply no man-made body parts that are as good as young human healthy body parts.”
Dr. Miller agrees that many patients have unrealistic expectations. “If patients are being told they are going to have perfect vision for distance and near, then they are being set up for a fall,” he says. “I implant premium IOLs in approximately 20 percent to 25 percent of my patients, and I’m in a high-demand area. It doesn’t get any more cosmetic than in Los Angeles, and I’m only at 20 or 25 percent. When people say they are putting multifocals into 50 or 60 percent of their patients, I think they are overdoing it, and that’s where many of those unhappy patients are being generated.”
Dr. Devgan notes that it is difficult to tell exactly how each patient will heal. If a patient ends up with unexpected residual refractive error, it will change the result. “Tell patients you don’t know how they will heal,” he advises. “Tell them that you may need to use LASIK or something else to fine-tune their refraction afterwards. Help them to have realistic expectations. Tell them they will probably be able to read a menu in a well-lit restaurant without glasses, but they will not be able to read a Splenda packet in a candlelit room.”
Dr. Pepose notes that patients’ pupil size can have an effect on their outcomes. “Multifocal IOLs function differently based on pupil size. If you have a patient who has giant pupils all the time and they never get small, he or she may not get as good near vision as someone whose pupil has a dynamic range or vice versa,” says Dr. Pepose. “Some people’s eyes have different pupil sizes in the same lighting, so the lens might function differently in the same lighting between the two different eyes. Or the pupils may be different shapes. The pupil is really important to take into account. The Tecnis IOL splits light equally, so patients will see near or far the same almost regardless of pupil size. I also measure patients’ angle kappa because a high angle kappa could influence the performance of a multifocal lens. Many surgeons don’t measure these things preoperatively. By the time they see the patient, he or she is dilated. They may have no idea what the pupil size of the patient is in a bright room or a dark room.”
If you are just entering or returning to the premium IOL arena, surgeons recommend choosing your first patients carefully. Dr. Miller recommends implanting toric IOLs first because these patients expect to wear glasses postoperatively. “They are easy to make happy. Only after that would I go to a Crystalens or a multifocal lens,” he says.
Dr. Colvard looks for patients with significant cataracts with very good visual potential and low levels of corneal astigmatism that can be easily corrected with limbal relaxing incisions.
Dr. Devgan agrees. “Start with someone in whom any improvement would be welcomed,” he says. “Don’t start off with someone who is 20/25, because you may have a hard time making him or her happy. None of these lenses tolerate a lot of residual astigmatism. You have to be very good at limbal relaxing incisions or just choose patients who don’t have much astigmatism. For the first patients with a new lens, I want patients with an advanced cataract, an easygoing personality, and low levels of astigmatism. I tend to like patients who are hyperopic and not myopic, because, for them, any degree of freedom from glasses is a big improvement.”
1. Lane SS, Javitt JC, Nethery DA, Waycaster C. Improvements in patient-reported outcomes and visual acuity after bilateral implantation of multifocal intraocular lenses with +3.0 diopter addition: Multicenter clinical trial. J Cataract Refract Surg 2010;36:1887-1896.
2. De Vries NE, Webers CA, Montes-Mico R, Ferrer-Blasco T, Nuijts RM. Visual outcomes after cataract surgery with implantation of a +3.00 D or + 4.00 D aspheric diffractive multifocal intraocular lens: Comparative study. J Cataract Refract Surg 2010;36:1316-1322.
3. Packer M, Chu YR, Waltz KL, et al. Evaluation of the aspheric Tecnis multifocal intraocular lens: One-year results from the first cohort of the Food and Drug Administration clinical trial. Am J Ophthalmol 2010;149:577-584.
4. Alio JL, Pinero DP, Plaza-Puche AB. Visual outcomes and optical performance with a monofocal intraocular lens and a new-generation single-optic accommodating intraocular lens. J Cataract Refract Surg 2010;36:1656-1664.



