Dry eye is the most common non-keratome-related complication of refractive surgery, and it can have devastating consequences in certain patients. Fortunately, it's also one of the most preventable complications if you take an intelligent approach to preop evaluation and management. However, there are still cases with surface abnormalities that contraindicate refractive surgery. In this article, I'll explain how I classify dry-eye patients as potential candidates and how I manage them, and take a look at the instances in which I just say no to certain refractive candidates.
Surface Testing
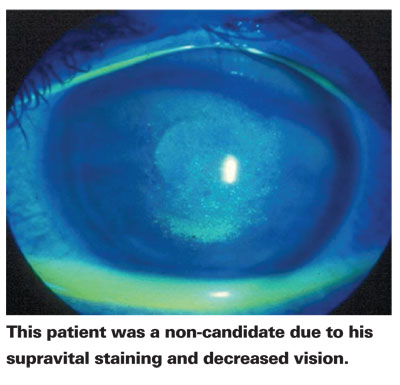
Just as the colors of a traffic light tell you how to proceed through an intersection, when you see staining in the conjunctiva or cornea, you should also be prepared to slow down or stop your progression toward refractive surgery. This is because such staining tells you there is tissue damage caused by dry eye that's going to either impact postop dry eye or visual acuity.
To evaluate the ocular surface, I use lissamine green on all candidates to look for conjunctival staining. Rose bengal is equally good for this. And I use corneal fluorescein staining to check for involvement of the visual axis.
When I see a patient for a preop evaluation, if there's no supravital staining at all, regardless of the symptoms, I consider him a very good candidate for refractive surgery, as long as I also perform the appropriate preop measures.
If a patient has conjunctival staining but there's no corneal staining, he's what I would call a moderate candidate. This type of patient has a risk for worse dry eye after his surgery. The moderate candidate should have his dry eye pretreated to improve the tear film, and should be warned about the possibility of worse dry eye postoperatively.
Finally, if a patient has supravital conjunctival staining and central corneal staining with fluorescein, he's a non-candidate. However, preop ocular surface therapy can turn these patients around. I'll never treat a patient with LASIK with active central corneal staining without some sort of preop treatment regimen.
As far as symptoms go, most of these patients will commonly complain of dryness and irritation. However, these symptoms don't really worry me as long as the signs are good. The one symptom that I pay particularly close attention to, though, is fluctuating acuity. If someone tells me he has changes in vision during the day, he will almost always have corneal staining and involvement of the visual axis.
Corneal topography tells you how significant the dry eye is. If you have an absolute breakup of the corneal surface, you know the patient has significant dry eye and isn't a good candidate unless his surface can be rehabilitated. The same goes for the wavefront. I look for the Hartmann-Shack image's small light reflections. If a patient comes in and has a poor Hartmann-Shack image, I know that not only is he at risk for dry eye postop, but his LASIK result may not be as good because of inaccurate Hartmann-Shack images.
Co-morbidities of Note
In addition to conjunctival and corneal stains, I also analyze co-morbidities, since there are a lot of diseases associated with neurotrophic corneas, which can cause or worsen dry eye and lead to poor results.
A common disease associated with neurotrophic corneas is diabetes. I check the corneal sensation of all diabetics who present for a LASIK consultation. If their sensation is normal, I treat them as routine patients. If they have corneal anesthesia, however, I consider them non-candidates, because these patients will most likely develop significant dry eye postop.
Some diseases and conditions that I also check for are:
• a history of Herpes, a very strong relative contraindication;
• structural lid disease;
• V and VII nerve palsies;
• a history of blepharoplasty that may have led to poor lid closure and a resulting exposure keratitis; or
• a history of rheumatoid disease, especially arthritis, Wegener's granulomatosis and thyroid disease.
For patients with rheumatoid disease, in addition to Schirmer's testing and corneal staining, I have an informed consent form that warns them they may have a worsened prognosis for dry eye with or without LASIK.
Salvaging the Surface
As I mentioned, many of these dry-eye patients can be treated preoperatively and have good LASIK outcomes.
First, you need to treat any existing lid disease with the traditional methods of patient-administered hot compresses and lid massage. I have also been using a new product, SteriLid (Advanced Vision Research) that sterilizes the lid margin in patients with significant blepharitis. If patients have a history of rosacea or haven't responded to traditional therapy, I will occasionally add oral doxycycline.
The most important therapy, which can be effective even for poor candidates, is a mild corticosteroid used preop alongside cyclosporine A (Restasis, Allergan). I usually choose Lotemax (loteprednol, Bausch & Lomb) for this, b.i.d. for two weeks; however fluorometholone (FML, Allergan) or rimexolone (Vexol, Alcon) are reasonable choices. I then start Restasis b.i.d. At the end of the first month of the treatment I'll taper or stop the steroid, but I'll continue using the Restasis pre- and postop for as long as necessary. I've found this combination really expedites the improvement in tear-film function and reduces the symptoms of inflammation and irritation associated with Restasis. Once I've used the Restasis for two weeks, I'll often use punctal occlusion as an ancillary therapy, and I'm a believer in nutritional supplements; I use TheraTears nutrition.
I've had good results with many types of patients using this regimen, including those with corneal and conjunctival staining. The only patients I wouldn't treat with refractive surgery would be those with active rheumatoid disease that wasn't stable, or someone with staining and fluctuating vision that doesn't respond to therapy.
Intraoperative Insights
I also take intraoperative steps to avoid dry eye postop.
First, if I think dry eye might be an issue with a patient, I consider performing a surface procedure. Since the creation of the LASIK flap severs more of the corneal nerves that serve the central cornea than PRK, the latter may preserve more corneal sensation and decrease the risk of dry eye.
If I choose to perform LASIK, I'll try to use as wide a hinge as possible, since we've found that the loss of corneal sensation and presence of dry-eye symptoms were greater in eyes with narrow hinges.1 I'll also place the hinge nasally, as some studies have shown a statistically significant increase in dry eye with a superior-hinged flap.2,3 (However, another study didn't find a difference.4) I also try to make the flap small, since a study we presented at the 2004 meeting of the American Society of Cataract and Refractive Surgery found that smaller flaps were associated with less dry eye.
I do my best to avoid epithelial defects with proper lubrication. I use Celluvisc postoperatively and minimize my use of non-steroidal anti-inflammatory drops and antibiotics to reduce the risk of epithelial sloughing. Probably most important, I start my anesthetics when the patient enters the operating suite in order to minimize epithelial toxicity.
Surface problems can be relative and sometimes absolute contraindications for refractive surgery. However, with intelligent management, you can decrease the incidence and severity of refractive-surgery related dry eye.
Dr. Donnenfeld is in private practice at Ophthalmic Consultants of Long Island, and frequently lectures on cornea, external disease and refractive surgery. In terms of products in this article, he is a consultant to Allergan, Alcon, AMO and Bausch & Lomb.
1. Donnenfeld ED, Ehrenhaus M, Solomon R, et al. Effect of hinge width on corneal sensation and dry eye after laser in situ keratomileusis. J Cataract Refract Surg 2004;30:790-797.
2. Donnenfeld ED, Solomon K, Perry HD, Doshi SJ. The effect of hinge position on corneal sensation and dry eye following LASIK. Ophthalmology 2003;110:3:1023-1029.
3. DePaiva CS, Chen Z, Koch DD, et al. The incidence and risk factors for developing dry eye after myopic LASIK. Am J Ophthalmol 2006;141:3:438-445.
4. Vroman DT, Sandoval HP, Fernandez deCasto LE, et al. Effect of hinge location on corneal sensation and dry eye after laser in situ keratomileusis for myopia. J Cataract Refract Surg 2005;31:10:1881-1887.



