Your fastest growing patient population and the field of refractive surgery are reaching their prime at the same time. With more surgical options available than ever, more patients over the age of 50 are flooding ophthalmology practices, seeking new ways to correct presbyopia and other refractive errors.1 This growing trend has established a paradigm shift in preoperative planning. Increased screening takes precedence over promoting the benefits of LASIK, LASEK, Epi-LASIK, bladeless LASIK, wavefront LASIK, PRK, corneal inlays, implantable lenses and clear lens exchange.
“More than ever, we need to ask ourselves one simple question,” says George Waring IV, MD, FACS, founder and medical director of the Waring Vision Institute in Mount Pleasant, South Carolina. “What makes more sense–addressing the cornea or the lens?”
In this report, experts discuss the best answer to this question for a variety of patient types.
Ruling Patients In or Out
Surgeons accustomed to routine screening of younger patients need to evaluate more factors when individualizing refractive surgery recommendations for patients over 50.
David R. Hardten, MD, FACS, who is in private practice at Minnesota Eye Consultants in Minneapolis, looks carefully at health histories. For example, increased risks of early cataracts could raise second thoughts about refractive surgery for these patients. The following are such risk factors: history of smoking; diabetes; asthma; chronic bronchitis and cardiovascular disease. Inhaled and oral corticosteroids, oral chlorpromazine and oral multivitamin/mineral intake add to the risk.2
He also aggressively treats dry-eye disease before considering refractive surgery. “Ocular surface disease is more common in the older patient,” he notes. “It will get worse year by year, even after refractive surgery. Helping patients understand this is important.”
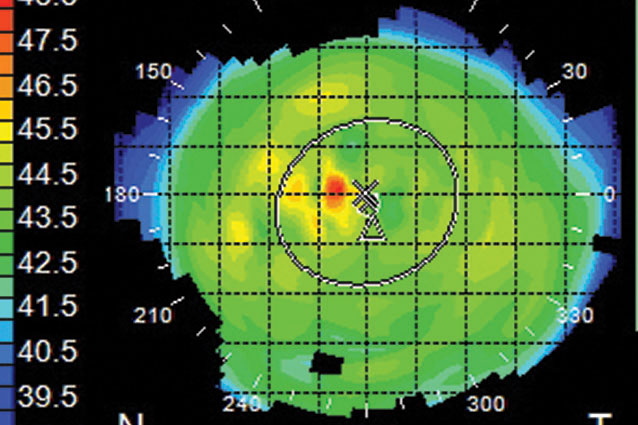
William D. Wiley, MD, medical director, Cleveland Eye Clinic and Clear Choice LASIK Center, holds off on LASIK and SMILE in the presence of contraindications commonly found in the over-50 population. “We won’t go through with it if a patient has keratoconus, age-related macular degeneration, corneal scars, early signs of cataract, acute eye disease and other contraindications, such as unstable refractive values, astigmatism over 5 D, suspicious corneal topography and thinner-than-average corneas.”
Dr. Wiley emphasizes scrutinizing the lens, the progression of nuclear sclerosis, and the condition of the cornea. “The cornea might not be in the best shape for refractive surgery,” he notes. “They could have other conditions, such as Fuchs’ endothelial corneal dystrophy, Salzmann’s nodular degeneration, pterygium and corneal stromal fibrosis. We need to get any disease under control before proceeding with refractive surgery. Some may require chronic treatment. Others, such as nodules, can be treated [before surgery], allowing us to stabilize the underlying condition and proceed with refractive surgery.”
“Younger Elderly Patients”
An increasing number of baby boomers and Generation X patients want visual improvement that will help keep them gainfully employed, attractive and vital well into their senior years. By 2020, an estimated 1.4 billion people will turn presbyopic across the world.3 And the number of patients in need of ophthalmic care will increase markedly during the next 20 years, primarily because of the aging of the U.S. population.4
Alan Aker, MD, who runs the Aker-Kasten Eye Center with his wife, Ann Kasten, MD, in Boca
Raton, Florida, has always attracted seniors in need of cataract surgery. Now, he has noticed increased demand for “premium solutions with specific refractive outcomes” expressed by “our younger elderly patients.”
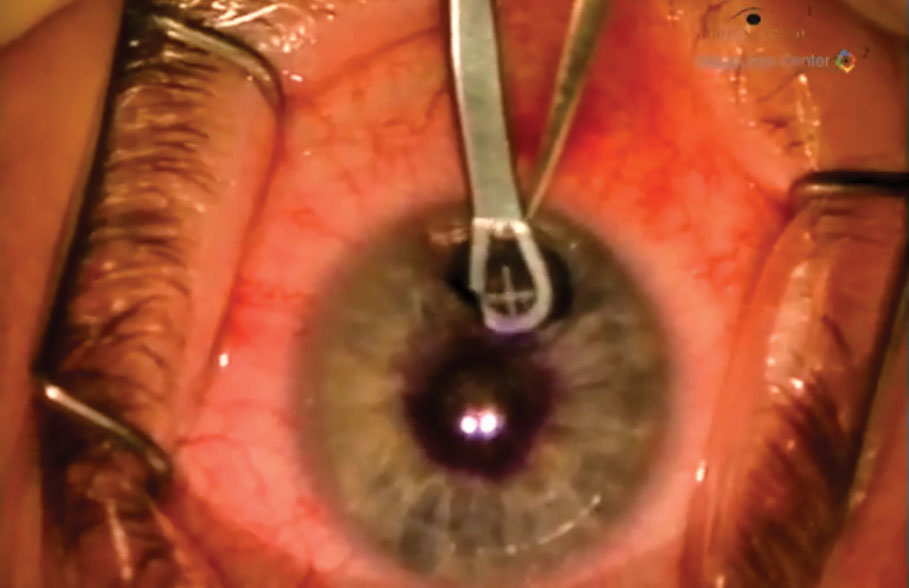
He and Dr. Kasten offer lens-based refractive procedures, and they say they’ve achieved success using the femtosecond laser. The addition of the femtosecond laser has helped the husband-and-wife surgical team increase their percentage of premium cataract-refractive cases from 30 percent to more than 75 percent in recent years. Dr. Aker explains that the femtosecond laser is attractive to the over-50 set because, among other things, its precise, bladeless cutting minimizes postoperative cornea issues and allows for correction of corneal astigmatism.
“For patients of this age who are interested in LASIK, we go into a lengthy discussion of the impact of LASIK and cornea-based refractive surgery on their future cataract surgery,” says Dr. Aker. “We explain that following a LASIK procedure, the calculations for the appropriate IOL power can be more challenging.”
Dr. Aker also informs over-50 patients seeking LASIK that, after some LASIK procedures, because of resulting spherical aberration, they may not be good candidates for some of the more advanced presbyopia-correcting implants. “We also explain to these younger patients presenting with minimal lens changes that youth and technology are on their side. We are currently involved in an FDA study evaluating the investigational SC9 IOL produced by the CORD Group LLC (Hammond, Louisiana). This is an extended-depth-of-focus IOL. We explain to these patients that this and other new advanced IOLs are currently being evaluated that might be able to provide even better vision than IOLS that are currently approved. Sometimes it’s best to wait. We feel it’s important to share this option with our patients.”
 |
|
|
The Refractive Gamble
Uncertainty can be a challenge when caring for these patients. Some surgeons feel like they need a diagnostic crystal ball of sorts to determine if a refractive procedure after age 50 might actually be too close to a patient’s eventual cataract surgery. “These days, I do see too many patients who have had refractive surgery only a year or two before they come to us in need of cataract surgery,” says Dr. Aker. “It would seem that lens-based refractive surgery would have been a better choice for them. First of all, lens-based surgery spares the patient the expense of a LASIK procedure. In addition, it leaves the patient with a pristine, untouched cornea, enabling us to provide them with the best possible outcome following cataract-refractive surgery with the appropriate premium IOL.”
Dr. Hardten evaluates every factor when deciding if a patient is too close to needing cataract surgery. “When we analyze the lens, including the amount of nuclear sclerosis, we try to figure out if the refractive error will stay the same long enough before cataract surgery is likely needed to make it worth doing corneal refractive surgery alone,” says Dr. Hardten.
Dr. Wiley assesses a patient’s presbyopia, nuclear sclerosis, possible onset of cataracts and changes in the crystalline lens that begin before and during presbyopia.
“If the patient has experienced a myopic shift, that can be a significant factor,” he adds. “Patient history over time is critical.”
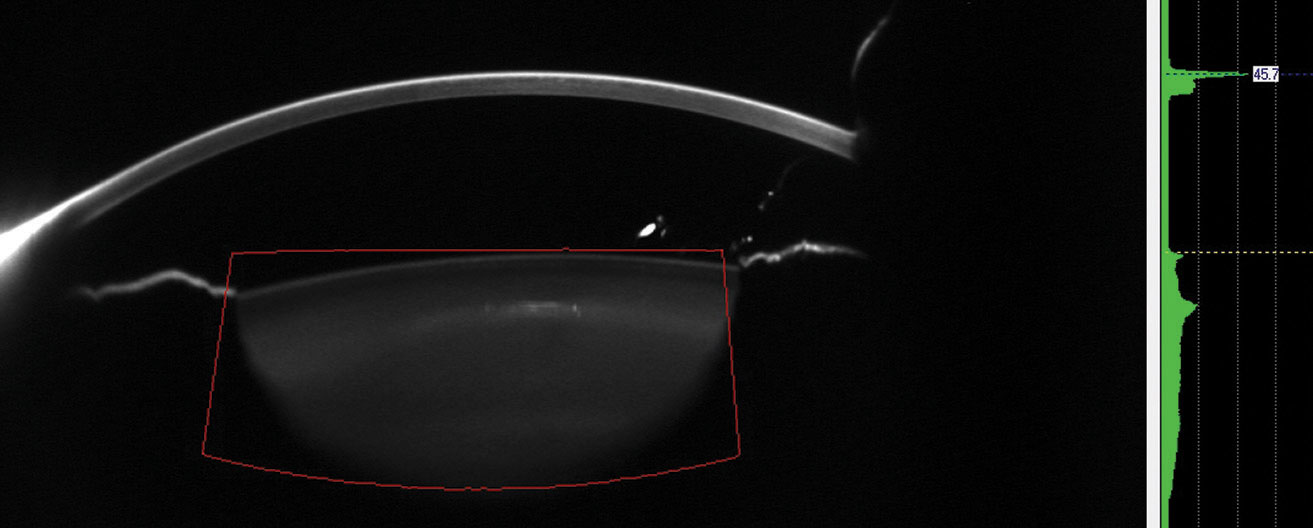
Dr. Wiley also uses the HD Analyzer (Visiometrics; Terrassa, Spain), which identifies subclinical cataracts by evaluating light scatter, helping determine if cornea-based or lens-based procedures are best. The instrument also measures tear-film breakup time. “We can determine if dry-eye therapy is best or, possibly, if a corneal approach should be avoided because of dry eye,” he points out.
Inside Versus Outside
Deciding whether to surgically correct a patient’s vision inside or outside of the eye is a judgment call, according to Dr. Wiley. “I base my decision on diagnostics and a big-picture analysis of the patient’s visual needs, corneal health and overall health. It’s never an automatic yes or no answer.”
 |
|
|
Deciding whether to address the cornea or crystalline lens involves a multifactorial decision-making process, guided by stages of dysfunctionality, according to Dr. Waring. He has evaluated the aging changes of the crystalline lens over the years. In an attempt to characterize these changes, Dan Durrie, MD, and Jason E. Stahl, MD, both of Durrie Vision in Overland Park, Kansas, and Dr. Waring suggested the term Dysfunctional Lens Syndrome, staged as follows:
Stage I: The lens becomes more rigid and less flexible, corresponding with presbyopia.
Stage II: Contrast sensitivity loss, increased higher-order aberrations and light scatter emerge.
Stage III: Lens opacities are now significant enough to interfere with daily activities. This stage corresponds with cataracts that qualify for an insurance-based procedure.
“We have found that lens replacement in patients with Stage II DLS improves vision in ways LASIK can’t,” he says. “We can reduce light scatter, improve retinal image quality and maintain binocularity. Furthermore, we are preventing the eventual degradation process into a cataract, when a second intervention could occur. Simply stated, we are preventing cataracts.” Dr. Waring still utilizes LASIK or implantable contact lenses “in the high axial myope with peripheral retinal pathology and other risk factors for retinal detachment in patients over 50 in Stage I DLS and, in select cases, in Stage II.”
One surgical option for presbyopia is the insertion of the donut-shaped Kamra (CorneaGen, Seattle) corneal inlay in the front of the cornea. The inlay, made of a dark polyvinylidene fluoride, is 3.8 mm in diameter with a 1.6-mm aperture. The Kamra relies on a pinhole effect to enhance near vision, allowing only central rays of light into the visual system to enhance depth of focus. It’s designed for monocular implantation at a minimum depth of 200 µm via a femto-created stromal pocket in the non-dominant eye. “If the patient’s lens is clear, ages 50 to 55 is the sweet spot for Kamra, providing enhanced range of focus for emmetropic presbyopic patients,” says Dr. Hardten. “If the patient has a refractive error of about -0.5 to -0.75, he or she can additionally gain some extra distance while improving near vision.”
Dr. Wiley combines Kamra inlays with LASIK for presbyopic patients. “We can target the dominant eye for plano and the non-dominant eye for -1 D,” he says. “We insert the inlay to extend the intermediate vision and conceivably remain in there indefinitely, offering a full range of focus of up to 2.5 D.”
Dr. Waring is also involved with a number of emerging presbyopia treatments beyond lens technology and excimer lasers, such as presbyopia eye drops. Furthermore, allogenic corneal inlays from corneal tissue are also being evaluated.
When Age Isn’t a Factor
Unlike some surgeons, Dr. Wiley says a patient’s older age doesn’t always prompt him to take a cautious approach to the corneal surface.
“We do LASIK and SMILE all the time,” he says. “On younger patients, we know they also will need cataract surgery at some point. A 20-year-old is the same as a 55-year-old, as I see it. Both have the same risks.”
Like many surgeons, Dr. Wiley is hardly an absolutist. “If I clearly see a patient is a year away from needing a cataract extraction and he or she wants refractive correction, I do a clear lens exchange. I am looking forward to increased usage of the Light Adjustable Lens (RxSight; Aliso Viejo, California), the only FDA-approved IOL that can be customized through a power adjustment after it’s implanted.”
Dr. Wiley has also found that corneal surface procedures on hyperopes may have less refractive stability over time. “Lens replacement may be best for them,” he conceded. “Hyperopia correction is trending toward lens replacement. LASIK and other corneal procedures become less viable because of the improvement that’s occurred in intraocular lens technology. We once considered LASIK for patients with a correction as high as +4 D or more. As lenses keep improving, we may consider lens replacement for over +1 D. Any presbyopic patient with moderate to high hyperopia would fall into this category.”
More SMILES for Older Patients
Dr. Wiley has started using the SMILE procedure more frequently for patients over 50.
 |
|
|
“The naturally occurring cross-linking of the corneal tissue makes the cornea strong, which helps these patients,” he notes. “SMILE is less invasive, doesn’t sever the corneal nerves, and minimizes dry eye, which is especially advantageous for patients over 50. Some of LASIK’s biomechanical characteristics are better tolerated by younger patients. With SMILE, removal of the lenticule-shaped disc of tissue is less traumatic for the older patient. I use SMILE on patients over 50 who are between -2 and -8 D and have 3 D of astigmatism or less and a manifest refraction spherical equivalent of -8.25 D.”
Clear Lens Exchange
Like Dr. Wiley, many surgeons are correcting refractive error inside the eye more because of advanced lens technology such as the Symfony and the AcrySof. Dr. Hardten favors the Tecnis multifocal IOLs for +2.75 D, +3.25 D or +4 D. “Depending on the patient’s desired second near point of focus, all of these lenses can be good options,” he says.
“For an older patient who is a good candidate for surgery, I consider lens replacement to address lack of accommodation, especially in the hyperopic patient,” Dr. Hardten says.
For lens replacement, Dr. Wiley also uses the Tecnis lenses and is impressed by Alcon’s new Activefocus optical design for the AcrySof IQ ReSTOR multifocal IOL.
“The low add power lenses don’t create the side effects of the higher add lenses of the past,” says Dr. Wiley, “Patients experience less glare, fewer halos, and not as much loss of contrast and visual quality. The more near vision you provide the patient, however, the higher the side effect profile will be.”
He addresses these issues by varying the lens powers. “The patient might say, ‘my near vision isn’t quite what I want,’” says Dr. Wiley. “Night driving might create adverse effects. So we will address that issue with less near power to reduce side effects. I will do one lens, let them drive for one to three weeks, then have them return and put in the correct lens for the other eye, with a power suited more for far or for near, depending on the patients’ visual experiences.”
Offer the Best
Whether you’re doing a procedure inside the eye or on the cornea, Dr. Wiley and other surgeons emphasize the need to be more flexible with the over-50 population, since it continues to grow. “We will have more patients and more options to offer them,” he notes. “It puts our diagnostic skills to the test and keeps us on our toes with all of the new technology. Overall, it creates a time of great excitement and opportunity for these patients and surgeons.” REVIEW
Dr. Aker is a speaker for Johnson & Johnson Vision and Bausch & Lomb. He also serves as Medical Monitor for the CORD Group. Dr. Wiley consults for CorneaGen, J&J Vision, Alcon and Zeiss, and receives research compensation from RxSight. Drs. Hardten and Waring report no relevant financial interests.
1.Paley GL, Chuck RS, Tsai LM. Corneal-based surgical presbyopic therapies and their application in pseudophakic patients. J Ophthalmol. 2016;2016:5263870. Epub 2016 Mar 9.
2. Prokofyeva E, Wegener A, Zrenner E. Cataract prevalence and prevention in Europe: a literature review. Acta Ophthalmol. 2013:91: 5:395-405. 2012 Jun 20.
3.Frick KD, Joy SM, Wilson DA, et al. The global burden of potential productivity loss from uncorrected presbyopia. Ophthalmology 2015;122:8:1706-10.
4. Congdon N, O’Colmain B, Klaver CC, et al. Causes and prevalence of visual impairment among adults in the United States. Arch Ophthalmol 2004;122:4:477-85.



