A number of companies are exploring regenerative medicine as a means for treating eye disease. “This is certainly in its infancy, but we are starting to see good results,” says David S. Boyer, MD, who is in practice in Los Angeles. “Delivery devices for stem cells have improved dramatically, which will pave the way for more stem cell utilization.”
Chicago’s Jennifer I. Lim, MD, adds that CRISPR-Cas technology will allow physicians to edit out the abnormal gene and insert the normal one. “I think we will have regenerative medicine to restore what has been depleted by atrophy or genetically programmed degeneration,” she says. “We will have ways to prevent the atrophy by giving a trophic factor to regenerate what’s still capable of growing, and then we’ll have ways to use stem cells to repopulate tissues and gene therapy to inject material to correct the problem that would cause degeneration again further down the road.”
Gene Therapy
Several companies are working on gene therapies for retinal diseases, trying to follow in the footsteps of Spark Therapeutics and its therapy Luxturna.
• Luxturna (Spark Therapeutics). Luxturna is the first FDA-approved gene therapy for a genetic disease. It is a one-time prescription gene therapy product that can be used for patients with an inherited retinal disease caused by mutations in both copies of the RPE65 gene and who have enough remaining cells in the retina.
It was approved by the FDA in 2017 for the treatment of patients with confirmed biallelic RPE65 mutation-associated retinal dystrophy that leads to vision loss. According to the FDA, the primary evidence of Luxturna was based on a Phase III study that included 31 participants and measured the change from baseline to one year in a patient’s ability to navigate an obstacle course at various light levels.1 Patients who received Luxturna demonstrated significant improvements in their ability to complete the course at low light levels compared with control patients.
• Intravitreal Gene Therapy (ADVM-022, Adverum). Adverum is investigating ADVM-022 as a one-time intravitreal injection for the treatment of wet AMD.
“Adverum has a modified AAV2 vector, which can be injected in the vitreous, and the results have been very encouraging,” says Pravin U. Dugel, MD, who is in practice in Sun City, Arizona. “Obviously, the big advantage is that it can be injected into the vitreous. It’s being studied for neovascular macular degeneration, and the results recently have shown that the number of injections is dramatically less in patients who otherwise would need repeated injections.”
 |
In the spring of 2020, Adverum presented interim data from cohorts 1 to 3 of the OPTIC Phase I trial of ADVM-022. They reported that all six patients in cohort 1 were rescue-injection-free after a year. Eight of 11 patients treated with a lower dose have also been rescue-injection free. The company says that ADVM-022 has been safe and well-tolerated, with no dose-limiting toxicities, and inflammation has been manageable with topical steroids; 69 percent of treatment-related adverse events are mild and 31 percent are moderate. In April, researchers dosed the first patient in Cohort 4 of the trial.2
In late May, the company initiated the INFINITY trial, evaluating the treatment in diabetic macular edema.
• Sepofarsen (ProQR). Sepofarsen, designated QR-110, is an RNA-based therapy, delivered via intravitreal injection, for congenital retinal diseases. The therapy is currently undergoing a Phase II/III trial called Illuminate, in which it’s being used to treat Leber’s congenital amaurosis type 10.
In the study, there was a high percentage of cataract development (eight out of 11 cases, 73 percent; six required surgery). There were two cases of mild cystoid macular edema that were treated successfully, and two cases of subclinical retinal thinning. However, pooled dose group data showed a significant improvement in the treatment group vs. baseline in best-corrected acuity, full-field stimulus threshold test and in the patients’ performance on a mobility course.3
Sepofarsen has an orphan drug designation, and received fast-track designation and rare pediatric disease designation from the FDA.
• RGX-314 (RegenxBio). RGX-314 is being developed by RegenxBio as a novel, one-time subretinal treatment that includes the NAV AAV8 vector containing a gene encoding for a monoclonal antibody fragment. It has the potential to treat conditions such as wet age-related macular degeneration and diabetic retinopathy. The expressed protein is designed to neutralize VEGF activity.
The company has an ongoing Phase I/IIa trial of RGX-314, which includes 42 patients with severe wet AMD that requires frequent anti-VEGF injections. These patients have been treated across five dose cohorts, with doses ranging from 3 x 109 GC/eye to 2.5 x 1011 GC/eye.
At two years, RegenxBio reports that RGX-314 continues to be well-tolerated across all cohorts, with no drug-related serious adverse events reported. It says that cohort 3 has shown a mean (14-letter) improvement in vision and stable retinal thicknesses. Half of the patients (three out of six) have remained anti-VEGF-injection-free, and 67 percent (four out of six) are injection-free from nine months to two years. In cohort 5, 73 percent of the patients (eight out of 11) have been injection-free for nine months.4
“The impressive thing about the RegenxBio data is that it’s not just that the number of injections are also dramatically less, but, for the first time, we’re able to see that there’s a dose-dependent increase in the amount of protein that’s produced, which we’ve never seen before,” Dr. Dugel says. “So, that is very impressive. Additionally, RegenxBio has a partnership with Clearside. Researchers believe that transfection of the vector can be as efficient given by suprachoroidal injection as subretinal delivery. This is very significant because the delivery may now be converted from a surgical procedure delivered in the subretinal space to a clinical procedure injected in the suprachoroidal space.”
• HMR59 (Hemera). CD59 is a protective protein that is normally found on the plasma membrane of cells, and it protects cells from a natural inflammatory cascade in the body called complement that acts as a part of the body’s nonspecific immune response. It is believed that macular degeneration is caused by an overactivity of complement. Studies have shown that patients with AMD have less CD59 present in the retina to protect their cells from damage caused by complement. Currently, Hemera’s gene therapy (HMR59) is under FDA-approved Phase I clinical testing for the treatment of both wet and dry AMD. When HMR59 is injected in the eye, it increases the ability of retina cells to make a soluble form of CD59 called sCD59. According to the company, the soluble CD59 circulates within the retina to block complement from further damaging the retina.
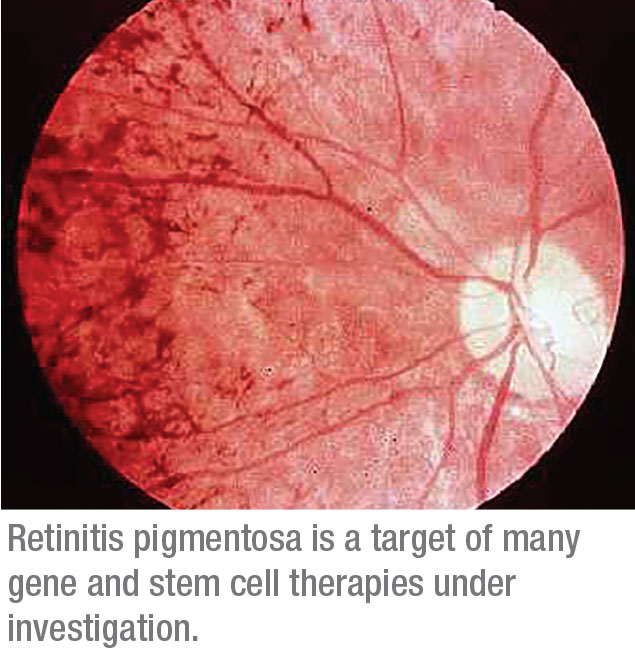
• OCU400 (Ocugen). Another gene therapy for retinitis pigmentosa, but at an earlier stage of development (Phase I), is Ocugen’s OCU400 (AAV-NR2E3). According to the company, OCU400 consists of a functional copy of a nuclear hormone receptor gene that’s delivered to certain cells in the retina using a viral vector.
Stem Cell Therapy
The idea behind stem cell therapy is to use implanted stem cells, which have the potential to develop into different types of useful cells, to generate healthy cells to replace those lost in retinal conditions. Here’s a look at what’s in the pipeline:
• jCyte. jCyte’s developmental stem cell therapy to treat retinitis pigmentosa is currently undergoing Phase IIb trials. Researchers at jCyte found that retinal progenitor cells could rescue and even replace diseased retinal cells, so they developed jCell, an allogeneic human retinal progenitor cell suspension. Patients will receive a single intravitreal injection, which can be done in the office. Early results from the Phase IIb trial have shown that the treatment is safe and doesn’t trigger an immune response.
“The advantage here is that it’s a clinic procedure as opposed to a surgical procedure, and it can be repeated,” Dr. Dugel says. “So, the fact that it’s not as invasive and is repeatable is a plus. Additionally, this treatment is agnostic of the retinitis pigmentosa subtype.” The company recently entered into a licensing agreement with Santen.
• hRPC Stem Cell Therapy (ReNeuron). ReNeuron is using proprietary human retinal progenitor cells, which, when transplanted onto the retina, have the potential to preserve existing photoreceptors and potentially reduce or halt further deterioration of vision.
The company has announced positive long-term data from its ongoing Phase I/IIa clinical trial of its hRPC stem cell therapy for the treatment of retinitis pigmentosa.
Patients in the study had a successful surgical procedure with sustained clinically relevant improvements in visual acuity compared with baseline, ReNeuron says. Additionally, the company says that long-term efficacy data from the study continue to show a meaningful clinical effect from the therapy out to 12 months.
The company has submitted a protocol amendment to the Phase IIa trial to treat an additional nine patients.
• ASP7317 (Astellas). Astellas is using cell therapies to address vision loss. ASP7317 is an investigational therapy derived from pluripotent human stem cells, and it is undergoing a clinical trial for the treatment of dry AMD. The company is sponsoring a two-stage, multicenter clinical trial to evaluate the optimal dose, safety, and efficacy of ASP7317.
• CPCB-RPE1 (Regenerative Patch Technologies). Regenerative Patch Technologies is developing cell-based implant technology for the treatment of retinal diseases. CPCB-RPE1 is a bioengineered implant consisting of stem cell-derived, mature, polarized retinal pigment epithelial cells in a single layer on an ultrathin synthetic parylene membrane. It is designed to replace the retinal pigment epithelium and Bruch’s membrane.
The membrane is implanted into the subretinal space during an outpatient surgical procedure. Preliminary results from a Phase I/IIa clinical trial demonstrated the safety of the implant.
Several assessments of visual function were also conducted. After CPCB-RPE1 implantation, patients demonstrated improved ability to focus or fixate on a target using the diseased area of the retina, and patients showed either stable or improved visual acuity, with one patient demonstrating a 17-letter improvement.
“This is a patch with an artificial membrane-type surface where the cells are very elegantly transplanted exactly where they’re missing,” Dr. Dugel explains.
CRISPR
Researchers are still in the early stages of assessing the genetic manipulation technique known as CRISPR (clustered regularly interspaced short palindromic repeats) for eye disease. It’s a new kind of genetic engineering that allows scientists to edit DNA. While traditional gene therapy uses viruses to insert new genes into cells in an attempt to treat diseases, CRISPR directly makes changes in DNA. The technique uses targeted molecular tools that work like scissors to cut out abnormal DNA and replace it with normal genetic material.5
Editas Medicine and Allergan are conducting a human trial of a CRISPR gene-editing therapy for inherited blindness. The Phase I/II trial will test a single subretinal injection of AGN-151587, also called EDIT-101, in 18 patients with Leber’s.6
Researchers plan to administer low, medium and high doses of the drug in children, and medium and high doses in teens. Similar to Luxturna, EDIT-101 is delivered to retinal cells via an adeno-associated virus.
Dr. Boyer says that CRISPR seems promising. “The most important thing about CRISPR is that you can take diseases that are hereditary and remove the gene,” he says, “so that the person who is affected can’t pass it along. However, we are messing with Mother Nature, so we don’t know what the long-term effects will be. Certainly, if you have a one-gene or two-gene disease, you may be able to modify enough to be able to overcome the defect. This is very exciting technology.” REVIEW
Dr. Boyer is a consultant to Allergan, jCyte, Adverum and RegenxBio. In terms of products mentioned in the article, Dr. Dugel is a consultant to Allergan, Santen and Spark Therapeutics. Dr. Lim has a financial interest in Santen.
1. FDA news. https://www.fda.gov/news-events/press-announcements/fda-approves-novel-gene-therapy-treat-patients-rare-form-inherited-vision-loss
2. Adverum news. http://investors.adverum.com/news-releases/news-release-details/adverum-biotechnologies-reports-positive-interim-data-cohorts-1
3. Russell S, Drack A, Cideciyan A, et al. Results of a phase 1b/2 trial of intravitreal (IVT) sepofarsen (QR-110) antisense oligonucleotide in Leber congenital amaurosis 10 (LCA10) due to p.Cys998X mutation in the CEP290 gene. Invest Ophthalmol Vis Sci 2020; 61:866.
4. RegenxBio news. https://regenxbio.gcs-web.com/news-releases/news-release-details/regenxbio-announces-additional-positive-long-term-and-interim
5. AAO news. https://www.aao.org/eye-health/news/crispr-gene-editing-dna-therapy-eyesight
6. AAO news. https://www.aao.org/headline/crispr-trial-inherited-blindness-underway




