When patients need both cataract and retina surgery, the procedures can be performed in combination or using a staged approach. The combined procedure, phacovitrectomy, provides several advantages for patients and retina specialists.
According to Christina Weng, MD, MBA, a retina specialist on faculty at Baylor College of Medicine in Houston, there are two categories of situations in which surgeons might consider a combined approach. The first situation is out of necessity. “For example, I can’t fix a retinal detachment if a dense cataract is obscuring the view,” she notes. “However, the more common situation is when there are two pathologies that can be addressed electively, such as an epiretinal membrane and a cataract. In these scenarios, it can be challenging to discern which symptoms are from the cataract and which are from the epiretinal membrane, but if both are likely contributing to the patient’s visual impairment, combined surgery is a terrific option.”
Dr. Weng believes that concurrent management of anterior and posterior segment pathology can often help patients achieve their best visual outcomes sooner. “If you stage the surgery, there’s always the risk that patients will have an outcome that falls short of their expectations,” she says. “While there are some risks with combined surgery, both modern-day cataract and retina surgery are very safe. I find that most patients are more than happy to have a two-in-one surgery to optimize their visual acuity, especially in a cataract surgery era where patients’ expectations are so high.”
According to Andrew Kao, MD, who is in practice in Bakersfield, California, one benefit of a combined procedure is potentially less cost to the health system overall. “In that situation, if a patient has a retinal problem and has already had intravitreal injections or some sort of vitrectomy in the past, it does increase the risk of a retained lens fragment or a posterior capsular rupture during cataract surgery,” he says. “For example, during my residency, I was performing a cataract procedure first, and then half the lens fell to the back of the eye. The patient was already going to have a vitrectomy that day, so then the retina specialist just stepped in a little earlier, removed the remaining lens and then did the retina procedure.”
Combined procedures also have some downsides, one of which is scheduling, says Tom Stone, MD, who is in practice in Louisville, Kentucky. “My biggest referring cataract group operates at a different surgery center than I do, so even if I wanted to do a combined case with one of their surgeons, I couldn’t,” he says. “I also think it’s inefficient to perform a combined procedure with another surgeon. They are either taking up your OR time by doing a cataract or you’re taking up their OR time by doing a retina case. I also find that a combined surgery is sometimes unnecessary. I almost always have the cataract surgeon do his surgery first, and in cases of borderline macular disease, patients will be happy with their vision after cataract surgery alone, and not need vitrectomy.”
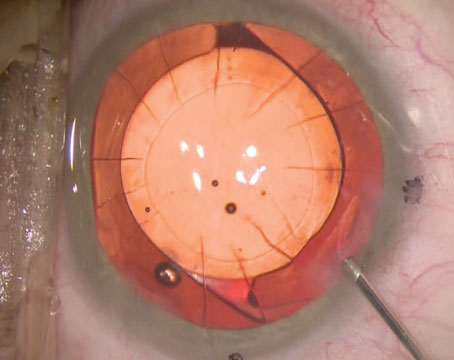
According to Uday Devgan, MD, who is in practice in Los Angeles, another critical factor is making sure the capsulorhexis overlaps the optic for a full 360 degrees. “If the capsulorhexis is too big, it may be best to wait at least a month to allow the capsular bag to “shrink-wrap” down to hold the lens firmly in place,” he explains.
Dr. Devgan also notes that retinal surgeons often use a gas bubble in the vitreous cavity to hold the retina in place. This gas can stay inside the vitreous cavity for weeks or longer. “If you just do a combined case in the same sitting, that gas bubble may end up pushing the IOL out of the capsular bag,” he warns.
When he performs combined cases, Dr. Devgan prefers to perform the cataract surgery first. “This gives the retina surgeon a much better view,” he says. “Remember that the retina surgeon has to look through either your cataract or your IOL in order to see the retina. Additionally, because the human lens is so thick, it can make access to the vitreous base or the edge of the retina very difficult because your instrument has to go across the eye and not hit that thick lens. Once you have a thin IOL in the eye, access to the vitreous base and the retinal periphery is easier.”
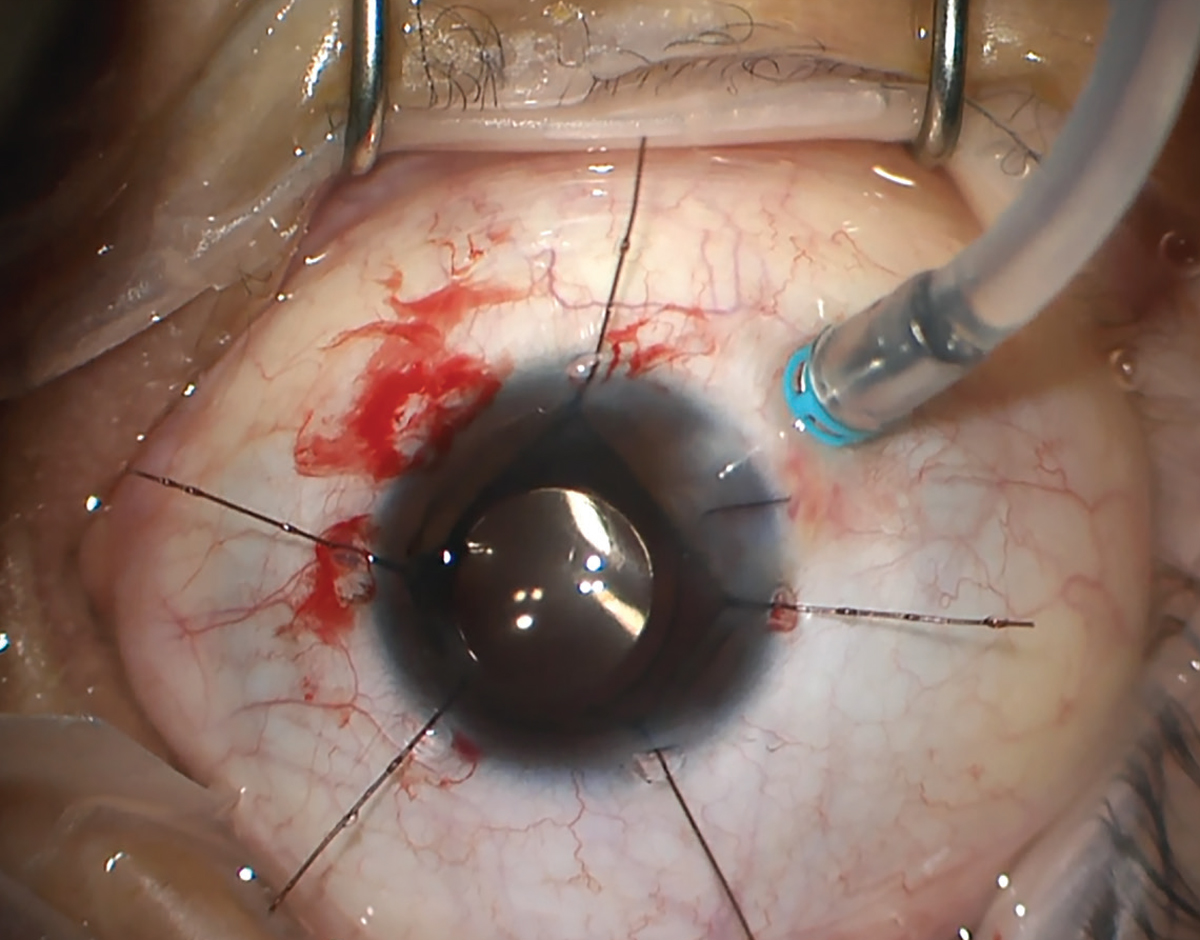 |
| Combined cataract and tractional retinal detachment surgery. Note the corneal suture, which was placed after the cataract extraction. Additionally, the inferotemporal trocar-cannula was pre-placed at the start of the surgery (infusion line was attached later). Both of these elements enhance globe stability, surgeons say. Photo: Christina Weng, MD. |
Staged Procedures
Dr. Kao, who works in a private practice setting, typically performs staged procedures. “Our local retina group refers cataract patients to us,” he says. “We do the cataract first, and then once the patient heals, he or she goes back to the retina surgeon. In an academic practice, it’s much easier to perform a combined procedure.”
He adds that a staged procedure is easier for the eye because there is less inflammation overall, and the eye has a chance to heal between the procedures. “One of the complications of cataract surgery is corneal edema, so if you do the cataract procedure first and allow the eye to heal for a couple of weeks, the retina surgeon will have a much easier time doing the retinal procedure. If you do a combined procedure and the view becomes compromised for some reason, the retina surgery becomes more difficult,” he says.
Additionally, physicians say that certain conditions can benefit from performing staged procedures rather than combined ones.
“For example, I was recently consulted by one of our local retina colleagues about a patient who had retinal detachment surgery and silicone oil in the eye. The oil needs to stay in the eye for at least six months, but the cataract is already pretty advanced, and the retina specialist is having a difficult time seeing into the back of the eye. He would like me to perform cataract surgery first with the oil still in the eye, and then once the patient reaches six months with the oil in the eye, the retina specialist will perform the silicone oil removal. That course of action would be safer overall for the patient,” Dr. Kao says.
Pearls for Surgery
Dr. Kao recommends a hydrophobic acrylic IOL for cataract patients who also have a retinal condition. “We want to avoid silicone IOLs in those patients because, if a patient needs silicone oil in the future, the vision can be compromised due to fogging of the IOL or adherence of the silicone oil to the IOL,” he says.
Dr. Devgan recommends a monofocal IOL. He advises to avoid lenses that have rings in them, like trifocal or multifocal lenses, because those will compromise some of the vision quality, and these patients may already have a compromised macula.
Dr. Weng recommends teasing out the symptoms as best as you can. “Although it’s impossible to definitively attribute a certain symptom to a specific pathology, it is important for the treating surgeon to tease out the symptoms,” she says. “If a patient presents with a cataract and a very mild epiretinal membrane, and he or she says, ‘I’m having decreased night vision’ or ‘I’m having a lot of glare,’ these are symptoms much more consistent with a cataract versus an epiretinal membrane, which typically presents with blurry vision or metamorphopsia. In situations like that, it may be a better decision to take a staged approach where you remove the cataract and then see how the patient does before you do anything with the epiretinal membrane.”
She adds that there’s an art to making these decisions, and she lets every patient know all the options so that shared decision-making can be practiced. “In every case where I’m considering combined surgery, I also present the option of doing it staged,” Dr. Weng says. “That way, patients will feel reassured that they’re making the most informed decision possible and are playing an active role in their own care.”
Another argument for performing combined surgery is that a vitrectomy can accelerate cataract progression within two years. “For many of our elderly patients who are already coming in with a cataract at baseline, it can be beneficial to combine the vitrectomy and cataract surgery so that they can avoid an inevitable second surgery down the road,” she says.
To increase the chances of success in combined cases, Dr. Weng prioritizes communication with her co-surgeon. “Before we even step into the operating room, I like to speak with him or her about trocar placement, wound location, and order of steps,” she says. “That way, the surgical territory is mapped out and neither encroaches upon the other’s space.”
She also has a pearl for retina surgeons: “Most of us use 5- to 10-cc retrobulbar blocks to anesthetize our patients,” Dr. Weng says. “For combined cases, it’s important to remember to limit the volume injected in order to avoid excess posterior pressure. I’ll typically inject 3 cc and then immediately apply pressure to the globe afterwards. Then, I save the rest of the block so that it can be used to supplement anesthesia if needed once the cataract has been taken out.”
Another tip is to consider placing the infusion line at the start of the case. Dr. Weng typically has the cataract surgeon perform his or her procedure first, and then she performs the retina surgery. However, she notes that when trocars are placed during vitrectomy, the globe pressure can be transiently increased to 70 mmHg.
“Obviously, when we’re working alone, this transient pressure spike isn’t as concerning because we don’t generally have open wounds,” she says. “But in combined cases where there may be multiple pre-existing wounds (like a 3-mm corneal wound) by the time the field is turned over to me, I prefer to pre-place my infusion line. This way, when I’m ready to start my portion, I simply attach the infusion line without having to worry about globe collapse or prolapse of intraocular contents.”
Dr. Weng highly recommends suturing all wounds in combined cases. Even if a cataract wound might normally be stable without a suture, the retina surgeon may significantly elevate the globe pressure via infusion line placement, scleral depression, or intentionally increasing the infusion pressure for hemostasis. A simple 10-0 nylon suture through the corneal wound, and maybe even the paracenteses, can protect globe stability. “Similarly, I also recommend that retina specialists suture all their sclerotomies,” she adds. “There’s often many wounds by the end of these combined cases, and you really want to limit the chance of hypotony or other postoperative complications.”
Dr. Devgan advises cataract surgeons to make a longer incision that seals well. “Additionally, sometimes it is easier and more accurate to do the lens calculations before the vitrectomy,” he says. “If the vitreous is removed, the new intraocular lens will tend to sit a little deeper in the eye. So, if I’m doing cataract surgery on a patient who already had a vitrectomy, I actually need to change my lens calculations a bit by adding a little bit to the IOL power. So, in general, lens calculations are a little bit easier in an eye where you do the cataract first.”
It is also important to check the placement of the IOL. If the vitrectomy is done as the second procedure, Dr. Weng says that the IOL can potentially shift out of place as a result of the manipulation of the eye. “Before I close up on my end, I’ll invite my cataract colleague to come back in and take a quick look,” she says. “If he or she isn’t available, I take a quick look myself to make sure that the intraocular lens is still well-centered.”
The last thing to remember is to counsel the patient and let him or her know that the healing process may be a little bit longer. “In combined surgeries, there can be a bit more injection and inflammation of the globe, which can slightly prolong visual recovery,” Dr. Weng says. “Patients who have had previous cataract surgery in their other eye might be expecting to see well the next day, so I try to prepare patients appropriately so that they have realistic expectations.”
This article has no commercial sponsorship.
Dr. Weng is a consultant for Alcon, Alimera Sciences, Allergan/AbbVie, Novartis, DORC, Regeneron, RegenxBio and Genentech. Dr. Devgan is the owner of CataractCoach.com, a free teaching website. Dr. Kao is a consultant for and receives research funding from Johnson & Johnson Vision. Dr. Stone has no relevant financial interests to disclose.