Sutureless cataract surgery has been growing in popularity during the past decade. This technique has many advantages for both patients and surgeons. Patients achieve rapid visual recovery after phacoemulsification, and they experience less inflammation and practically no foreign-body sensation. Surgeons prefer this technique because of decreased surgical time and rapid visual recovery for their patients.
The one downside to clear corneal incisions is their apparent association with an increased risk of endophthalmitis. While they are meant to be self-sealing, at least some clear corneal incisions leak. The problem is that, rather than fluid leaking from the anterior chamber to the outside of the eye, there is a "suction effect" into the anterior chamber, allowing extraocular fluid to have access to the anterior chamber.
Increased Incidence of Endophthalmitis
The incidence of postoperative endophthalmitis is increasing, and the type of surgical incision appears to be a risk factor. A meta-analysis of studies conducted between 1979 and 1991 found an incidence rate of acute postoperative endophthalmitis after cataract extraction of 0.13 percent.1 This was before the introduction of sutureless incisions.
Another study examined patient records from 1992 to 1996 and found an incidence rate of endophthalmitis after cataract extraction with sutureless clear corneal incisions of 0.29 percent and an incidence rate of endophthalmitis after cataract extraction with scleral tunnel incisions of 0.02 percent.2 In 2003, there was a report of a statistically increased risk of endophthalmitis with clear corneal incisions compared to sclerocorneal incisions.3
Another 2003 study examined the possible association between clear corneal incisions with or without placement of a suture during cataract extraction and postoperative endophthalmitis.4 This retrospective, case-controlled study included 38 patients treated for culture-positive, acute post-cataract surgery endophthalmitis and 371 randomly selected control patients who underwent uncomplicated cataract surgery. Of the 38 patients with endophthalmitis, 17 had clear corneal incisions and 21 had a scleral tunnel incision. In 371 controls, 76 patients had clear corneal incisions and 295 had scleral tunnel incisions. Clear corneal incision was associated with a threefold greater risk of endophthalmitis than scleral tunnel incision.
One of the reasons for the increased risk of endophthalmitis after cataract surgery with clear corneal incisions is that these incisions are not always self-sealing. In 2003, a study examined the in vitro dynamic changes in unhealed clear corneal cataract incisions that might adversely affect the risk of intraocular infection.5 In this study, self-sealing clear corneal incisions were created in cadaveric human and rabbit eyes. Intraocular pressure was controlled with an infusion cannula, and optical coherence tomography was used to image incisions in real time as IOP was increased and decreased. Using an artificial anterior chamber, India ink was applied to the surface of cadaveric human corneas with clear corneal incisions to detect possible flow of surface fluid along the incision. IOP was varied by raising and lowering the infusion bottle so as to simulate the variation in IOP that would occur with successive blinks.
|
|
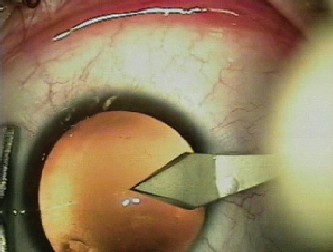
| Figure 1. Clear corneal incision for a standard cataract surgery through phacoemulsification in a patient. The dotted line represents the intrastromal tunnel of the incision, in arectangle-shaped configuration (less stability). |
|
|
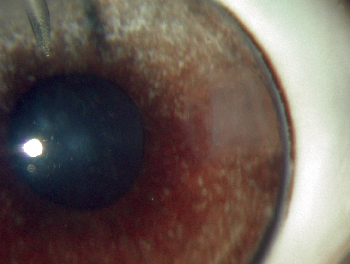
| Figure 2. Clear corneal incision in a rabbit eye. The dotted line shows the limits of the intrastromal tunnel, in a square-shaped configuration (more stability). |
In a second study, the same group evaluated the effect of IOP, location of the incision and angle of cataract incisions on wound apposition and sealing in post-mortem globes.6 This ex vivo laboratory investigation included 20 rabbit eyes and 14 human eyes. Self-sealing clear corneal, limbal and scleral incisions were created, and IOP was controlled with an infusion cannula. Incisions were made at a variety of angles, and OCT was used to image the incisions in real time as the IOP was varied by raising and lowering the infusion bottle. This was done to simulate the variation in IOP that would occur with blinking or squeezing the eye.
With each type of incision, OCT demonstrated the dynamic nature of cataract wound morphology as IOP fluctuated. Generally, higher IOPs were associated with more tightly sealed wounds than lower IOPs, but this varied according to the location and angle of the incisions. More perpendicular incisions, relative to the surface tangent, sealed less well than incisions created at smaller angles at higher levels of IOP. At lower IOPs, the opposite was observed, in that more perpendicular incisions sealed better than smaller incision angles.
The authors concluded that changes in IOP may result in variable and sometimes poor wound apposition in sutureless cataract incisions. The type of incision and angle of the incision may affect the likelihood of inoculation of the aqueous humor with potentially pathogenic bacteria. For each type of incision, there may be a critical angle at which the incision is better able to withstand fluctuations in IOP.
Testing the Seal
In 2004, my colleagues and I published a study that evaluated the self-sealing properties of standard clear corneal cataract incisions during application of mechanical external pressure and during controlled fluctuation of IOP.7 The study included eight fresh human donor globes, which were prepared for Miyake video microscopy. A standard, two-plane 3-mm clear corneal incision was created, and a 3-mm by 3-mm sponge soaked with India ink was placed on the wound surface. One globe with a sutured corneal wound served as the control. A transcleral cannula was inserted and connected to a bottle of saline. IOP was varied by changing the bottle height. External pressure was applied through manual contact on different regions of the cornea.
|
|
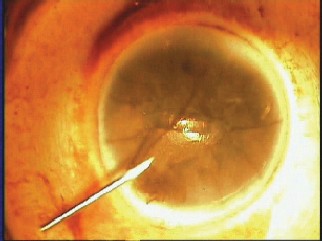
| Figure 3. Miyake view of the posterior cornea. Internal aspect of the wound (line) and the track of India ink flowing inside the eye (arrows) after mechanical stimulation of the vicinity of incision. |
Four of seven eyes demonstrated intraocular presence of ink. Three eyes experienced this only after external digital manipulation, as might simulate the pressure applied through the lid while opening an eye to apply drops postoperatively. In our model, the self-sealing properties of sutureless clear corneal wounds appeared compromised. Fluid did not leak out, but did "leak in." The results of this study helped us to gain insight into the possible mechanisms involved in the inflow of extraocular fluid into the eye through clear corneal incisions.
Reducing the Risk of Endophthalmitis
To date, no configuration of a clear corneal incision has been found to be completely safe. However, modifications to the technique have been proposed and should be considered in clinical trials.
One such modification includes adding a simple step to close incisions securely. This method was developed by Michael Y. Wong, MD, and he calls the method stromal hydration of a supraincisional pocket or the "Wong Way."8
The first step is creating the pocket. Just central or anterior to the surgeon's normal clear corneal or limbal incision site, he or she makes one or two stabs into the anterior stroma with a keratome. The goal is to create a triangular pocket with its tip toward the pupil. Then, the surgeon performs a standard keratectomy with the starting point just peripheral to, and the pass directly beneath, the pocket. At the completion of a standard cataract procedure, the surgeon reforms the anterior chamber and hydrates the tip and edges of the triangular, supraincisional stromal pocket with balanced salt solution until the stroma whitens. This technique was designed to prevent microleaks; however, its efficacy has not been confirmed yet in experimental models.
The design of the clear corneal incision is important for creating a well-sealed incision. Important factors include a relatively long tunnel as compared with the chord length. A longer tunnel provides more apposition of the wound. The longer the incision, the more likely there is to be a sealing effect at the end of of the incision.
Some surgeons have suggested using antibacterial drugs pre-, intra-, or postoperatively to reduce the risk of endophthalmitis. This approach might be valuable if it maintains therapeutic levels of drug within the aqueous long enough to allow the wound to "seal" as a result of epithelial closure and perhaps some stromal healing as well.
Placing a suture in the wound, we have shown, does prevent India ink ingress in our laboratory model.9 So, this is an option. However, using a suture might induce corneal cylinder, cause foreign-body sensation, and require removal, so this solution is not ideal.
New Alternatives?
An alternative to sutures is an adhesive. Using a biodegradable adhesive to seal the wound would eliminate the problem of having to remove the suture. Adhesives are currently being studied for use in corneal wounds, although they have not yet been used for this specific purpose.
One problem with adhesives is that they would add time to the procedure. Some adhesives require two substances. One substance is the adhesive, and the other substance is used to activate it. Alternatively, some others are activated by light from a laser. This makes the process a bit more complicated and time-consuming.
Large Numbers Needed for Studies
Evaluating the effect of medications or technique modifications on endophthalmitis rates is difficult. Endophthalmitis is very rare, and large numbers of patients are needed to detect a change in incidence rates.
It is worth our while, however, to continue to search for the perfect incision configuration or to find alternatives to make the actual incisions watertight. Endophthalmitis, when it does occur, is difficult to treat, and the potential outcome is blindness.
Dr. Behrens is a cornea/cataract surgeon and researcher at the Wilmer Ophthalmological Institute, Johns Hopkins University School of Medicine. Contact him at (410) 502-0461 or abehrens@jhmi.edu.
1. Powe NR, Schein OD, Gieser SC. Synthesis of the literature on visual acuity and complications following cataract extraction with intraocular lens implantation. Cataract Patient Outcome Research Team. Arch Ophthalmol 1994;112:239-252.
2. John ME, Noblitt R. Endophthalmitis: Scleral tunnel vs. clear corneal incision. In Buzard KA, Friedlander MH, Febbraro JL (eds): The Blue Line Incision and Refractive Phacoemulsification. Thorofare, NJ: SLACK. 2001:53-56.
3. Nagaki Y, Hayasaka S, Kadoi C. Bacterial endophthalmitis after small-incision cataract surgery: Effect of incision placement and intraocular lens type. J Cataract Refract Surg 2003;29:20-26.
4. Cooper BA, Holekamp NM, Bohigian G, Thompson PA. Case-control study of endophthalmitis after cataract surgery comparing scleral tunnel and clear corneal wounds. Am J Ophthalmol 2003;136:300-305.
5. McDonnell PJ, Taban MT, Sarayba M, et al. Dynamic morphology of clear corneal cataract incisions. Ophthalmology 2003;110:2342-2348.
6. Taban M, Rao B, Reznik J, Zhang J, Chen Z, McDonnell PJ. Dynamic morphology of sutureless cataract wounds—Effect of incision angle and location. Surv Ophthalmol 2004;49(Suppl 2):S62-S72.
7. Sarayba MA, Taban M, Ignacio T, Behrens A, McDonnell PJ. Inflow of ocular surface fluid through clear corneal cataract incisions: A laboratory model. Am J Ophthalmol 2004;138:206-210.
8. Wong MY. Securing clear corneal incisions. Cataract Refract Surg Today 2003;3:25-27.
9. Taban M, Sarayba MA, Almeda TI, Behrens A, McDonnell PJ. Ingress of India ink into the anterior chamber through sutureless clear corneal cataract wounds. Arch Ophthalmol (in press).