 |
|
Investigators from the United Kingdom have identified possible novel risk factors for posterior capsular rupture during cataract surgery. |
Modern cataract surgery is extremely safe, but the sheer volume of procedures performed—roughly four million each year in the United States alone—means that adverse events will affect a sizable number of people. As the intraoperative complication of posterior capsular rupture can negatively impact final visual outcome for patients, researchers and clinicians alike would like to know what risk factors are present for PCR during cataract surgery.
A shallow anterior chamber depth of <2.2 mm was associated with increased PCR rates, possibly due to iris prolapse being more common, thus surgeons making longer tunnels and increasing corneal distortion and impairing visualization, or more directly increasing proximity of instruments to the posterior capsule in a shallow anterior chamber.
Included in a new investigation were eligible operations from centers supplying data to the U.K. national cataract audit with complete data, including patients’ sex, age at surgery, anterior chamber depth and preoperative visual acuity. A model was designed to identify risk factors and calculated the odds ratios of factors on PCR likelihood. Results were recently published in the British journal Eye.1
A significant 961,208 cataract operations were included, performed on 682,381 patients from 136 different centers and with 3,198 different surgeons. Only 1.01 percent of these surgeries had PCR occur, with a median age of 75.7 for the first eye surgery and 76.7 for the second among affected patients. Of those who had PCR occur, 53 percent were women. The highest risk factors for PCR included a less experienced trainee surgeon, pseudoexfoliation/phacodonesis, younger men and brunescent/white/mature cataract. Other identified risk factors were glaucoma, worse preoperative visual acuity, previous intravitreal therapy, high myopia, previous vitrectomy, systemic diabetes, diabetic retinopathy, amblyopia, older age, shallower anterior chamber depth and an inability to lie flat and cooperate.
As part of their discussion, the study authors relay that these findings confirmed previously known risk factors of increasing age, trainee surgeon, male sex, inability to lie flat and cooperate, systemic diabetes, diabetic retinopathy, smaller pupil size, mature cataract, glaucoma and pseudoexfoliation/phacodonesis, with corroboration of more recently reported risk factors, too, of previous intravitreal anti-VEGF therapy and worse preoperative visual acuity. What’s more interesting are the novel risk factors identified of high myopia, previous vitrectomy, shallow anterior chamber depth and amblyopia.
They elaborate more on individual risk factors, stating that one of the highest odds ratios was in younger men; however, they note that the age/sex interaction term diminished this ratio in older patients, with similar risk in sexes by age 85, and even a switch of women having greater risk after 90 years of age.
The authors theorize that the novel risk factor of high myopia might affect PCR by a longer axial length making surgery more challenging, but previous literature hasn’t found an association between axial length specifically and PCR, thus suggesting other mechanisms at play, like higher cataract density.
Those who had a pervious vitrectomy may have had higher PCR risk due to altered fluid dynamics, unstable posterior capsules or posterior lenticular touch during vitrectomy, with the underlying increased PCR risk in these eyes potentially overlapping with high myopia, since the two possess a strong correlation.
Generally, the authors convey that “this analysis provides an update to the current risk adjustment model for PCR with the quantification of additional risk factors.”
As they explain, this information “will facilitate a bespoke, contemporary risk assessment tailored to an individual patient’s operation, thereby allowing more informed patient counseling, appropriate case allocation and adoption of precautionary measures to minimize the risk of posterior capsular rupture during surgery.”
1. Sim PY, Donachie PHJ, Day AC, Buchan JC. The Royal College of Ophthalmologists’ National Ophthalmology Database study of cataract surgery: A risk factor model for posterior capsule rupture. Eye (Lond). September 19, 2024 [Epub ahead of print].
First Whole-eye Transplant at One Year
In JAMA, surgeons at NYU Langone Health in New York City recently provided an update on the first whole-eye transplant that they performed a year ago.1
In their paper, the surgeons note that whole-eye transplantation has been stymied in the past “by a lack of microsurgical techniques for vascular anastomosis and a modern understanding of immunosuppression leading to transplant failures.” They add that there hasn’t been a workable surgical approach to such transplants, and that “retinal ischemia/reperfusion, and absence of optic nerve regeneration with restoration of oculo-cortical-visual pathways have remained substantial impediments to whole eye transplant.”
They say that recent studies, however, have explored the concept of whole eye transplant in the context of craniofacial transplant, adding that, “Vascularized composite allotransplantation (VCA) has revolutionized the paradigm of craniofacial reconstruction by recapitulating the lost anatomic and functional units that otherwise are insufficiently addressed with conventional reconstructive techniques.”
It’s with this VCA technique that they approached the treatment of a 46-year-old patient who had unfortunately sustained a high-voltage electrical injury in June 2021, resulting in loss of his left eye, left eyelid, nose, lips, and a large volume of facial tissue including skin and mimetic musculature.1
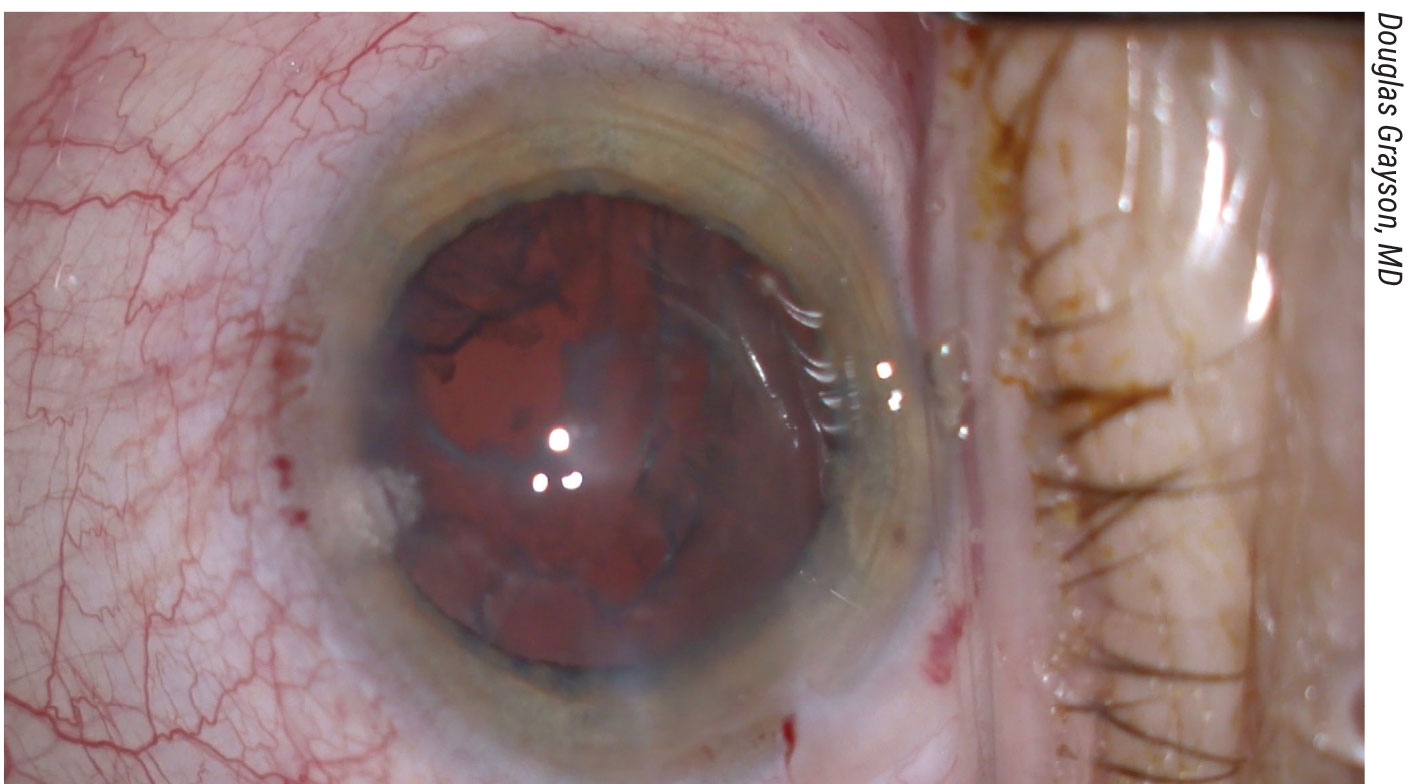
The patient ultimately underwent a combined whole eye and face transplant from a compatible donor with primary optic nerve coaptation and conventional postoperative immunosuppression. The physicians say that, per fluorescein angiography, globe and retinal perfusion were maintained throughout the immediate postoperative period.
Optical coherence tomography showed atrophy of the inner retinal layers and attenuation and disruption of the ellipsoid zone. Serial electroretinography confirmed retinal responses to light in the transplanted eye. The surgeons say that structural and functional magnetic resonance imaging demonstrated the integrity of the transplanted visual pathways and potential occipital cortical response to light stimulation of the transplanted eye. At one year post transplant (postoperative day 366), there was no perception of light in the transplanted eye, the physicians say.
“The globe transplant remained viable in the context of a face transplant including orbital bony anatomy,” the surgeons say in their paper, “although with time and greater understanding, there may be potential for isolated globe transplant.”
1. Ceradini DJ, Tran DL, Dedania VS, et al. Combined whole eye and face transplant: Microsurgical strategy and 1-year clinical course. JAMA. September 9, 2024 [Epub ahead of print].
Combined Treatment for PDR: Sequence Matters
Initial treatment of patients with proliferative diabetic retinopathy often involves a combined approach using panretinal photocoagulation and anti-VEGF injections. Large randomized clinical trials usually prefer monotherapy, limiting the information available on the outcomes of combined treatment approaches and whether the sequence of PRP and anti-VEGF therapy has an effect. A new study published in JAMA Ophthalmology aimed to close this research gap by comparing the need for pars plana vitrectomy among patients treated with PRP first then anti-VEGF injections and vice versa.
The retrospective cohort study included more than 3,000 patients with new PDR diagnoses from the TriNetX EHR network, stratified by therapy with PRP and subsequent anti-VEGF or anti-VEGF and subsequent PRP. While the primary outcome was the need for PPV, secondary outcomes included incidence of PPV, vitreous hemorrhage or tractional retinal detachment. After propensity score matching, which controlled for baseline demographic characteristics and medical comorbidities, there were 1,377 patients in each of the two treatment groups. The average age was 63 years in both groups, and the sex ratio was nearly 50:50.
The results showed that patients in the PRP-first group demonstrated a higher risk of needing PPV over the course of five years compared to those in the anti-VEGF-first group, with similar associations at six months, one year and three years. This group also had higher rates of vitreous hemorrhage and tractional retinal detachment at the same four time points.
“While combined therapy for the treatment of PDR has gained popularity in clinical practice, as shown by the ASRS PAT surveys, if this study’s approach is considered, it is unknown if the order of treatment modalities affects outcomes,” the researchers explained in their paper. They cited one previous study that found “PRP after intravitreal conbercept injections (Lumitin; Kanghong Biotechnology) was associated with a reduced number of subsequent anti-VEGF injections compared with eyes treated with PRP before intravitreal conbercept at two years [six vs. 8.5 injections], despite no difference in visual and anatomic outcomes between cohorts.”
Furthermore, in the present study, which used a large, heterogenous, real-world database of matched patients with proliferative diabetic retinopathy, “administration of PRP first was associated with an increased risk of undergoing PPV, as well as developing vitreous hemorrhage and tractional retinal detachment, compared with anti-VEGF injection [first],” the study authors wrote.
Study co-author Amer Fadel Alsoudi, MD, has some thoughts on what’s behind the results. “Combined treatment is preferred practice among ophthalmologists across the world (supported by ASRS PAT surveys and real world practice),” he says, “with some evidence to support better outcomes than monotherapy (though no study that directly compares combined treatment with monotherapy). We recently published that monotherapy anti-VEGF may have improved outcomes than monotherapy PRP in a select cohort of patients. It’s perhaps the VEGF sequestration with anti-VEGF therapy that facilitates successful PRP and prevention of PDR complications.”
While the literature on this topic is growing, they caution that further research is still warranted to determine the optimal order of panretinal photocoagulation and anti-VEGF injections for treating proliferative diabetic retinopathy, especially considering the increasing popularity of this combined approach.
Dr. Alsoudi notes what actualy surprised him about the results. “[I was surprised by] the magnitude of difference regarding outcomes secondary to the order of treatment that remained significant at every time point observed,” he says. “When we ask questions in science, we often don’t expect results that support or reject our hypothesis—rather to better inform the public one way or the other. When we find a signal that hasn’t been explained yet, we’re surprised.
In terms of limitations, Dr. Alsoud notes that, “Without belaboring the point, de-identified large database studies that require accurate clinical coding are limited by the possibility of inaccurate coding—though physician compensation is reliant on accurate coding.”
1. Alsoudi AF, Wai KM, Koo E, et al. Initial therapy of panretinal photocoagulation vs anti-VEGF injection for proliferative diabetic retinopathy. JAMA Ophthalmol. August 29, 2024 [Epub ahead of print].



