An article in press at the Journal of the American Association for Pediatric Ophthalmology and Strabismus published a survey of pediatric ophthalmologists that quantified the significant impact the pandemic has had on them and, by extension, their patients.
The AAPOS says that the effects of the pandemic on their practices “portend access-of-care issues for children with blinding, if not life-threatening, diseases. As pediatric specialists struggle to keep their practices viable, children in America may suffer medical outcomes not anticipated in first-world countries.”
On the survey, which was administered in April 2020, the loss of clinic revenue was 76 to 100 percent in fully 75 percent of all responding practices (304/405). Overall, 93 percent of practices (377/405) reported at least a 51-percent loss of clinical revenue. For 93 percent of respondents (378/405), surgery revenue decreased by at least 76 percent during the survey period.
This survey also found that nearly 90 percent of pediatric ophthalmologists were either furloughed or had their salaries reduced; 10 percent of those in private practice filed for unemployment. If practices close, or limit Medicaid patients’ access to services—which the numbers on the survey indicate is a possibility—this will have an impact on economically-disadvantaged families’ access to care, the authors say.
Pediatric ophthalmologist Janine Collinge, MD, who practices at Connecticut Children’s Specialty Group, says the threat to patients is real. “The government programs that assisted practices based on medicare volumes left predominantly pediatric practices and childrens’ hospitals in the lurch for how they were going to find financial support to survive,” she says. “Pediatric ophthalmology is already an underserved subspecialty, so this field is not necessarily amenable to tolerating the stresses of COVID the way other fields may be.”
In addition to the economic impact, the survey also detailed how the infection risk—or just the fear of infection—has the potential to hinder patient care for kids who really need it. The authors explain that recent studies have shown that this coronavirus can spread readily through crying or screaming, two behaviors associated with pediatric patients. The article cites data from a personal communication with Maurice O’Gorman, PhD, Chief of Laboratory Medicine at Children’s Hospital Los Angeles. The article states, “testing of healthy, asymptomatic preoperative patients in the Southern California/Los Angeles area found that 1.9 percent of asymptomatic children were COVID-19 positive. This rate of positivity increased in tested children from local pediatric clinics, with degree of positivity noted with symptoms of 5.8 to 21.6 percent. Similar tests confirmed that nearly 10 percent of children in the Los Angeles area are COVID-19 antibody positive. Extrapolating from O’Gorman’s data, a daily pediatric ophthalmology clinic of 50 patients in Southern California could be expected to have at least one presymptomatic child carrying
COVID-19.”
Risk of Infection During Exams
Since every ophthalmologist wonders about the risk of infection during a routine clinic day, a group of ophthalmologists in Izmir, Turkey, performed an experiment that was published in the September issue of JAMA Ophthalmology.
In their report, the physicians say that, though person-to-person contact through airborne droplets is believed to be the main route of viral transmission, some have suggested that contaminated surfaces might also play a role. They cite a study of cruise-ship outbreaks of SARS-CoV-2 that found viral RNA on the surfaces in ships’ cabins up to 17 days after patients disembarked.1 Another study reported viable SARS-CoV-2 in aerosols up to three hours post-aerosolization.2 They note, however, that the latter study didn’t mimic ophthalmic exam room conditions, but instead used a nebulizer and a Goldberg drum that generates aerosols. “An important limitation of lab studies is the difficulty of evaluating individuals who are infected and asymptomatic in routine examinations,” the authors wrote. “Since we are examining patients who are asymptomatic during the pandemic, we wanted to know if we could detect COVID-19 viral material at the end of a day of examinations of patients who were asymptomatic and seen in an eye examination room.”
Before beginning the study, the researchers eliminated patients with symptoms, as well as patients and companions with a history of travel to affected areas (March 2020) or who had had contact with confirmed or suspected COVID-19 cases. In the exam room, they used a plastic shield on the slit lamp.
The room was cleaned and remained unused before the study. During the study, chin and forehead rests were wiped with isopropyl alcohol between patients. The same physician performed all exams, and one health-care worker visited the room.
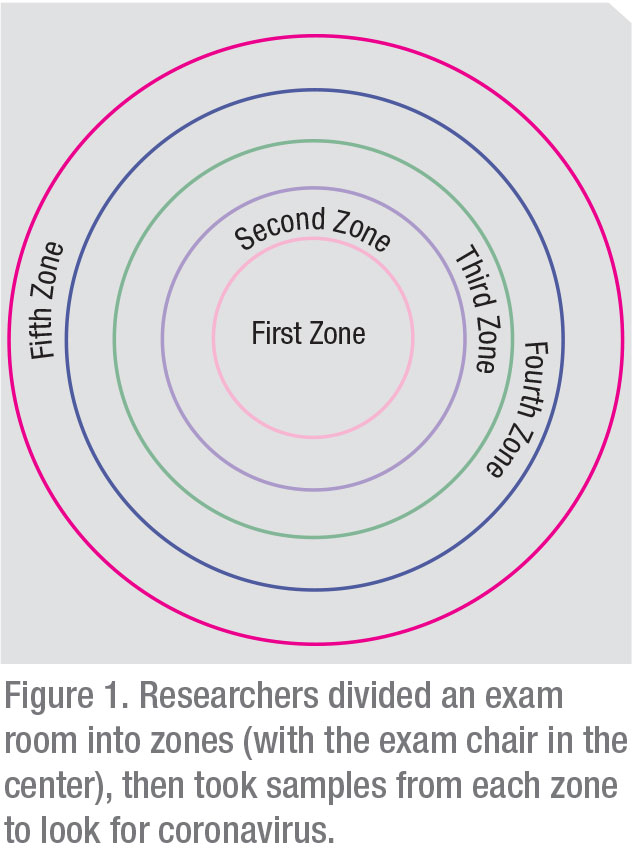 |
The researchers divided the room into five zones (See Figure 1), set up as concentric circles, with the patient’s chair in the center (zone 1). Samples were taken at each 1 m of distance away from zone 1, eventually defining the five zones. According to the zone definition, the slit lamp shield, biomicroscope stage and phoropter were in zone 1; the tonometer was in zone 2; the desk was situated in zones 3 and 4; and the door handles were in zone 5.
The day of the experiment, 29 patients came to the hospital for an exam. Seven of them were directed for COVID-19 tests following triage and didn’t go to the exam room. Overall, 31 visitors entered the room, of whom 22 underwent exams. The mean exam time was 9 ±4 minutes (range: 5 to 13 minutes). One ophthalmologist collected 14 samples from the surfaces in the room—seven before the exams and seven after. All pre-exam samples were negative. Two post-exam samples that were collected from zone 1—from the slit lamp shield and phoropter—were found to be positive for SARS-CoV-2 viral material.
Though the study gives an idea of the potential risk from asymptomatic patients, the authors acknowledge its limitations: The RT-PCR testing that was used on the samples only confirms the presence of viral material, but not the viral load or infectivity of it. It was also a small sample size. The authors wrote, “it was not known whether patients, companions and the health-care worker developed symptoms… . Further studies are needed to determine the clinical relevance of these findings.” REVIEW
1. Moriarty LF, Plucinski MM, Marston BJ, et al. Public health responses to COVID-19 outbreaks on cruise ships—worldwide, February-March 2020. MMWRMorb Mortal Wkly Rep 2020;69:12:347-352.
2. an Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med 2020;382:16:1564-1567.
 |




