|
| Image courtesy of Getty. |
Retinal vein occlusion is associated with cardiovascular risk factors, and it’s possible that such incidents may also carry predictive value for a future subsequent vascular event or mortality risk. In a new study, researchers examined rates of stroke, myocardial infarction (MI), deep vein thrombosis, pulmonary embolism and death in patients after RVO and found patients at an increased risk of these vascular events.
A total of 45,303 patients with diagnosis of RVO and a control group of patients with cataract were included. Patients were excluded if they had history of stroke, MI, deep vein thrombosis or pulmonary embolism within two years of diagnosis of RVO or cataract.
With a closely matched control population to assure parity in age, gender, ethnicity, race and systemic comorbidities of diabetes, hypertension and hyperlipidemia, this study found increased risks of death and subsequent vascular events, including stroke and MI, after RVO.
According to Ehsan Rahimy, MD, an adjunct clinical professor at Stanford University School of Medicine, Palo Alto, California, and a co-author of the study, previous studies exploring this topic were inconsistent. “There have been some well-publicized population studies out of Southeast Asia with mixed findings. One study out of Taiwan that analyzed a national database showed no increased risk of these systemic events (stroke or myocardial infarction) if somebody has a retinal vein occlusion, whereas a separate study from a Korean national database did demonstrate an increased risk,” he says. “Prior to our study we had conflicting results in the literature, which makes it challenging to know how to best counsel patients when these events occur.”
The study authors were able to evaluate such a large population retrospectively using the TriNetX network (Cambridge, Massachusetts), an electronic health records research network comprising multiple large health organizations within the United States and globally. “There were three unique advantages of our study design to investigate systemic correlations with RVOs over what has been previously published,” says Dr. Rahimy. “Number one was the sheer numbers of patients included for analysis even after applying fairly stringent inclusion/exclusion criteria. We ended up with over 45,000 patients with retinal vein occlusions with a propensity-matched control group of 45,000 patients; whereas these previous studies’ numbers were in the low single-digit thousands. A second advantage of this TriNetX network that benefited our study design is the patient data was acquired from multiple countries—not just here in the United States. As of the last time I checked, there were 19 countries worldwide participating in the research network. By virtue of that, we’re allowed to assess a very diverse and heterogeneous patient population with vein occlusion. Previous studies tended to be very homogenous populations (i.e. Taiwan, Korea), while our study is presenting more of a balanced representation of this condition across different patient populations.”
The second advantage of this study was the long-term follow up. “We were able to carry follow-up out to 10 years after the index event (i.e., the time of RVO onset) to better inform patients’ systemic risk,” continues Dr. Rahimy. “To obtain that degree of longitudinal long-term follow up is unique about this TriNetX platform, and was a key strength of our study.”
“The key takeaway of the study is that patients who get retinal vein occlusions do carry a higher risk throughout their life, or at least out to the 10 years measured, of experiencing strokes, heart attacks and even death,” says Dr. Rahimy. “The two other categories we measured out of interest were other systemic venous occlusive conditions, such as deep vein thrombosis or pulmonary embolism,” he continues. “Logically, one may surmise that someone with an RVO may have an elevated risk of other venous occlusive events in the body, too. But interestingly, this didn’t turn out to be the case in our study. This may invite some speculation as to what is really going on when a patient presents to you with retinal vein occlusion. Is the underlying pathophysiology more in line with a venous clot, or rather, is this more indicative of broader vascular disease (arterial and venous) in that patient’s body (i.e. could this be suggestive of similar microvascular changes within an organ like the brain)?”
Examining central RVO and branch RVO separately may be needed to explore the underlying mechanism, as both showed elevated risk of death when comparing these patients, but no difference in stroke, MI, DVT or PE at the same time points.
“I think most of us would agree that not all retinal vein occlusions are the same,” Dr. Rahimy says. “Because of ICD-10 coding we could only break them up by BRVO or CRVO. We didn’t find any major signal differences in these sub-types, but in these big-data studies, you’re dependent on ICD-10 coding diagnoses to be accurate. However, not all ICD codes capture the different things we see in retina. A great example is that we have ICD codes for CRVO, we have ICD codes for BRVO, but we don’t have ICD coding for hemiretinal vein occlusions, and people argue in our field that perhaps HRVOs are a separate subgroup altogether. So, how an HRVO ultimately gets classified depends on a given physician’s coding tendencies. Do they classify it as a CRVO or as a BRVO in their EHR? In the data, you probably get a mix of both throughout it.”
Overall, ophthalmologists “should be aware of elevated risk of death and vascular events including MI or stroke in patients presenting with RVO,” the researchers concluded.
“Ultimately, this study heightens the importance of making sure patients’ systemic comorbidities are being optimally controlled and of ommunicating these findings to their core care team when they have a vein occlusion,” Dr. Rahimy says. “In my practice environment, a large multidisciplinary network, whenever I have somebody with a vein occlusion, I’m closely communicating with their PCP about this event that happened, how we’re treating it and how it’s very important to comanage any systemic comorbidities. We often see some patients come in with RVOs who may not initially have other issues going on elsewhere in their body, and this is where I think this type of study is valuable. Patients should know, even if they don’t have anything now, it behooves them to take good care of themselves, lead a healthy lifestyle and continue with routine care assessments with their primary care doctor to check for the development of potential underlying cardiovascular or cerebrovascular risk factors down the line."
1. Wai KM, Ludwig CA, Koo E, et al. Risk of stroke, myocardial infarction, deep vein thrombosis, pulmonary embolism and death after retinal vein occlusion. Amer J Ophthalmol. August 23, 2023. [Epub ahead of print].
AAO Analyzes SLT as First-line Therapy
Periodically, the American Academy of Ophthalmology conducts Ophthalmic Technology Assessments to assess the clinical efficacy, effectiveness and safety of new and existing procedures, drugs, diagnostics and screening tests. Recently, selective laser trabeculoplasty underwent systematic review—its first since November 2011. The report, published in Ophthalmology, confirmed its clinical safety and identified areas for further research.1
A total of 30 articles—including the LiGHT Trial—were included. Evidence level ratings were assigned, with 19 studies assigned a level I rating and 11 studies assigned a level II rating.
The data from level I studies show that SLT has long-term effectiveness as a primary or supplemental treatment to medical therapy in open-angle glaucoma. First-line SLT and medications showed equivalent IOP control for open-angle glaucoma and ocular hypertension and may also be more cost effective and provide better long-term disease control than medications. Interestingly, SLT wasn’t found to result in measurable quality-of-life improvement.
In level I studies, SLT and ALT were found to be equivalent in safety and long-term efficacy in several studies, with repeat SLT possibly more effective than repeat ALT in the long-term. Level I studies also showed that SLT’s IOP lowering was equivalent to several other modalities including micropulse laser trabeculoplasty, pattern-scanning laser trabeculoplasty and titanium-sapphire laser trabeculoplasty. Level II data showed equivalence with excimer laser trabeculoplasty.
Additionally, studies indicated that perioperative corticosteroid and NSAID drops didn’t hinder the treatment’s IOP-lowering effects, though the reported impact of the drops varied across studies.
The review also identified several areas for further study, including a need for more randomized clinical trials with diverse patient populations and more randomized studies on treatment settings and repeatability.
1. Takusagawa HL, Hoguet A, Sit AJ, et al. Selective laser trabeculoplasty for the treatment of glaucoma: A report by the American Academy of Ophthalmology. Ophthalmology 2023;1-11.
Endophthalmitis in Glaucoma Surgery vs. Cataract Surgery
 |
|
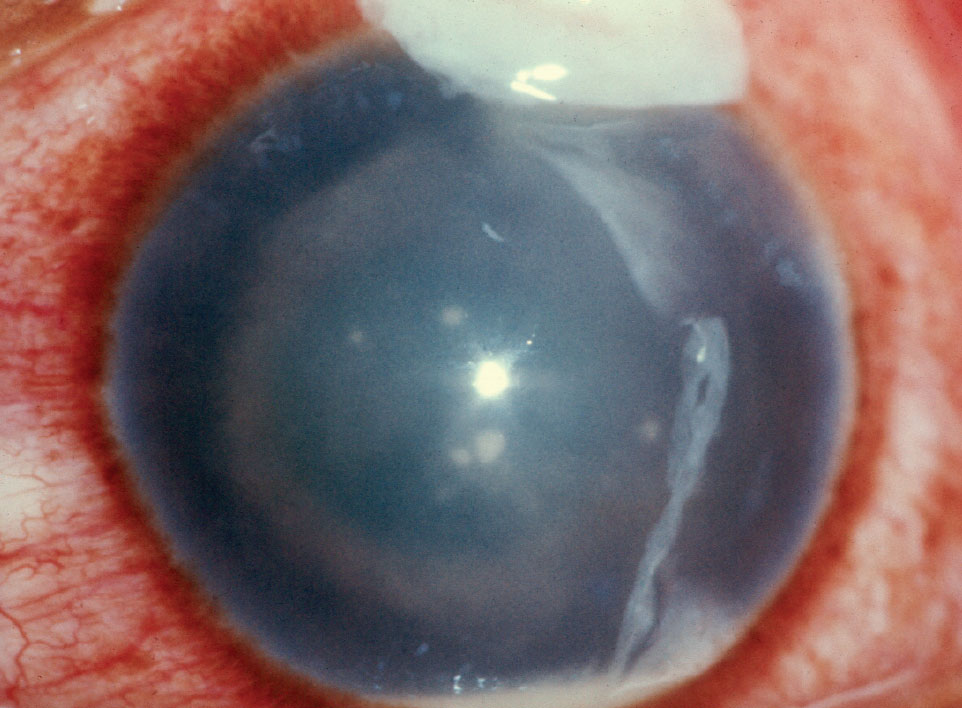
In the study, the onset of endophthalmitis after glaucoma surgery was one to two weeks later than cataract surgery or MIGS. |
Infamous for being “the most feared complication” of ocular surgery, endophthalmitis is fortunately rare but occurs more often after glaucoma surgeries than other types of intraocular surgeries. In order to better understand the risk factors and the incidence of endophthalmitis, which can vary significantly across different types of glaucoma surgeries, researchers analyzed glaucoma surgery outcomes using a large Medicare claims database. They found that incidences were nearly double those of cataract surgery.1
In the retrospective, longitudinal study, 466,928 glaucoma surgeries were identified based on 2016-2019 Medicare Fee-For-Service and Medicare Advantage claims of patients 65 and older. Endophthalmitis cases within 42 days of surgery were identified based on ICD-10 codes. About two-thirds of the glaucoma surgeries were combined with cataract surgery. (The researchers used cataract surgeries alone [n=8,460,360] as a reference group.) Most of the glaucoma surgeries were MIGS (67.8 percent), followed by trabeculectomies (14 percent) and tube shunt procedures (10.9 percent). Other procedures made up 7.3 percent of surgeries.
A total of 572 cases of endophthalmitis occurred following all glaucoma surgeries (an incidence of 1.2 per thousand). The breakdown for incidences per thousand procedures were as follows: glaucoma surgeries alone 1.5, combined cataract/glaucoma 1.1 and cataract alone 0.8.
The researchers found that the median day of endophthalmitis diagnosis was later for glaucoma surgeries (16.5 days) than combined cataract/glaucoma (eight days) or cataract alone (six days).
They identified two significant risk factors for endophthalmitis with both standalone and combined surgery—tube shunts and Charlson comorbidity index. They also found that age and male gender were significant risk factors for only combined cataract/glaucoma surgeries.
“The median onset of endophthalmitis following traditional glaucoma surgeries was one to two weeks later than that following cataract or MIGS, suggesting that the wait time between sequential surgery on contralateral eyes should perhaps be slightly longer for traditional glaucoma surgeries unless immediate pressure lowering is needed,” the researchers explained in their Ophthalmology paper.
They added that the identified risk factors will be “relevant in assessing surgical risk for the individual patient” and may serve as a national benchmark for endophthalmitis incidence after glaucoma surgery.
1. Sabharwal J, Dai X, Dun C, et al. Early endophthalmitis incidence and risk factors following glaucoma surgery in the Medicare population from 2016 to 2019. Ophthalmology 2023. [Epub ahead of print].
Risk Factors for Exudative Progression in AMD
A group of international researchers from numerous countries, including Denmark, the Netherlands and the United Kingdom, systematically reviewed and reported the rate of exudative progression over time in patients with non-exudative macular neovascularization in age-related macular degeneration, as part of a review with prevalence and individual participant meta-analyses.1
Researchers searched 10 literature databases on March 26, 2023, for studies of consecutive patients with treatment-naïve non-exudative macular neovascularization in age-related macular degeneration.
The primary outcome of interest was time from diagnosis to exudative progression. Researchers conducted meta-analyses on the prevalence of exudative progression at one and two years. Wherever possible, they extracted individual participant data from studies and conducted an individual participant meta-analysis, as well as evaluated exudative progression using a time-to-event curve.
Researchers ultimately identified 16 eligible retina studies reporting on 384 eyes with non-exudative macular neovascularization.
Here are some of the results they reported:
- Exudative progression occurred in 20.9 percent (CI, 13.1 to 29.8) of eyes at one year and 30.7 percent (CI, 21.8 to 40.4 percent) of the study eyes at two years.
- Similar results were observed in the individual participant meta-analysis, showing exudative progression in 18.9 percent of eyes (CI, 13.5 to 26.3 percent) at one year and 31.3 percent (CI, 24.2 to 40 percent) of the eyes at two years.
- Risk factors for a fast exudative progression were presence of subretinal lipid globules, large macular neovascularization areas, rapid macular neovascularization growth, growth in pigment epithelium detachment height and width, appearance of a branching pattern and development of a hyporeflective halo around the MNV.
Researchers concluded that patients with non-exudative macular neovascularization in age-related macular degeneration were at high risk of exudative progression. They suggested that recognition of these lesions may enable better individualized follow-up regimens and closer monitoring to facilitate earlier identification of exudative progression.
1. Nissen AHK, Kiilgaard HC, van Dijk EHC, et al. Exudative progression of treatment-naïve non-exudative macular neovascularization in age-related macular degeneration: A systematic review with meta-analyses. Am J Ophthalmol 2023; Aug 31. [Epub ahead of print].
PVD As a Biomarker for Central Retinal Vein Occlusion
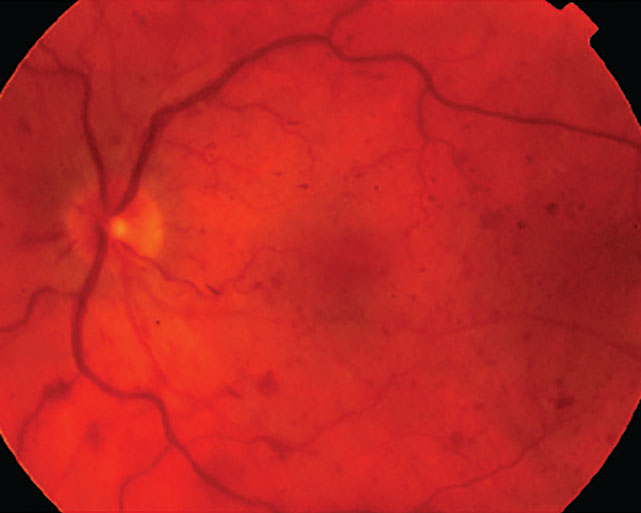 |
The vitreomacular interface is known to have important implications in the manifestations of retinal disease processes including retinal vein occlusion. Prior studies evaluating the influence of posterior vitreous detachment status in central retinal vein occlusion on retinal neovascularization in CRVO have suggested that complete PVD may be protective against neovascularization in eyes with ischemic CRVO. A recent study published in Retina has determined that cases of CRVO with complete PVD had significantly lower rate of cystoid macular edema (CME), lower central subfield thickness (CST) and lower anti-VEGF injection burden at one year.
The retrospective longitudinal cohort study assessed patients with acute, treatment-naïve CRVO diagnosed who had at least 12 months of follow-up.1 Clinical characteristics, treatment patterns and outcomes were analyzed between eyes stratified based on presence or absence of a complete PVD on OCT at presentation.
Of the 102 acute, treatment-naïve CRVOs identified, 52 (51 percent) had complete PVD at presentation and 50 (49 percent) did not. CST was significantly lower in those with complete PVD (12 months: 284.9 µm vs 426.8 µm; last follow-up: 278 µm vs 372.8 µm. One-year intravitreal injection burden was significantly less for those with a complete PVD than those without (5.1 injections vs 6.7 injections). At 12 months, those with complete PVD at presentation had significantly less CME than those with incomplete PVD at presentation (32 percent vs 65 percent).
“We suspect that the vitreous may serve as a reservoir and microenvironment for pro-inflammatory cytokines and molecules present in eyes with retinal vein occlusion,” the researchers wrote in their paper. “The presence of a complete PVD in eyes with CRVO contributes to reduced levels of locally circulating pro-inflammatory molecules at the vitreomacular interface, as has been demonstrated in eyes with diabetic retinopathy.”
They concluded that, “Assessment of the vitreomacular relationship on OCT at presentation in eyes with CRVO may serve as a prognostic imaging biomarker.”
1. Zheng Y, Woodward R, Feng HL, et al. Implications of complete PVD in eyes with central retinal vein occlusion. Retina. September 5, 2023. [Epub ahead of print].
Industry news Thea Addresses FDA Warning Letters After the FDA issued warning letters to eight companies, including Similasan AG/ New Approval Addresses Drug Shortfall Nexus Pharmaceuticals received FDA approval for fluorescein injection, USP 10%, available in 5 ml, single-dose vials in cartons of 10. Through the approval, the company said it hopes to address a supply shortfall of a critical medication on the Food and Drug Administration’s drug shortage list.
Outlook Therapeutics announced the FDA issued a Complete Response Letter in response to its application for ONS-5010, an investigational ophthalmic formulation of bevacizumab under development to treat wet AMD. While the FDA acknowledged the NORSE TWO pivotal trial met its safety and efficacy endpoints, it concluded it couldn’t approve the BLA during this review cycle due to several Chemistry Manufacturing and Controls (CMC) issues, open observations from pre-approval manufacturing inspections and a lack of substantial evidence. |