 |
In addition to documenting their outlook on presbyopic lens options, surgeons responding to this month’s IOL survey also shared their opinions on topics such as the most important features for an IOL to have, toric IOLs and managing complications of IOLs that require a secondary procedure to suture-fixate the lens. This month, the e-mail survey was opened by 1,089 of 8,171 subscribers to Review’s e-mail service (13.3 percent open rate) and, of those, 74 shared their responses. To see how your opinions on IOLs compare with theirs, read on.
Growing Interest
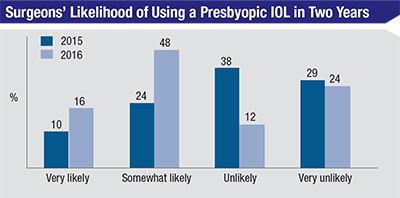
In last year’s IOL survey, surgeons didn’t have high hopes for presbyopic lenses: 38 percent characterized themselves as unlikely to use a presbyopic IOL within two years, and 29 percent said they were very unlikely to do so (for a total of 67 percent in the negative). Only 24 percent said they were somewhat likely to try them, and just 10 percent were very likely.
 |
Though the overall numerical results were positive, many of the surgeons who described themselves as somewhat likely to use a presbyopic lens maintained a guarded outlook on the devices. “There are still unanswered questions about the night-driving qualities of these lenses,” says a surgeon from Kansas.
A surgeon from Ohio is thinking along the same lines. “I hesitate to use a lens that can decrease a patient’s best potential visual acuity,” he says. “I also hate to risk problems with glare and halos. If a patient has a high priority for being spectacle-free, I will use them. Otherwise, I hate to leave patients with a lens that could impair their best corrected visual acuity and glare for the rest of their, hopefully, many years of future life.”
 |
| Surgeons on the survey ranked IOL features in terms of their usefulness using a numerical scale that ran from 1 (least useful) to 6 (most useful). The average scores are shown. |
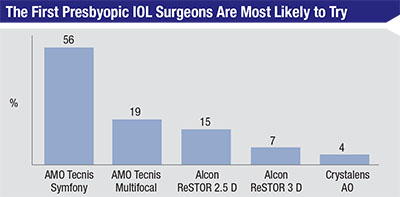
When asked which lens in particular they might like to try if they’re not yet performing presbyopic lens surgery, 56 percent of the respondents chose the Symfony. Nineteen percent named the Tecnis multifocal and 15 percent said the ReSTOR 2.5 D. (The rest of the results appear in the graph above.) “The Symfony has a longer range of focus and a wider central zone,” explains a surgeon from Oregon who says he most likely would try the Symfony. “Also, it takes the patient’s astigmatism into account.” A surgeon from Michigan also says he might implant the Symfony. “I’d like to try this new lens and see if the results are satisfactory,” he says. “Also, I’d like to see if the side effects are less.”
As for the surgeons who currently use presbyopic lenses, 34 percent are satisfied with their lens, and 27 percent are very satisfied. Thirty-seven percent say they’re somewhat satisfied, while 2 percent are unsatisfied.
“They’re not great, but they’re all we have,” says a surgeon from Maryland who implants the ReSTOR and the Tecnis multifocal. “There is a loss of contrast sensitivity, and we must screen patients carefully prior to use. These lenses can only be used in a small percentage of patients. We need a lens that mimics the natural lens in design.”
Sid Moore, MD, of Macon, Ga., agrees that this sort of lens would be helpful. “A true accommodative lens would be hugely beneficial,” he says. “Optical compromises with multifocals make predicting patient satisfaction difficult.”
A surgeon from Maryland who’s begun implanting the Symfony lens says that he’s had a positive experience so far. “I love the new Symfony lens,” he says. “Minimal halos, great optics. Patients say they have never seen like this before. I’d love it to have a little more reading vision and would also like to have better IOL formulas to improve outcomes.” Jon Weston, MD, of Roseburg, Ore., says he’s developed a way to deal with any near issues with Symfony. “I’ll mix a Tecnis multifocal with a Symfony if sharper vision for shorter working distances is needed,” he says.
Lens Design
Surgeons also took a look at the various elements of IOL design, commenting on which ones they preferred.
 |
Surgeons also ranked specific IOL features, such as toric correction or multifocality/bifocality, on a scale of one to six, with six being most important. (A graph of all the rankings appears above.) Toric design, with an average rank of 4.5, was thought to be most important, followed closely by asphericity/neutral asphericity at 4.2. Pseudo-accommodative motion, at 2.6, was thought to be least important. “The optics are the most important part of any lens,” avers Bruce Cohen, MD, of St. Louis. A surgeon from Montana says he doesn’t have a lot of confidence in multifocality/bifocality, saying, “Premium lens patients are a pain if they have the least little complaint after paying extra out of pocket.” A surgeon from Maryland also doesn’t think highly of this approach to presbyopia. “Right now,” he says, “it seems better to correct presbyopia on the cornea than within the lens.”
As the rankings suggest, surgeons are very impressed with toric IOLs. Fully 65 percent of surgeons rate toric performance as excellent, and 31 percent say it’s good. Fifty-seven percent of the surgeons use the AcrySof toric for most of their cases, and 33 percent use the Tecnis toric. Eight percent use the Symfony. “Toric IOLs provide excellent vision and have been a real advance in the treatment of patients with cataracts and astigmatism,” says Dr. Mamalis. Ron Glassman, MD, of Teaneck, N.J., agrees, saying, “This is the way to treat astigmatism.”
Some surgeons on the IOL survey, however, are more reserved in their praise for toric lenses, noting that, though they’re useful in many cataract cases, they can still have some issues, as well. “Often, there’s astigmatism that’s unaccounted for in the preop calculations,” says a surgeon from Michigan. “Also, the lens often rotates at the last second when trying to remove the viscoelastic.” A surgeon from Maryland says, “It’s difficult for the patient to go back to the OR if I need to rotate the lens; we also need a better system to ensure alignment in the OR.”
Complications
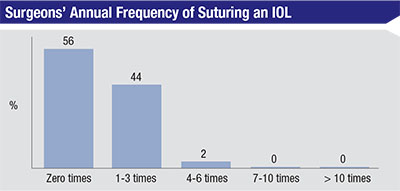
In another section of the survey, surgeons say there are times when implantations don’t go as well as hoped, and intraocular lenses need to be sutured in place in order to remain stable. Fifty-four percent of the respondents, though, say that this is rare, and they don’t need to do it in a given year. Forty-four percent, however, say they usually need to suture a lens one to three times per year, and 2 percent have to do it four to six times.
Surgeons also described various scenarios that called for suturing. “Suturing was performed for a dislocated IOL within the capsular bag or for a case of poor zonular support,” recounts Dr. Mamalis. A surgeon from Montana says his suturing was a result of “pseudoexfoliation and a dehisced capsular bag,” for which he sutured the lens to the iris, adding he’ll suture it “rarely to the sclera.”
Juan Nieto, MD, of Dubuque, Iowa, says his complicated IOL suturing cases usually involve “poor or no capsular support” and that he’s “comfortable suturing to the iris or glueing it to/tucking it into the sclera.” An ophthalmologist from Kansas says there’s one surgeon at his practice who performs all the challenging cases requiring IOL suturing. “He uses mostly an intrascleral fixation approach for them,” he says. “He does fewer cases using either polypropylene suturing to the iris, or Gore-Tex suturing to the sclera.” REVIEW



