Branch and central retinal vein obstructions are common retinal vascular disorders that are often associated with moderate to severe vision loss. Branch retinal vein occlusion is the most common retinal vascular disorder after diabetic retinopathy. Overall, 60 percent of all patients retain vision of 20/40 or better. The Branch Retinal Vein Occlusion Study demonstrated that laser photocoagulation improved vision in patients who had vision of 20/40 or worse due to macular edema; however, patients with vision worse than 20/200 did not do significantly better than with observation alone.1
The visual prognosis for many patients with central retinal vein occlusion is even more guarded, and laser treatment for macular edema is ineffective.2 Recently, several new surgical approaches for these entities have been described, and these may offer hope to our patients.
Adventitial Sheathotomy for BRVO
BRVO usually occurs at arteriovenous (A/V) crossings, and the arteriole crosses over the vein between 70 and 99 percent of the time.3,4 Many patients with BRVO have hypertension and arteriolosclerosis. As the arteriole and venule share a common adventitial sheath at A/V crossings, hypertensive and atherosclerotic changes to the arteriole narrow the venous lumen and cause turbulence in the vein that may lead to thrombosis.5
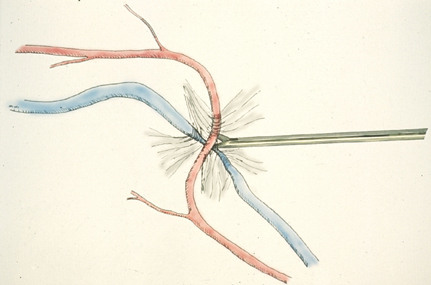 |
| Figure 1. This schematic shows the use of scissors to lyse the common adventitial sheath of an artery and vein. |
The goal of sheathotomy is to lyse the adventitial sheath that binds the vessels together. After performing a pars plana vitrectomy, a bent MVR blade or scissors are used to cut the sheath until the arteriole can be lifted off of the venule (See Figure 1). In the largest published series to date, postoperative visual acuity improved by an average of four lines in 10 of 15 patients, and the study included patients with macular ischemia as well as those with macular edema. However, several of these patients had symptoms for less than three months preoperatively, and the average follow-up was relatively short (five months).6 A longer-term study followed five patients who underwent sheathotomy for macular edema. All patients had initial vision of 20/200 or worse. At a minimum of five years after surgery, four of five patients had marked visual improvement ranging from 20/30 to 20/70.7
For patients with advanced vision loss caused by BRVO, in whom laser photocoagulation either has not helped or will likely not help, adventitial sheathotomy may offer a chance for long-term visual improvement.
Chorioretinal Venous Anastomosis
The purpose of chorioretinal anastomosis is to bypass the venous obstruction by enabling the venous system to drain directly into the choroidal circulation. This has been used for both branch and central venous obstructions. At a site at least three disk diameters away from the optic nerve and usually along the inferotemporal vein, a green argon laser using a power of 2.5 to 3.5 W creates a small spot to rupture Bruch's membrane and a second spot to rupture an adjacent venule. Fluorescein angiography may confirm a successful anastomosis, and additional treatments can be done six to eight weeks later, if needed.
This technique was described for patients with nonischemic central retinal vein occlusions who experienced progressive visual loss. In the study, investigators created a successful chorioretinal venous anastomosis in eight of 24 eyes, and all of these patients had improvement in vision and in their fundus appearance. However, six of the 16 patients in whom a successful anastomosis was not created also experienced an improvement in vision.
Interestingly, in the group in which a successful anastomosis was not created, five of 16 eyes evolved into an ischemic CRVO, while none in the successfully treated group became ischemic.8 Another study showed similar success in patients with CRVO, and found that this technique may be beneficial in patients with BRVO as well.9
Although these studies reported only mild complications, such as mild vitreous and retinal hemorrhages, and small to moderate amounts of scar tissue around the laser sites, other people have reported significant complications, including rubeosis, vitreous hemorrhage and neovascularization or traction at the laser site.
Experiences such as this appropriately are a concern to a number of retina specialists. However, close follow-up and immediate panretinal photocoagulation to areas that become ischemic can minimize the risk of rubeosis. Also, selective laser spots placed at the appropriate locations may help to achieve greater success.10
t-PA Injection in Eyes with CRVO
Tissue plasminogen activator, or t-PA, has been used for a number of years to treat stroke patients. Several reports cite patients with CRVO and CRAO treated with systemic t-PA who gained several lines of vision. Systemic t-PA can, however, cause cerebral hemorrhage and even death.
A recently described technique uses much less t-PA by cannulating a branch retinal vein. The study included 28 patients with both ischemic and non-ischemic CRVO, who had symptoms ranging from one week to 30 months. After a pars plana vitrectomy, a branch vein was cannulated and a 3- to 4-ml bolus of t-PA was infused into the vein. The vast majority of patients had at least a one-line improvement in vision, and more than 50 percent had at least a three-line improvement within six months postop. Twenty five percent of the patients developed vitreous hemorrhage, and there was one retinal detachment.11
This technique may work via several different mechanisms. Vitrectomy with peeling of the posterior hyaloid face may help reduce macular edema. t-PA itself may lyse the clot, and the bolus of fluid may "flush" the thrombus downstream. There has been active debate about the mechanism of action. In the treatment of strokes, most of the success of t-PA has come within the first few hours after the thrombotic event. Soon after forming, the thrombus becomes organized and in a long-standing occlusion, it may be difficult to dissolve.
Other evidence suggests that the inner retina may suffer irreparable damage after several weeks and that even if a clot is dislodged, the retina may be too damaged to recover. Also, if collateral vessels have time to form, t-PA may be routed away from the thrombus and may not reach it in sufficient amount to dislodge the clot.12
While the initial report of this technique is encouraging, further studies into mechanisms of action, as well as the success of this technique in the hands of other surgeons, are needed.
Radial Optic Neurotomy
One of the main pathogenic theories behind the formation of CRVO involves arteriole disease that affects the adventitial sheath that joins the central retinal artery and vein and causes turbulence that leads to thrombosis. Some view CRVO as possibly due to a compartment-like syndrome caused by increased pressure around the optic nerve head. If this is the case, they hypothesize that making an incision to decompress the optic nerve head would help relieve the obstruction.
In a published series of 11 patients, researchers used an MVR blade to make an incision through the scleral ring and lamina cribrosa at the nasal aspect of the optic nerve head. In the series, all patients had initial vision of 20/400 or worse, with a duration of one to seven months. Seven of 11 patients had final visual acuity of 20/200 or better, and five of 11 had vision better than or equal to 20/70. There were no operative complications reported.13
While this technique may decompress a "tight" scleral ring, our experience suggests that part of the effect may be due to the formation of collateral vessels at the site of the neurotomy (See Figures 2 to 4). The collateral vessels may allow restoration of more normal venous flow, allowing resolution of hemorrhage and edema with improvement in vision.
Intravitreal Triamcinolone
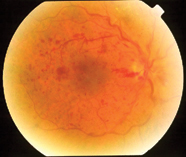
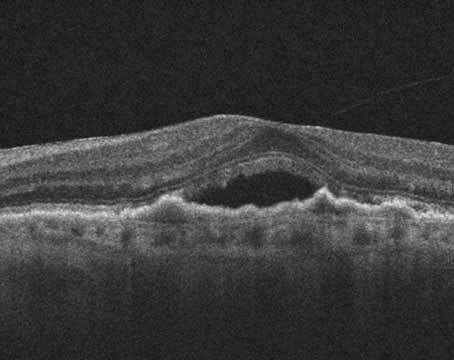
Figure 2. Preoperative photo of a central retinal vein occlusion.
Over the last few years, considerable experience has been gained in the treatment of diabetic macular edema with intravitreal triamcinolone. This procedure may be easily performed in the office setting. Given that triamcinolone seems to help reduce diabetic macular edema, we have given patients with BRVO intravitreal steroid injections. In several of our patients who still had considerable macular edema and vision loss despite extensive focal argon laser photocoagulation, there has been marked reduction in edema and modest improvement in visual acuity.
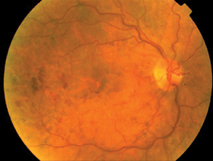 |
| Figure 3. Postoperative photo of a CRVO six weeks after radial optic neurotomy. Note the resolution of hemorrhages. There is also a collateral vessel on the nasal side of the disk, at the site of the incision. |
Both branch and central retinal vein occlusions are very common retinal vascular diseases. While laser therapy has been the mainstay of treatment for over a decade, many people still have significant visual loss as a result of these conditions. Recently, several new and exciting techniques to treat these conditions have been described, and each may have a specific role to play.
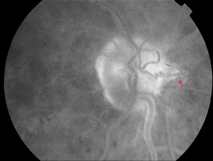 |
| Figure 4. Postoperative fluorescein angiogram at the same visit as figure 3. Note the collateral vessel and the minimal damage to the optic disk and retina (arrow). |
Dr. Garg is a fellow and Dr. Vander, an attending surgeon, in the Retina Service at Wills Eye Hospital. Contact them at (215) 928-3300 or sunirgarg@yahoo.com and jamvan@ umich.edu.
1. Branch Vein Occlusion Study Group. Argon laser photocoagulation for macular edema in branch vein occlusion. Am J Ophthalmol 1984;98:271-282.
2. The Central Retinal Vein Occlusion Study Group. Evaluation of grid pattern photocoagulation for macular edema in central retinal vein occlusion: The Central Vein Occlusion Study Group M Report. Ophthalmology 1995;102:1425-33.
3. Weinberg D, Dodwell DG, Fern SA. Anatomy of arteriovenous crossing in branch retinal vein occlusion. Am J Ophthalmol 1990;109:298-302.
4. Zhao J, Sastry SM, Sperduto RD, et al. Arteriovenous crossing patterns in branch retinal vein occlusion. Ophthalmology 1993;100:423-428.
5. Kumar B, Yu D, Morgan WH, et al. The distribution of angioarchitectural changes within the vicinity of arteriovenous crossing in branch retinal vein occlusion. Ophthalmology 1998;105:424-427.
6. Opremcak EM, Bruce RA. Surgical decompression of branch retinal vein occlusion via arteriovenous crossing sheathotomy. Retina 1999;19(1):1-5.
7. Shah GK, Sharma S, Fineman M, et al. Arteriovenous sheathotomy for the treatment of macular edema associated with branch retinal vein occlusion. Am J Ophthalmol 2000;129:104-106.
8. McAllister IL, Constable IJ. Laser-induced chorioretinal venous anastomosis for treatment of nonischemic central retinal vein occlusion. Arch Ophthalmol 1995;113:456-462.
9. Fermat S, Goldberg MF, Finkelstein D. Laser-induced chorioretinal anastomosis for nonischemic central or branch retinal vein occlusion. Arch Ophthalmol 1998;116:43-52.
10. Browning DJ, Antsy AN. Laser chorioretinal anastomosis for nonischemic central retinal vein occlusion. Ophthalmology 1998;105:670-679.
11. Weiss JN, Bynoe LA. Injection of tissue plasminogen activator into a branch retinal vein in eyes with central retinal vein occlusion. Ophthalmology 2001;108:2249-2257.
12. Hare SS. t-PA in CRVO (letter). Ophthalmology 2002;109:1758-1761.
13. Opremcak EM, Bruce RA, Romeo MD, et al. Radial optic neurotomy for central retinal vein occlusion. Retina 2001;21:408-415.
14. Ip MS, Kumar KS. Intravitreous triamcinolone acetonide as treatment for macular edema from central retinal vein occlusion. Arch Ophthalmol 2002;120:1217-1219.