The introduction of the Light-Adjustable Lens (RxSight) and its customizable technology have generated excitement in the cataract-refractive space. Not only can patients who may have been previously ineligible for anything other than a standard monofocal have an opportunity to achieve excellent vision, but surgeons also have the chance to hit their refractive targets more closely in challenging cases.
Implementing the LAL does take some additional legwork, however, as postop adjustment and lock-in appointments affect clinic workflow. For tips on how to negotiate patient selection, counseling and scheduling, we spoke with seasoned cataract/refractive surgeons who are familiar with the nuts and bolts of this technology. Here, we share their feedback.
Patient Education and Selection
Conversations with patients seeking cataract surgery usually begin with education about the various IOL options. And when it comes to the LAL, patient counseling is just as important as any other lens.
“Patients often don’t know what to expect from any lens implant,” says John Hovanesian, MD, who’s a surgeon practicing in Laguna Hills, California. “Even those who have researched the options may have encountered misleading information that doesn’t apply to their specific situation. Therefore, it’s essential for the surgeon to educate them thoroughly.”
Sumitra Khandelwal, MD, who’s a professor of ophthalmology at Baylor College of Medicine in Houston, begins by outlining the various lens options available, including monofocal lenses, astigmatism-correcting lenses, and presbyopia-correcting lenses, which come in multiple categories. “If a patient is concerned about issues such as glare and halos associated with some presbyopia-correcting lenses, I explain that the LAL provides an alternative,” she says. “The LAL functions similarly to a monofocal lens but has the added benefit of being adjustable after implantation. This adjustment capability allows us to fine-tune the lens to provide distance, intermediate, and potentially near vision based on the patient’s needs and preferences.”
 |
|
Adjustments for the Light-Adjustable Lens are scheduled approximately three weeks after the second eye for post-myopic LASIK or virgin eyes, whereas post-hyperopic or post-RK patients begin adjustments at least six weeks after their second eye to ensure the cornea has stabilized, recommends Neda Shamie, MD. |
An analogy can be effective in this situation, explains Neda Shamie, MD, of the Maloney-Shamie Vision Institute in Los Angeles. “An analogy helps patients and my team understand the technology more easily,” she says. “Essentially, it’s a lens made from a material that can be adjusted after implantation, allowing patients to ‘test drive’ their vision. I use the analogy of a designer dress or suit that you would then tailor to fit your exact size or waistline. Similarly, the LAL allows for customization of vision to the exact measurements of the patient’s eyes and can allow for test driving blended or monovision before making a commitment. This analogy helps patients grasp the concept of how the LAL can be fine-tuned to their individual needs.”
Some patients are better suited to the LAL than others and surgeons should make sure to explain why that is.
“For patients who have undergone previous refractive surgery or have unusual eye characteristics, such as flat corneas or shallow anterior chambers, I emphasize that our standard formulas for calculating IOL power may not be as accurate,” Dr. Khandelwal says. “This can lead to refractive surprises. I explain that because their eyes are atypical, the ability to achieve perfect distance vision might be limited compared to other patients. Therefore, if precise focal points are crucial and the patient wishes to avoid glasses for various distances, the LAL could be a suitable option. I stress that the LAL allows for post-implant adjustments, which can be particularly beneficial for these complex cases.”
While it has some advantages over non-adjustable IOLs, be mindful to manage expectations for the LAL carefully, advise surgeons. “The LAL’s performance can depend on two key variables: whether you’re using the LAL+ and whether you’re planning for monovision or mini monovision,” Dr. Hovanesian says. “The LAL+ is designed to provide a greater range of vision, functioning similarly to an extended depth of focus lens by modifying spherical aberration. This lens adds negative asphericity, which can increase the depth of focus for many patients. However, exercise caution when using this lens for patients who’ve undergone hyperopic LASIK or have significant corneal aberrations, as it induces some aberration that isn’t typically present in spherical lenses.”
“Patients who have undergone RK can also be very challenging because their vision fluctuates,” Dr. Khandelwal says. “I advise them that achieving stable vision may take longer and involve more frequent adjustments. I make sure to address these challenges upfront so patients are prepared for a potentially longer and more involved process, and they’re typically understanding. If they mention it’s hard for their doctor to get an accurate glasses prescription, that’s sort of a red flag to ask a few follow-up questions. Is it because they’re tough to be refracted, is it the cataract? It might be someone who isn’t going to be easy to do adjustments on, so you want to have your radar up.”
Tolerance of monovision is an important component of patient criteria. “Many patients may not have ever tried monovision before and may be hesitant about the ability to tolerate the anisometropia,” says Dr. Shamie. “A typical LAL candidate in our practice is one who is motivated to have spectacle independence but is concerned about the aberrations related to multifocal lenses or may have eyes that aren’t ideal for multifocal implants. They may be a patient who has specifically high visual expectations, or has had corneal-based refractive surgery such as LASIK, PRK or RK. The LAL’s advanced technology provides a solution tailored to their needs.”
For those who have experienced monovision, whether naturally or with contact lenses, the LAL would be a good fit, continues Dr. Shamie. “Even if they’ve never had LASIK, PRK or RK, but they’ve done well with monovision, those patients also understand what it means to optimize the distance vision and have their near at that sweet spot,” she says. “In fact, the LAL+ especially is an ideal option because it gives a bit of range of vision with the ability to fine tune it further and to create a blended zone of vision.”
Be cognizant of a patient’s ocular comorbidities as well, cautions Dr. Shamie. “Initially, we were more aggressive in recommending the LAL for patients with comorbidities such as macular degeneration who wouldn’t otherwise be candidates for premium lenses, but we learned that this may not always be the best approach,” she says. “The LAL behaves similarly to a monofocal or monofocal toric lens in terms of optical quality, so there are no added visual aberrations as one sees with diffractive multifocal lenses. The reason to hesitate recommending the LAL to patients with visually significant comorbidities such as AMD is mostly to avoid an unhappy outcome when a patient has invested time and money in this advanced lens technology and may have related unrealistic expectations of the visual potential of the eye.
“I’m fully transparent with such patients about my hesitation and paint a realistic picture of what they would achieve to help them understand why the LAL may not be the ideal IOL for them,” continues Dr. Shamie. “The time and cost commitment might not be justified if the patient’s best possible vision is limited.”
Another element to keep in mind is the patient’s astigmatism. “The LAL only corrects for regular astigmatism up to 2 to 3 D; it doesn’t correct irregular astigmatism,” says Dr. Shamie. “The lens isn’t a good option for patients with highly aberrated corneas, such as keratoconus. It’s a great lens to correct regular astigmatism up to 3 D but in its virgin state upon implantation, it’s essentially a monofocal IOL needing light adjustments to correct the refractive astigmatism. Therefore, it’s important for the patient to understand that right after the surgery their vision isn’t going to be optimized due to the remaining astigmatism up until the point that they start getting light treatments. They may need a temporary pair of glasses for some activities.”
For some patients, the commitment on their end may turn them off, while for others, it can be a rewarding experience.
“I’d put the LAL in everybody, but it requires a few things from the patient, including time, patience and a financial investment,” explains Dr. Khandelwal. “Patients need to be aware that achieving optimal results with the LAL involves multiple follow-up visits and may take several months to finalize. This is a contrast to presbyopia-correcting lenses, which generally offer a more straightforward outcome with a quicker recovery period. I make it clear that if a patient isn’t willing to commit to the necessary time and follow-up appointments, the LAL might not be the right choice for them.
“When you explain that it could potentially take two to three months for the final lock-in, if not longer for those with RK, there are patients who will decline,” she continues. “At that point I direct the conversation to a different lens platform. On the other hand, we’ll have patients who go home and read about the LAL and understand the fact that it can be optimized after surgery and it realigns their priorities. They realize this is an investment in the eyes that will last their lifetime and they’re willing to put some other things on hold to make it happen.”
Understanding patient psychology is crucial in determining who would benefit most from the LAL, according to Dr. Shamie. “It’s essential to match the technology to patients who will appreciate the detailed adjustments and fine-tuning,” she says. “Those who have enjoyed excellent vision with past refractive surgeries or are highly discerning about their vision are typically the best candidates for the LAL. On the other hand, patients who are less discerning about their visual needs may not find the LAL necessary and would push back on the time commitment.”
Those who do commit to the requirements associated with the LAL are treated like partners in the process. “We routinely observe higher satisfaction levels with the LAL compared to other lenses,” says Dr. Hovanesian. “This is largely due to the favorable refractive outcomes and the fact that patients are actively involved in the process. They understand from the beginning that they’ll need to wear glasses for a while and invest time into achieving a long-term outcome. They appreciate the ‘lock-in’ process and feel satisfied because they see their results evolve. This creates a sense of accomplishment, similar to preparing for a sports competition, where the effort put in leads to great results. By the end of the treatment, we celebrate with our patients, referring to them as graduates of the process.”
Preop Planning and Surgery
The screening process for the LAL is similar to that of any premium lens, according to surgeons, who note there are some important elements not to overlook.
“In terms of preoperative diagnostics, the LAL requires careful assessment to ensure that it’s the right choice for the patient,” Dr. Shamie says. “This includes using advanced diagnostic tools such as macular OCT to check for any underlying conditions like epiretinal membranes or drusen that could affect vision quality. We also perform topography and tomography to assess the corneal contour and identify any potential limitations due to comorbidities before proceeding with the implantation.”
Dr. Hovanesian says signs of dry eye should be managed effectively before surgery.
That therapy will likely have to continue after cataract removal. “I used to think the LAL was going to be the lens implant for patients who couldn’t have a multifocal or an EDOF because of their dry eye, but these patients are so hard to refract,” Dr. Khandelwal says. “If they have ocular surface disease, they can swing like a pendulum. Not only will you need to optimize them ahead of time, you’ll need to make sure they’re optimized afterwards. Otherwise, it’s tough to lock them in because their cylinder is changing so much.”
Dr. Shamie says the LAL requires a pupil dilated to at least 6 mm to allow for effective light adjustments. “If a patient has conditions such as pseudoexfoliation or is on medications that affect pupil dilation, this could limit the ability to perform necessary adjustments,” she says.
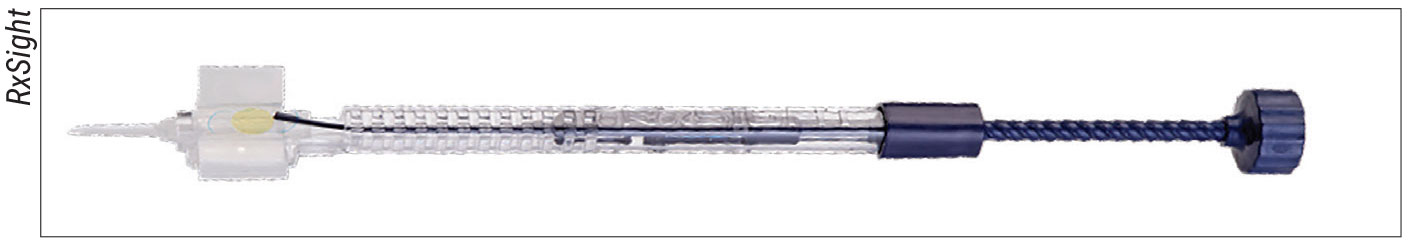
Intraoperatively, surgeons recommend expanding the traditional cataract incision to 2.8 mm to accommodate the LAL injector.
“The surgical procedure for the LAL is very similar to that of traditional silicone lenses,” Dr. Hovanesian says. “It’s a three-piece lens, so for surgeons who have only trained with single-piece acrylic lenses, there are some differences. The lens loads differently and requires skill and experience during loading. It’s crucial to handle the posterior side of the lens carefully, as it has a fragile ultraviolet-absorbing coating that can be damaged with significant manipulation. When implanted, the lens opens more quickly than an acrylic lens, so surgeons need to be prepared for that.”
“In our practice, we have our scrub techs handle the loading because they’re used to loading them all day long for different surgeons,” adds Dr. Khandelwal. “If your surgical center doesn’t have experienced scrub techs, it’s advisable for you to load the lens yourself to avoid scratching the optic. Scratching the optic would necessitate removing and replacing the lens. As surgeons, we’re okay with the leading haptic coming out a little awkwardly if we know it’s going to happen, but we don’t want it to be scratched.”
Dr. Shamie advises that the capsule be fully expanded with viscoelastic during implantation. “The slightly rapid nature of how the LAL unfolds could catch on the capsule if the eye is soft, so it’s important to make sure there’s enough viscoelastic in the eye,” she says. “There’s a technique of rotating your hand first to the left and then to the right to make sure the haptic opens in a more planar fashion. Going slow is beneficial. While the unfolding process is quicker than with a one-piece lens, it can be learned with practice. Using an artificial anterior chamber to practice lens implantation can be helpful.”
When determining a target for the LAL, Dr. Shamie suggests a slightly hyperopic outcome initially and adjusting towards myopic. “This approach provides an extended depth of focus and gives patients a sense of ongoing improvement,” she says. “For patients who have tried monovision before, and that’s what you’re targeting, I tend to pull back on the near correction. If their monovision was a -2.5 D for example in their near eye, I don’t go straight to targeting -2.25 D. I start off at maybe 0.75 D less myopic correction in the near eye, because, again, when you adjust towards the near they tend to have some extended range of focus which could mean less anisometropia but still excellent range of vision.”
“From my extensive experience, I’ve found that many patients achieve 20/20 distance vision and often get to J2 or even J1 for near vision,” Dr. Hovanesian says. “When combined with a small amount of myopia in the non-dominant eye, say 0.25 or 0.5 D, you often get a full range of vision with minimal compromise on distance vision. It’s a very satisfying option, although it’s not suitable for every patient.”
Managing Appointments and Treatments
While the LAL technology opens up the possibilities for a host of patients to reach their vision potential, there are some scheduling and logistical hurdles to overcome within the clinic.
Introducing this lens to your staff should be gradual, and everyone should expect adjustments to be made as it’s rolled out to more patients, surgeons tell us.
“Implementing significant changes in workflow begins with bringing everyone together in the practice to explain why we’re adopting this new process,” explains Dr. Hovanesian. “It’s crucial to get everyone on board, as they’re more willing to work through the steps when they understand the rationale. Many practices overlook this essential step, assuming that everyone will simply fall in line with new procedures. We approach this very deliberately.”
The scheduling and management of postoperative visits for patients with the LAL has the potential to be quite intricate and differs from the typical postop cataract visits. “Initially, I’d schedule a standard follow-up plan: a day one visit, possibly with a co-managing optometrist, followed by a visit with me three to four weeks later,” Dr. Khandelwal says. “However, with the LAL, we’ve adjusted this approach to optimize outcomes.
“The LAL really works better if you schedule the second eye surgery one week after the first eye to align with the LAL’s requirement for simultaneous adjustments,” she continues. “This approach ensures that both eyes are treated together. You don’t want to stagger them. After the initial surgery, we schedule follow-up visits for light treatments one week apart.”
For patients with a history of hyperopic LASIK or RK, the adjustment schedule will differ. “For post-myopic LASIK or virgin eyes, we recommend the first adjustment about three weeks after the second eye is done, with subsequent adjustments and lock-ins spaced one week apart, usually completed within eight weeks after surgery,” Dr. Shamie says. “In contrast, for post-hyperopic or post-RK patients, we start the first adjustment at least six weeks after their second eye, with adjustments spaced two weeks apart. This longer schedule helps ensure that the cornea has stabilized before making further adjustments.”
Dr. Hovanesian says there’s no denying that the adjustment process is somewhat time-consuming, but it’s discussed from the outset. “There can be as many as five visits for light treatments, with two of those being lock-ins,” he says. “Each visit includes careful refractions, counseling, dilation and treatment, along with any waiting time. Therefore, each adjustment visit usually takes at least 45 minutes to an hour, often longer.”
The adjustment itself is relatively quick, taking about 10 minutes, says Dr. Khandelwal. “However, the entire visit usually lasts about an hour and a half. Patients undergo a refraction with our optometrist, followed by dilation. If the goal is to achieve distance vision only, the process takes about an hour, but if the patient seeks additional near vision, we might conduct a monovision trial and have them walk around to gauge their vision. This extra step can extend the duration of the visit,” she says.
Considering the scheduling challenges associated with the LAL, practitioners using the lens have adopted their own modus operandi that suits their particular clinic. Some surgeons choose to perform the adjustments and lock-ins themselves, and others rely on the skills of an optometrist (whether internal or external) to see the patient through these appointments.
“In our practice, managing patients with the Light-Adjustable Lens involves a dedicated team approach,” Dr. Khandelwal says. “Initially, when we started using the LAL, we had several technicians help with refractions and trained them to assist with the treatments. However, we have since found it beneficial to have one or two primary staff members responsible for performing refractions and conducting monovision trials and patient counseling during each visit. In our office, we have an optometrist who does this for multiple surgeons. This setup allows for a collective experience.”
Dr. Khandelwal prefers to personally handle her patients’ adjustments of the LAL. “Although some practices may have optometrists or even retired ophthalmologists perform these final adjustments, we find that having our optometrists involved in the refraction and counseling process, while I handle the adjustments, works effectively,” she says. “This arrangement works well because the refraction, the monovision trials, and counseling all fall within the optometrist skillset. Then I come in and verify everything with the patient before doing the treatment with the optometrist by my side. It doesn’t take me out of the clinic for very long.”
She adds that each surgeon at her center has designated days for surgeries and treatments, and patients are aware of the schedule from the start to manage patient expectations.
When Dr. Shamie began working with the LAL, she initially performed light adjustments in order to gain a thorough understanding of the process before training their staff optometrists. “Now, our optometrists, who are specially trained in light adjustments, handle this aspect,” she says. “They perform initial postop light-adjustment exams, including trial frames and contact lens trials if necessary, to determine the best refractive target.”
 |
|
Surgeons say to enlarge the cataract incision to 2.8 mm to accommodate the Light-Adjustable Lens insertion device. They recommend careful loading of the lens to avoid scratching the optic. |
Dr. Hovanesian says everyone on his staff was trained for the LAL, and they developed a special process, including electronic paperwork and a patient flow protocol. “Our optometrists play an integral role in this process; they handle everything except the light treatments,” he says. “During appointments, optometrists dilate the patients and then send them to us on the same visit for light treatment, with the surgeons performing the actual light treatments. Given the number of visits required, it’s vital to have a well-organized system in place.”
In the process of making adjustments, Dr. Khandelwal says patient psychology is still in play. “For example, if I know they were a monovision patient, but they didn’t tolerate driving at nighttime with monovision contact lenses, I’m not going to push the monovision right away,” she says. “I’ll go slow with the monovision, whereas, if they were a rock star monovision patient, we can go a little bit more near on that first eye treatment. If the patient used to be a -3 and now I’ve made them distance in both eyes, I know that patient is going to want to push the envelope on the near vision. I make sure to discuss compromises with them.”
These surgeons warn others to be careful not to keep moving those visual goalposts.
“It’s important to get a clear commitment from the patient to the refractive target prior to initiating the first adjustment to avoid confusion and ensure a smooth process,” Dr. Shamie advises. “If the patient is given the impression that they can change their mind at every adjustment, it would cause a serious workflow challenge. We made that mistake in the beginning. Now, the optometrists handle subsequent adjustments, focusing on moving towards the target without revisiting the target at each visit.”
Remember that the ultimate goal is patient happiness, Dr. Hovanesian adds. “Sometimes we may feel tempted to pursue a sharper target, but it’s important to avoid pushing the goal too far, which could lead to a worse outcome,” he says.
One final word of caution from Dr. Khandelwal: Occasionally, patients may experience early posterior capsule opacification. “In such cases, we address this issue with an early YAG capsulotomy before proceeding with any adjustment treatments,” she says.
Weighing the Return on Investment
The vast array of IOL options on the market leaves some cataract surgeons wondering where the LAL fits into their everyday practice. These surgeons say it’s a worthwhile investment.
“For those considering adopting the LAL in their practice, I recommend viewing it as an opportunity to expand premium offerings rather than as a replacement for existing lens options,” says Dr. Khandelwal. “I don’t think it cannibalizes the current lenses out there.”
More often than not, patients are seeking advanced IOL technology, but are limited by their own pathology. “Having the LAL expands the offerings to those patients who would otherwise have gotten standard lenses,” Dr. Shamie says. “There are patients in every practice who desire freedom from glasses or want customized vision, but for one reason or another, they’re not a great candidate for the other presbyopia-correcting lenses. Unfortunately, if the surgeon doesn’t have access to the LAL, this patient can only fall back onto a standard lens when they may have been willing—more than willing—to invest in optimized, advanced lens technology.”
“By offering this technology, you may find that it can be used for more patients than you initially thought, extending beyond just post-refractive patients,” Dr. Hovanesian concludes. “It allows for greater patient control over their outcomes.
Dr. Hovanesian discloses stock in RxSight. Dr. Khandelwal reports no disclosures. Dr. Shamie is a consultant for RxSight.



