|
| The effects of post-femto LASIK rainbow glare, simulated here using a treated PMMA disk, can be frightening to patients. (All images courtesy Damien Gatinel, MD.) |
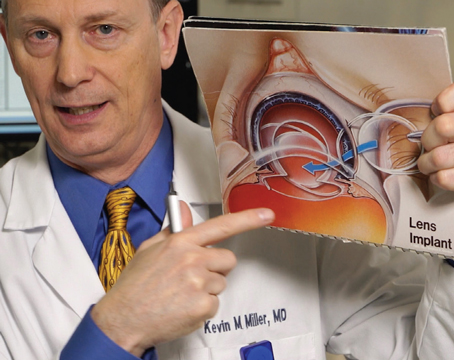
The Face of the Problem
When Damien Gatinel, MD, of Paris, France, encountered his first case of post-LASIK rainbow glare, the patient was in dire straits. “He had already spent two weeks in a psychiatric hospital because he was complaining about color fringes,” Dr. Gatinel recalls. “No one took him seriously because the complication wasn’t very well-known at that time. He was telling his doctors that the problems started after his refractive surgery, and when he was asked to draw what he saw—or was pretending to see—what he drew was quite scary: Bizarre bands of colors. When I finally saw him, I’ll never forget what he told me: ‘Dr. Gatinel,’ he said, ‘I’m looking at you, and if you were a bright light I would also see another you in colors 50 cm to your left, another you 50 cm to your right, and a ghost head floating above yours.’ He was quite serious, and was so concerned about his vision that he could no longer drive, and what was particularly disturbing for him was the ghosting effect. He told me that when he would walk at night and would look at the pedestrian walk signals at intersections, he’d see duplicates of the signals floating in the air on all sides of the light. This is because such lights are monochromatic, as opposed to a white light that will produce a spectrum when it’s viewed by someone with this complication. Fortunately, his case resolved within six months, and we now know that some cases resolve spontaneously.”
Studying Rainbow Glare
Rainbow glare after LASIK was first described in a retrospective study from the Cleveland Clinic’s Cole Eye Institute in 2008.
In the study, investigators reviewed 215 patients (399 eyes) who had been treated using an older model IntraLase laser and 97 patients (186 eyes) who had been treated with a newer model. They found that 37 (19 percent) of the older-laser patients whom they had been able to contact had rainbow glare. However, in the new-laser patients whom they were able to contact, only two patients (2 percent) reported rainbow glare.1 These findings seem to jibe with current surgeons’ experience that newer femtosecond technology has greatly reduced, but not eliminated, rainbow glare as a complication.
To get an idea of what was behind rainbow glare, Dr. Gatinel placed a PMMA disk beneath his FS200 femtosecond laser and programmed a regular flap cut that placed the laser’s raster pattern inside the plastic. When he went outside and looked at light sources through the disk, he was able to replicate patients’ rainbow-glare complaints, right down to the duplicate images surrounding pedestrian walk signals. He says the glare is the result of a diffractive process that, ironically, stems from the perfect regularity of the spacing of the treatment. “The glare arises from a diffractive effect caused by the regularity of the pattern,” he says. “If the femtosecond were randomly shooting the spots and they weren’t evenly spaced, you wouldn’t have much diffraction of light and rainbow glare because the diffracted light rays would cancel each other out. Rainbow glare is the price you pay for a very regular spot delivery.”
Erasing the Rainbow
After another patient was referred to Dr. Gatinel with rainbow glare, he began to devise a strategy for treating it.
“At that time, I knew that the cause of the rainbow glare was probably the posterior surface of the flap,” he says. “The mechanism is quite straightforward: Because the femtosecond laser’s raster pattern imprints some spots in the stroma and the posterior surface of the flap, when you perform the LASIK ablation the excimer erases the raster pattern from the stromal bed but not from the posterior flap surface. I began thinking of doing some treatment on the back surface of the flap.”
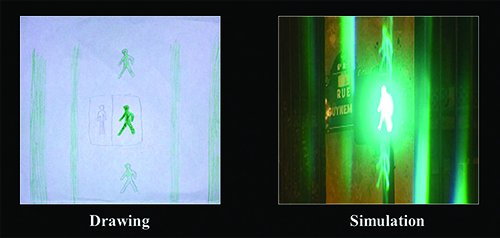 |
| When Paris surgeon Damien Gatinel used a femtosecond laser to simulate a flap cut on a PMMA disk, and then held the disk up to the light, he was able to reproduce the images patients had drawn to illustrate their rainbow glare complaints after femto LASIK. |
For a surgeon who’d like to treat a patient with rainbow-glare complaints, Dr. Gatinel offers some tips. “If the patient also has a refractive error, you can kill two birds with one stone by a treatment on the back surface of the flap to improve vision and erase the raster pattern,” he says. “But, for an emmetropic patient, you can do a 10- to 15-µm PTK instead. To place a treatment on the back surface of the flap though, you have to deactivate the excimer’s eye tracker because it looks for the center of the pupil, which will not be there because the flap will be reflected back. So, before you reflect the flap back, be sure to mark the center of the pupil with an ink dot so you can center the treatment on that. Also, if you’re treating astigmatism, you have to reverse the astigmatism axis of your treatment because, when you lift the flap, the astigmatism is a mirror image of what it is normally. The formula for the treatment axis, then, is 180 degrees minus the astigmatic axis from your measurements.
“In terms of treatment limits, if the flap is thin you need to be cautious,” Dr. Gatinel adds. “For a 110-µm flap, for example, if the epithelium is 50 µm, you’re left with about 50 or 60 µm of stroma. That’s probably not enough to treat more than 20 or 30 µm. Thirty µm is around a 2-D correction with a 6-mm zone. I don’t think hyperopia is a good indication because in a hyperopic correction you don’t remove the stroma in the center, but the goal of the rainbow-glare treatment is to remove the depth of the femtosecond spots, which is about 10 µm. This means a hyperopic treatment that doesn’t treat the center might not be that effective. What you could do, however, is put a non-refractive PTK treatment on the back surface of the flap to treat the glare and then do a hyperopic treatment on the stromal surface.”
Dr. Gatinel thinks that, even if a rainbow-glare treatment doesn’t eliminate the problem, just reducing it can be enough for many. “After the rainbow-glare surgery that minimized my second patient’s symptoms,” he recalls, “the patient looked into the light of a smartphone and burst into tears of relief, saying, ‘I’ve been brought back to life.’ ” REVIEW
1. Krueger RR, Thornton IL, Xu M, Bor Z, et al. Rainbow glare as an optical side effect of IntraLASIK. Ophthalmology 2008;115:7:1187-1195.