Review of Cornea & External Disease In this Issue... Artificial Intelligence for the Cornea Specialist by Christine Yue Leonard DSO and Cultured Endothelial Cell Transplants: A Review by Thomas John, MD, and Anny M.S. Cheng, MD Premium IOLs in Patients with Corneal Conditions by Asim Piracha, MD Diagnosis & Management of Blepharitis by Charles Bouchard, MD, MA |
If you decide to venture into the world of premium surgery or are looking for ways to improve how you’re already offering these services, cataract surgeons say it’s important to be committed in order to do it right. Incorporating premium services requires a degree of business know-how and some logistical changes, including technology investment, scheduling and clinic flow alterations, and providing additional education for both patients and staff.
“You need to believe you’re actually giving the patient something that can benefit them and improve their life, because if you don’t believe in the technology yourself, it’s hard to present these options to qualified patients,” says Kendall Donaldson, MD, of Bascom Palmer Eye Institute in Miami.
In this article, cataract surgeons discuss their approaches to premium services and how to shape a practice that supports patient happiness at every step.
Avoid the Sales Pitch
“The original challenge was finding the perfect candidate for some of the first- or second-generation presbyopia-correcting lenses. Now, the challenge is tailoring the discussion to the patient so they can decide which of the appropriate lens implants is best for them,” says Sumitra Khandelwal, MD, of Baylor College of Medicine in Houston. “It’s important to let the patient know all of their options.”
When having this discussion, experts say to avoid sounding as if you’re giving a sales pitch. “Sales-pitch-style discussions offend many patients,” says Dr. Donaldson. “Be honest about what the technology can offer the patient and discuss the limitations as well as the benefits.”
Kevin M. Miller, MD, of the Stein Eye Institute at the University of California Los Angeles, says there’s an overemphasis on the IOL in the world of premium surgery. “The word ‘premium’ implies that a standard lens is somehow subpar, which of course, it’s not,” he says. “We call premium IOLs ‘specialty’ lenses in our practice because they fit specialty needs. They’re not for everybody.
“The emphasis should be on doing what’s in the best interests of the patient,” he continues. “Each patient who comes through our office door can be approached as a premium patient because we can achieve premium results by managing astigmatism even if we’ll be implanting a monofocal lens. In the end, what determines how well a person sees is the health of the eye and their refractive state.
“Much of your discussion should revolve around pathologies in the eye, the patient’s lifestyle, and their wants and their needs,” Dr. Miller points out. “There are some patients who are quite content wearing reading glasses and trying to upsell them on a multifocal lens may be the wrong thing for them.”
Many practices separate the lens and money discussions. After Dr. Khandelwal gives her lens recommendations to the patient, the patient speaks with the practice’s surgical coordinator to review the costs for the lenses the patient is a candidate for. “Then, during the preop visit, we sit down and confirm the lens implant, and I answer any questions,” Dr. Khandelwal says. “I always tell my patients, ‘It’s your decision, and it’s okay if you pick a standard lens covered by insurance. You’ll still see better than you do now.’ That way they don’t feel pressured into anything by their surgeon.”
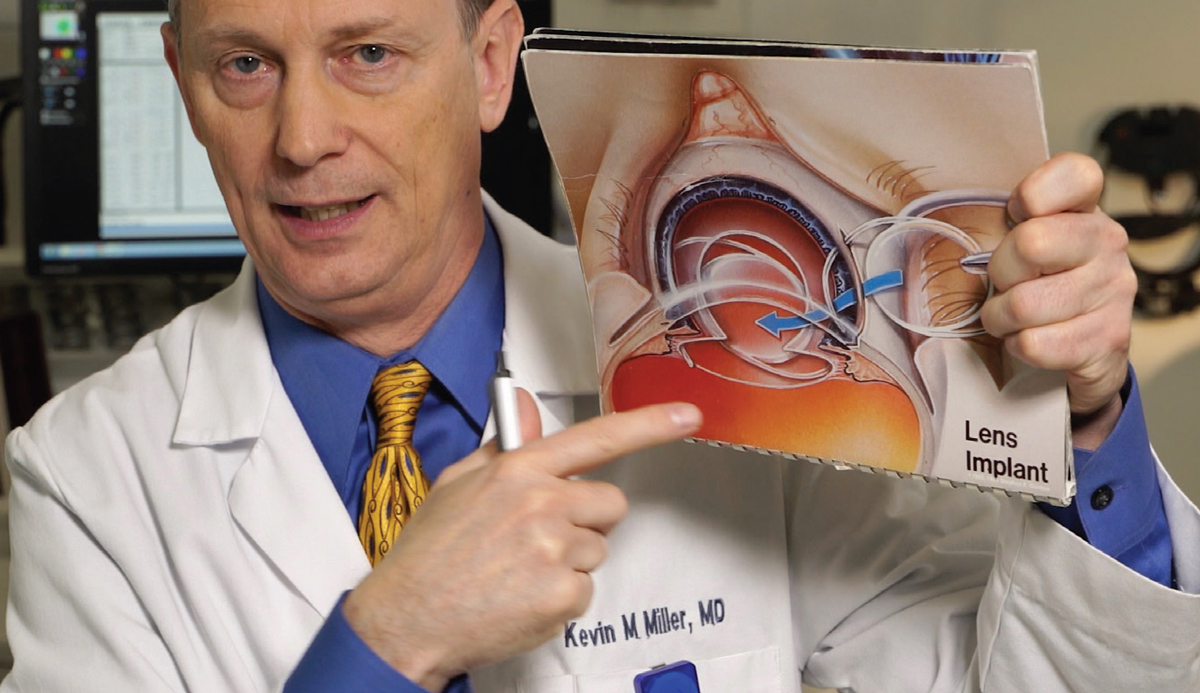 |
| All potential cataract surgery patients at Kevin M. Miller, MD’s practice at the Stein Eye Institute at the University of California, Los Angeles, watch a 40-minute educational video to learn about the eye, cataracts, cataract surgery, lens options, complications and what to expect. Educational videos for patients are one way to standardize what’s said to the patient, and the video can be documented in the patient’s chart. Photo: Kevin M. Miller, MD. |
Additional Chair Time
Premium lens candidates generally require more chair time than patients receiving standard lenses, such as a patient whose retinal pathology limits their choice of implant. Experts say it’s important that your schedule allow for that additional time, or that you have a dedicated staff member such as a surgical coordinator who can spend time with patients, so they can make the best choices for themselves. “Sometimes this requires logistical changes in the way we schedule patients,” Dr. Donaldson notes.
You may be able to streamline some of this process with supplemental material and by educating patients before they come into the office. “Our website has patient information on cataract surgery and lens options, and even just identifying a patient as a cataract consultation allows us to send them information electronically,” Dr. Donaldson says. “Having these educational materials available for the patient before they come see us increases our efficiency.”
Dr. Khandelwal points out that if you don’t have educational material ahead of time for the patient, give it to your patient the day they’re evaluated in the clinic and let them go home to read it and then follow up with somebody, such as the surgeon, optometrist or surgical coordinator.
Keeping your recommended options simple is often most helpful for the patient, experts say. “We weed out patients who wouldn’t be appropriate for certain lenses and limit their options because we know they might have more glare or halos—though we can’t really determine how much they’ll notice those,” Dr. Donaldson says.
“I give my patients a handout that has everything I discussed with them,” Dr. Khandelwal says. “It includes pricing, so they have a chance to actually look at it before they talk with my surgical coordinator. Having things on paper is so important because patients get really confused, and they’re given so much information during a cataract evaluation—important dates, risk factors, lens implant information, etc.”
Dr. Khandelwal also says it’s good to have at least two different times when patients can ask questions. “This is important for practices,” she says. “If you see a patient for the first time, and they’ve never heard of the different lens options, and that’s the only time they’re going to ask their questions, it’s very hard for them to understand what they’re getting into. It’s key that they hear this information twice and get to ask questions at least twice. That could be with you, the optometrist or the surgical coordinator.”
Educational videos are another way to inform the patient, save the surgeon time and provide consistency. Dr. Donaldson and Dr. Miller both created educational videos in which they discuss cataract surgery and lens options.
“I created a nine-minute video that reviews all of the lens options for patients, so I don’t have to repeat that to every patient throughout the day,” Dr. Donaldson says. “It’s been a great time investment. When they’re in the exam room waiting for me, they’re given an iPad to watch the video. (It’s also available on our website.) They can watch it while they’re waiting for me and while they’re dilating, and it goes through all their choices. It’s very helpful and has made my practice more efficient.”
She says you can also document in the patient’s chart that they saw the video. “You know exactly what’s been told to the patient, as far as benefits, limitations and technology, and that the patient’s specific lens options will be reviewed with the physician. Then, I can walk in and say, ‘Oh, now you’re a bit familiar with it, and we can go over in more detail what would be most appropriate for you.’ They usually have some questions lined up after the video.”
Patients coming for their preoperative evaluation view Dr. Miller’s video during their encounter. He says that during the 40-minute video, he discusses the nature of cataracts, cataract surgery, astigmatism management, femtosecond laser use, intraoperative refractive guidance systems, postoperative refractive enhancement, risks and complications.
 |
| The Atrium at Vance Thompson Vision in Sioux Falls, South Dakota. Customer service is important in any practice, but it’s especially key when patients are paying so much out of pocket. When patients enter the clinic, they’re greeted by the First Impressions team. After the front desk collects patient information, the team enters a description of what the patient is wearing and where they’re sitting so the technician can walk right up to the patient and greet them. Dr. Thompson’s practice uses a seating chart for their Atrium similar to that of a restaurant for reference. Photo: Vance Thompson, MD. |
“They get the whole spiel, including a section for those interested in taking part in our patient-based research at the University of California’s Stein Eye Institute,” he says. “It’s a bit like taking a sip of water from a fire hydrant, but this way the concepts aren’t completely foreign when they meet with me subsequently. On the initial consultation, the one before the preoperative visit, they also receive a one-page handout that describes all our refractive services and the associated costs. We get sticker shock out of the way early. If they don’t come back, we haven’t wasted any time.”
Consistent Messaging
“Patients may not remember 90 percent of what I say or what anybody in my office says, but they’ll pick up on any discrepancies in a heartbeat,” says Dr. Miller. “You really have to make sure your messaging is consistent. Everything in our office is well-scripted. We have documents and forms to give to patients, and we’re very clear about what our services are over the phone.”
Dr. Donaldson agrees. “Patients ask a lot of questions along the way, and you want to make sure they’re receiving a consistent message from the time they walk into your office, through the exam and imaging, and sitting with the surgical coordinator,” she says. “You want one consistent message, so the patient doesn’t feel overwhelmed.
“When I finish my cataract consultation, I write a specific recommendation in my plan so that when my staff see the patient, and when we’re taking measurements, they can propagate the same message about what I’ve recommended instead of talking about all the other lenses again,” she says. “To ensure that consistency, your staff need to be well-educated too, and also buy into the technology.”
Dr. Khandelwal says her practice hosts lunch-and-learns for the staff whenever a new technology comes out. “Our technicians are really excited about new lens implants,” she says. “They really notice how happy the patients are after these procedures.”
Dr. Miller’s practice has monthly staff meetings. He says they frequently perform walk-throughs from the patient’s point of view. “We roleplay how it looks from the patient’s perspective at each touchpoint, starting at the front desk,” he explains. “A patient might say, ‘Hey, I hear you guys use these lasers? What’s that all about?’ And the front office staff will tell me what they would say to the patient. I might say, ‘Okay, refine that answer a bit.’ We do this through the entire process, and we do it continuously because we’re constantly bringing new people on as some staff move on to other jobs.”
Dr. Miller also has his staff go to the operating room so they can see what goes on there. “Patients often ask the front office staff what surgery is like,” he says. “They can’t answer those questions if they’ve never been there themselves, so we bring them down to see everything live. I also have every staff member watch the educational video I show to patients, and at the monthly meetings we talk about patients who were a problem in the past month and go over talking points for the staff. It’s just a matter of continuous education.”
Investing in your team will pay off, doctors say. “When you look at the clinic flow, so much of the patient’s time is spent with your team,” says Vance Thompson, MD, of Vance Thompson Vision in Sioux Falls, South Dakota. “The majority of the functions in a clinic are delivered by staff. We have training classes, retreats, manuals and forms, and then we have employee-to-employee training for new employees working in the same job.”
Simple Pricing Structures
Physicians agree that a simple pricing structure usually works best for a practice and its patients, but every practice is unique. “Having a global fee has worked the best for us,” says Dr. Thompson. “We used to not include the enhancement and the patient would simply pay extra, but that didn’t go over well.”
Two commonly used models are an à la carte system or a package. “With à la carte pricing, the practice usually charges the patient for the surgeon fee and a lens,” Dr. Khandelwal explains. “There are several things to factor into this model though. For one thing, premium lenses cost more money than standard lenses, so the cost of the lens must be included in your pricing. Your time is also valuable—these patients expect a certain outcome and you may have to see them more often. Some of these premium lenses may make small things, such as ocular surface disease or posterior capsule opacity, more apparent, so it’s important to calculate how much time you’re spending on that.”
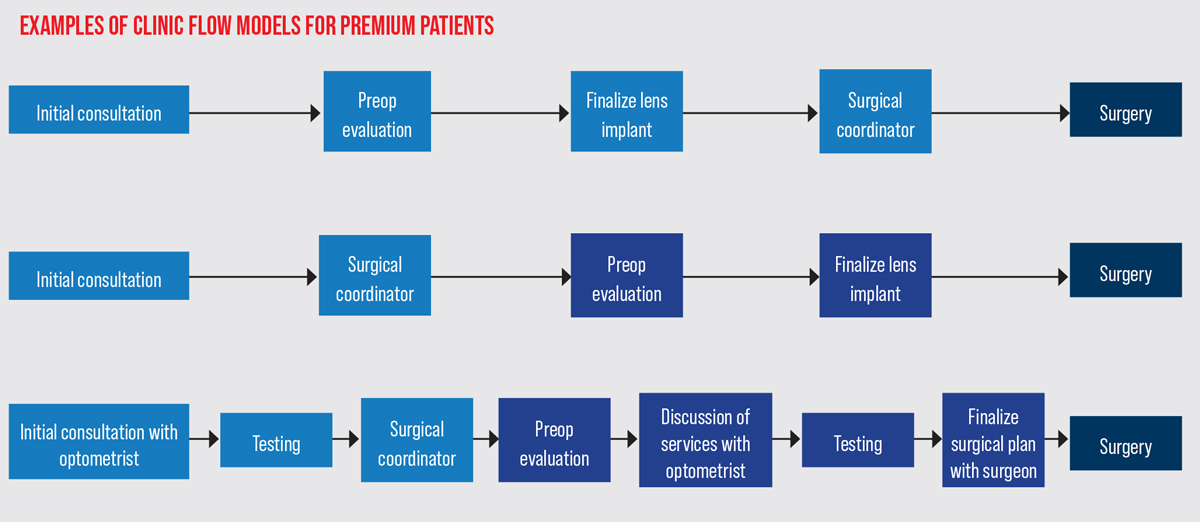 |
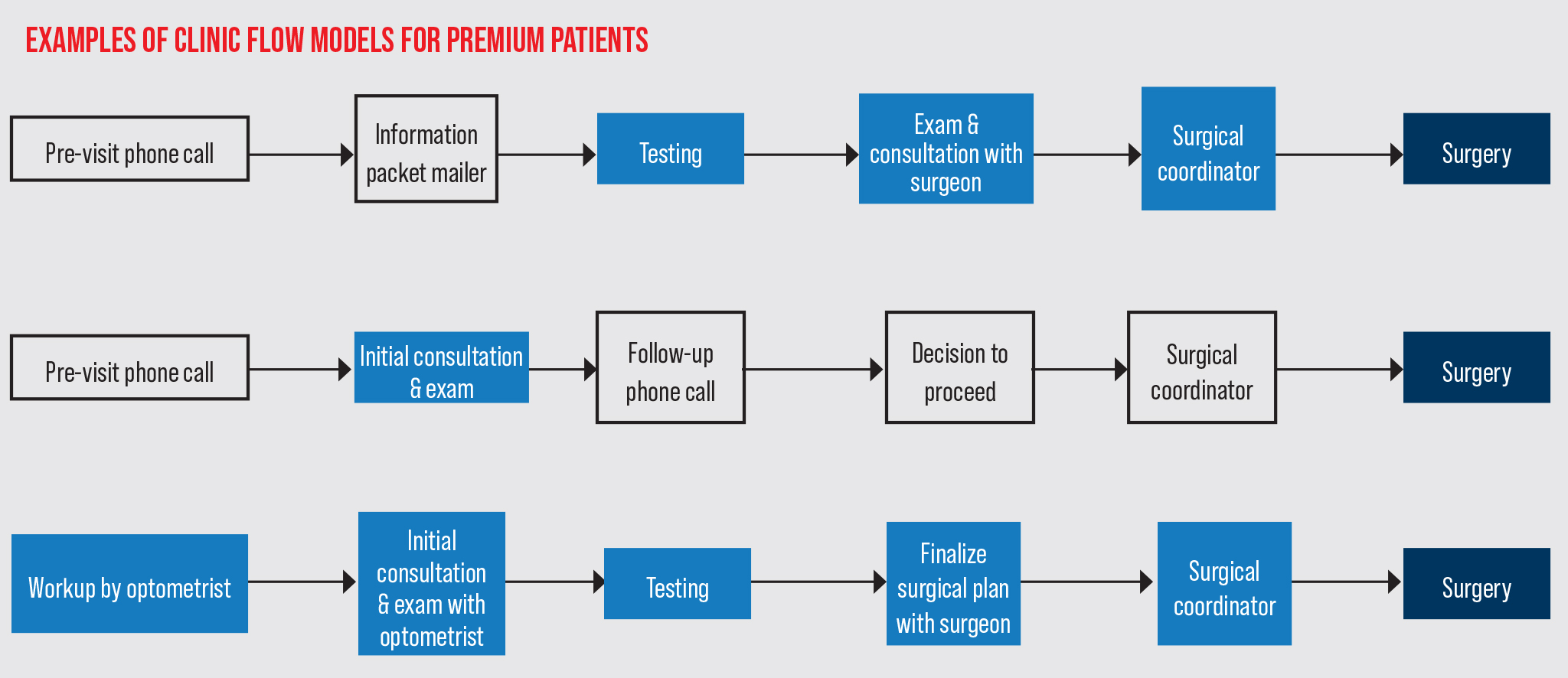
| Some practices conduct the initial consultation and preoperative evaluation as separate visits (middle, bottom), and others do it all in one day (top). (Boxes of the same color are within the same visit.) |
Dr. Khandelwal’s practice finds package pricing easier. In this model, enhancements such as refractive cataract surgery, LRIs or lens exchanges are included in the package (e.g., standard cataract surgery, astigmatism correction or presbyopia correction packages). “Pricing really depends on each practice and on the market rates,” she notes. “You can ask your colleagues about market rates, but not everyone will feel comfortable doing this.”
Dr. Khandelwal performs any enhancements herself. “I’m a cornea specialist and a LASIK surgeon, so doing LASIK or PRK is easy for me since it’s already incorporated into my practice,” she says. “We own our excimer laser and are prepared to do enhancements on our patients.
“If you’re not a corneal refractive surgeon, you have a couple of options,” she continues. “You can learn how to do basic PRK, or you can talk to a neighboring practice that owns its own laser and work out a model where they can assist you with enhancements for your patients. We often do that for our referring doctors who implant lenses but don’t have access to a refractive laser for corneal enhancements. In those cases, we discuss with them the best option for the patient’s best outcome.”
“At Bascom Palmer, we have a pretty simple pricing structure, which is key because patients can become overwhelmed,” Dr. Donaldson says. “We have our standard lens options that are covered by insurance and those outside insurance. We have two levels of upgrades. The first is astigmatism correction, where we would use distance lenses, near lenses or monovision. The second is presbyopia correction. PanOptix, Synergy, Symfony, Vivity or any of the various presbyopia-correction options are all the same price. It’s pretty simple. Any enhancements are included in the price of the upgrade for one year, so we aren’t charging for LASIK or PRK. Refractive enhancements are included and one year covers most people.”
“If appropriate patients want an EDOF or multifocal lens, they pay the hospital for the lens,” says Dr. Miller. “I don’t make any money from the sale of a specialty lens, so there’s nothing pushing me to sell lenses. It takes a lot of the financial bias away. I don’t have to figure out, for example, if I can ‘get away with’ implanting a multifocal lens into an eye with a mild epiretinal membrane. I simply don’t do it because it’s not in the patient’s best interest.”
 |
| Vance Thompson, MD, of Sioux Falls, South Dakota, is teaming up with Kathryn Hatch, MD, of the Massachusetts Eye and Ear Infirmary to host a course called Absolute Presbyopia on January 12-13, 2023, in Napa Valley, California. The course’s goal is to teach physicians and their staff about the steps of the premium IOL journey. Photo: Vance Thompson, MD. |
His practice charges patients based on services provided and the hospital charges for devices. There are four services. The first two are related to astigmatism management: one option with a diamond knife or metal blade and the other with a femtosecond laser. The third option involves the use of intraoperative refractive guidance technologies such as Callisto, Verion and ORA. “We have all three and talk to patients about which device or devices we’d like to use or that would be optimal for their particular situation. They can sign up to have a guidance device used if they want. Otherwise, we just do it the old-fashioned way. For refractive guidance, patients pay a certain amount of money to the physician, a certain amount to the hospital, and a certain amount to the lab for the extra work performed.”
The fourth service is postoperative refractive enhancement. “If patients sign up ahead of time for postoperative refractive enhancement, they get a laser refractive enhancement for 20 percent of the price they would pay if they came to us otherwise,” he says. “Most of the time, we’re not going to need to do an enhancement because the refractive results will be good. However, if there is a small refractive error in the end and the patient needs glasses for best visual acuity, signing up ahead of time for the postoperative refractive enhancement service would then have been a good idea. We’ll do a touch-up PRK or LASIK once they’re stable.”
 |
Plan for Unhappiness
“You have to have a plan for dealing with occasional unhappy patients,” Dr. Miller says. “They’ve spent a lot of money and time, and they’re unsatisfied. The first time you get an unhappy patient, it’s upsetting, and you may think that doing refractive cataract surgery is too much work. Good communication is key. Speak honestly with the patient, find out what’s keeping their vision from being satisfactory, and talk objectively about costs. You need to be able to manage the occasional patients who don’t have optimal results and work with them. I can take almost anybody who’s not happy and make them happy eventually.”
“This is why we make the phone calls,” says Dr. Thompson. “We want to ensure that patients remember what we told them preoperatively—that there can be blurry vision, that fine-tuning is often needed postop and that there’s a neural adaptation time period. We cover this in detail preop but also deliver this postop to make sure the patient is happy.”
Clinic Flow Models
There are many different clinic flow models, and they vary by practice. “Some people do the cataract evaluation and then bring the patient back for the preop while others do it all in one day,” Dr. Khandelwal explains. “In some models, the optometrist does the preop or the counseling and then surgeon meets the patient.”
“We target the cataract surgical evaluations in advance of the clinic,” says Dr. Donaldson. “When the patient is seated in the exam room waiting for the physician, they’re given an iPad with a nine-minute video explaining cataract surgery and the potential lens options. Following the cataract surgery consultation, they’re given a package of information to review and they receive a follow-up phone call within one week to review any questions and discuss whether they’re ready to proceed with surgery. They’re also given the surgical coordinator’s information at the time of their visit so that they may move forward on their own schedule, if they prefer. We’re very cautious to not ‘oversell’ and let the patient lead the process with their desires and expectations for their cataract surgery.”
Dr. Khandelwal’s practice has two models, depending on where the patient comes from. “Most patients are referred to me for cataract evaluation, and I start the discussion of lens implants that day for those without any prior knowledge,” she says. “I give them a handout and have them talk to my surgical coordinator. Then, they come back another day for the preop visit where we finalize the lens implant decision.
“The second model works well with our trusted referral sources, both optometrists and ophthalmologists, who really know the different lens implants out there and counsel patients,” she continues. “The patients come to me on the day of their evaluation, but because their referring doctor has spoken with them, and they already have an idea of which lens implant they want, it’s also their preop day. We often go with what the referring doctor said, but sometimes I change the plan. At the end of the day, the referring doctor is looking to me as a surgeon who will implant the best lens for their patient.”
Patients see an optometrist for their initial consultation at Dr. Miller’s practice. “Patients also get some labs done and, if they’re a candidate for cataract surgery, they see a surgical coordinator to schedule surgery,” he explains. “If we can fix their vision sufficiently with glasses or contact lenses, we’ll do that instead of performing surgery.
“The preoperative evaluation occurs two weeks before the surgery,” he continues. “The patient sees an optometrist, and then goes to a video room to watch an educational video. The optometrist then gives them a preliminary walkthrough of all the services offered and the patient selects or deselects services. Then, they go off for more testing relevant to the cataract operation, such as lens power calculations, corneal tomography, and a macular OCT if they’re considering a multifocal lens. They’ll sometimes come back to have the optometrist clarify things. I then answer any remaining questions when I see them and we finalize the surgical plan, which might also include a conversation about MIGS devices, capsular tension rings or a dozen other things. When I’m finished, we all sign the surgical and financial consent forms, and the next event is the surgery.”
Dr. Thompson’s private practice has a First Impressions team that collects and documents patient information during an initial phone call—including the patient’s favorite beverage and music. “We have Pandora in each of our exam rooms so we can have the patient’s favorite music playing when they enter the room,” Dr. Thompson says. Patients receive an information packet in the mail after booking their appointment. Dr. Thompson’s office also verifies the patient is in their network.
The First Impressions team greets the patient when they come in (and aren’t on the phone with other patients). “We have fresh cookies, coffee and water available for our guests,” Dr. Thompson says. “After collecting more information, the team enters a description of what the patient is wearing and where they’re sitting so the technician can walk right up to the patient and greet them. We have a seating chart of our Atrium similar to a restaurant that we reference.”
Patients undergo testing (including Epic, Lenstar, OCT, Pentacam and Tearlab osmolarity) before their exam and consultation with the doctor, where Dr. Thompson “matches the implant technology with their hopes and eyes.” The patient sees the surgical coordinator to schedule surgery, discuss postop drop options and fill out financial forms and consents. Then, they go over financial information.
“We use our Financial Information and Consent to Upgrade to Refractive Diagnostics for Refractive Cataract Surgery forms,” Dr. Thompson explains. “This clearly explains the difference between the standard charges and the refractive charges. The patient will walk out, personally escorted by the surgical coordinator, with a very good idea of what the surgery will cost them. We also have financing options to help with the cost. Once their surgery is scheduled, the counseling team sends the patients a text with a link to a video that informs them what to expect in the time leading up to their surgery.”
The team calls the patient later on to set up a postop appointment with Dr. Thompson’s practice or a local provider. They send additional videos about what to expect on the day of surgery and after (e.g., that it’s normal to have some blurry vision or for the eyes to feel scratchy), as well as a one-week postop video in addition to their exams, a surgery center experience survey and “touch-base” phone calls if they’re not being seen at Dr. Thompson’s practice.
Pearls for Newcomers
“Adding premium lenses to your practice is one of the most rewarding things you can do,” Dr. Thompson says. “There’s a high rate of satisfaction with premium IOLs—not just for patients, but for the surgeon, staff and community. Patients love that you’re presenting them with all their options and delivering what they want. Staff love the professional growth since they become specialists in their area of emphasis.”
Here are some pearls for incorporating premium lenses into your practice or improving your existing services:
• Start with toric lenses. “Someone who’s trying to get into premium lens surgery usually starts with toric lenses because they’re much more forgiving, as far as any side effects such as glare or halos,” Dr. Donaldson says. “You don’t have to manage any of the potential dysphotopsias we see with multifocal lenses.”
“There are basic things you need to learn if you’re going to perform refractive cataract surgery—making a reference mark on the limbus to compensate for recumbent torsion, marking the steep axis, aligning a toric lens in the eye, and ensuring that the lens stays aligned when you remove the viscoelastic,” says Dr. Miller, “but patients with astigmatism are generally easy to please. Even before you start with toric lenses, hone your astigmatism management skills by placing phacoemulsification incisions on the steep axis and performing peripheral corneal relaxing incisions.”
• Invest in the preoperative technology. You’ll also need to invest in preoperative technology, such as topography and tomography. “The IOLMaster 700 has been key for us because it has advanced formulas built in, including the Barrett formula,” says Dr. Donaldson. “We use it in addition to topography and tomography images, and we like them all to match.”
• Learn the business. The business side of premium lenses can be complicated. Experts say you should take the time to learn everything that’s involved. Dr. Thompson notes, “I’m offering a course with Kathryn Hatch, MD, called Absolute Presbyopia, where we teach doctors and their employee implementor every step in the premium lens journey.” The first course takes place January 12-13, 2023, in the Napa Valley.
• Choose easy first patients. “I always say to start with a lens you believe in, with the smallest side-effect profile and with a patient who has reasonable expectations,” says Dr. Khandelwal. “A patient who has a pristine cornea and a pristine retina is a good candidate. Once you do your first premium lens, you’ll gain a lot of confidence if it’s a great outcome. If you pick a difficult case the first time around, you may feel as if you don’t want to do these lenses anymore, but these are really good lenses and have great outcomes. So, choose a patient who’s an ideal candidate and don’t try to stretch into any gray zones.”
• Follow your results. “Creating a personal nomogram and analyzing your results is really important,” says Dr. Donaldson. “If a patient has a complication or needs an enhancement, and you’re not following your own postoperative outcomes, it can be difficult to know the side effects or what the full patient experience is unless you’re closely following your own patient results.
“Track your results and analyze the patient experience throughout the whole process,” she says. “The process begins preoperatively and extends through surgery and the postoperative course. Presbyopia-correcting lenses can have some limitations and need enhancements much more frequently than standard distance lenses. Our job doesn’t end at the end of the surgery. In fact, a lot of times, that’s just the beginning. Some of these patients may take six months to neuro-adapt. Sometimes we may be waiting a few months because we want to do a refractive enhancement, but the patient isn’t stable yet. The postop process can be lengthy with premium lens technology.
“We also tend to do Nd:YAG lasers more frequently in our multifocal-lens patients than in our standard-lens patients because they’re much more sensitive to small opacities and any small degree of ocular surface disease,” she continues. “This may require extended amounts of time preoperatively and postoperatively to manage their ocular surface disease, more so than with a standard-lens patient.”
Dr. Khandelwal adds that it’s important to educate your technicians about the type of work-up necessary for premium lens patients. “Cataract surgeons need to know their outcomes with different lenses,” she says. “If all your technicians are doing for patients with astigmatism- or presbyopia-correcting lenses is checking their visual acuity and not refracting them, you’re not going to know what your individual refractive targets are. That’s very important with these lenses. We educate our technicians, even our float technicians, that when a patient has a premium lens, they need to check distance, intermediate and near vision, and look for any astigmatism, because these can all affect outcomes. Tracking your outcomes allows you to become a better surgeon because you know what your refractive outcomes are for your cases with these particular lenses.”
Dr. Donaldson consults for Alcon, Johnson & Johnson Vision, Carl Zeiss Meditec, LensAR and Bausch + Lomb. Dr. Miller consults for Alcon, Johnson & Johnson Vision and Oculus USA. Dr. Khandelwal consults for Alcon, Bausch + Lomb and Zeiss. Dr. Thompson discloses financial relationships with Alcon, Bausch + Lomb, Rayner, Zeiss, Vance Thompson Vision and Absolute Presbyopia.