The 65-and-over population is expected to increase globally over the next several decades; with it, the proportion of people with cataract and frailty should grow correspondingly.1 While cataract patients with age-related physical disability represent one group that might benefit from getting bilateral cataracts
 |
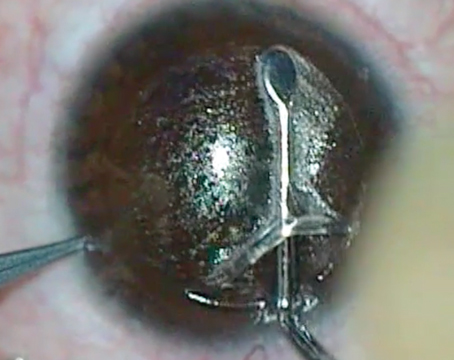
| Avoidance of enzymatic detergents when cleaning surgical tools, or using disposable components where possible, may minimize the risk of bilateral TASS. |
removed at the same time, staggering cataract surgeries is still standard practice in the United States. Here, surgeons who offer immediate bilateral cataract surgery describe why, how and for whom they do it.
“I do it, but very rarely and in accordance with very strict criteria,” says Derek W. DelMonte, MD, assistant professor of ophthalmology at the University of Colorado in Denver. “I’ll do same-day bilateral cataract surgery when the whole-body benefits to the patient clearly outweigh the drawbacks of doing each eye separately. Some patients will have trouble getting to the operating room twice, and some cannot cooperate with me and will require general anesthesia because of some physical or mental disability. For those patients, I’ll do both eyes on the same day. I’ll operate on both eyes in one day for my patients with Down syndrome, for example.”
Dr. DelMonte thinks even more of his patients could benefit from same-day bilateral procedures, but reimbursement issues are another factor prompting his selectivity. “Economically, it does benefit the patient in terms of less downtime and less follow-up, but since Medicare will only reimburse the second eye of a same-day bilateral procedure at 50 percent, I think that continues to limit the number of same-day procedures,” he says. “There are systems like Kaiser Permanente where surgeons are doing same-day procedures a great deal and enjoying great success with them. But for now, I generally don’t perform same-day procedures, except where the benefit to the whole patient is clear.”
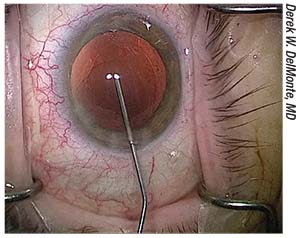
The Kaiser Permanente medical group isn’t subject to Medicare’s reimbursement model for Medicare Advantage patients: Patient care is allocated in prepaid, capitated lump sums. Its providers have been offering immediate bilateral cataract surgery (IBCS) since around 2010. Prior to that, Neal H. Shorstein, MD, of Kaiser Permanente’s ophthalmology and quality departments in Walnut Creek, California, collaborated with colleagues to investigate its safety and outcomes in their 21 independent surgical centers. “In Walnut Creek, we had patients several years ago ask about whether we’d do both eyes on the same day. At the time we weren’t doing it. There were ophthalmologists in some of our other medical centers doing it,” he recalls. “In other places—Canada and the Canary Islands in particular back then—some surgeons did a lot of bilateral same-day surgery. A group of surgeons and other stakeholders at Kaiser Permanente looked at this, and they found some controversy in the literature with regard to outcomes.”
Infection and Inflammation Risk
Specifically, Dr. Shorstein says their review spotlighted three main concerns about IBCS: fear of bilateral endophthalmitis; fear of bilateral toxic anterior segment syndrome (TASS); and the idea that the first eye’s visual outcome informs IOL selection for the second eye, making staggered surgeries superior.
“Regarding endophthalmitis, there have been no reported cases of bilateral endophthalmitis, except in developing countries where the recommended procedures of doing bilateral surgery weren’t followed,” he says.2
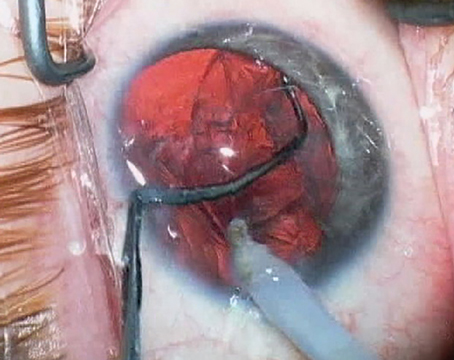
Dr. DelMonte says intracameral injections help to minimize endophthalmitis risk. “I think that cataract surgery has become so safe, thanks in part to intracameral injections, that the risk of monocular endophthalmitis and other complications is miniscule, and bilateral risks are similarly low—although I know that if a patient were to be affected bilaterally, that would be a very dire situation,” he says.
Dr. Shorstein, who uses intracameral antibiotic at the close of surgery, cites the International Society of Bilateral Cataract Surgeons (iSBCS) with regard to sterilizing equipment and maintaining a separate surgical tray for each eye. “Steve Arshinoff, a leader of the iSBCS, recommends having two separate surgical trays, and also recommends separating as many of the pharmaceutical products as possible in terms of their lot numbers. Then, if there was some manufacturing abnormality or irregularity, it wouldn’t affect both eyes,” he says.
Dr. Shorstein says that TASS has become less prevalent in recent years. “In the past five years or so, there have not been a lot of publications reporting TASS,” he says. “I think that’s because the ophthalmologi
 |
| Enrolled members of the Kaiser Permanente medical group in Northern California can routinely undergo noncomplex, immediate bilateral sequential cataract surgery. Benefits to the patient include lower cost and a quicker return to work, driving and other activities. |
c community has now recognized the best practices to prevent it.” He attributes the apparent reduction of TASS cases after cataract surgery to increased attentiveness to cleaning viscoelastic out of the phaco handpiece and to better cleaning of the tips after surgery. “Refraining from the use of enzymatic detergents is helpful, but if you must use enzymatic detergents to clean something as required per manufacturer instructions, then I think thoroughly rinsing away the detergent has also been very helpful in reducing TASS. We did a top-down risk analysis by going through all the steps of our cleaning and sterilization.” he says.
In addition to the established practice of using intracameral antibiotic injections, Kaiser Permanente—which does not promulgate rules for its surgeons, but does have established policies and procedures for its surgery centers—recommended the following:
• Use separate surgical trays for each eye. “We emphasize that it’s very important to separate surgical trays. When you’re done with one eye, completely take down the draping and gloves, and re-scrub as you would for a completely new patient for the second eye, with a new tray,” says Dr. Shorstein.
• Consider going disposable. “Our content experts felt that for any instruments that have very small lumens, like cannulas, the risk of TASS is small if they’re cleaned very thoroughly. But they still tended to recommend disposable cannulas for these cases, and I agree.” Dr. Shorstein says.
• Use intracameral antibiotic preparations with a different lot number for each eye. “Since there’s still no intracameral antibiotic manufacturer in this country, it has to be compounded. We use a 503(B)-compliant outsourcing facility,” says Dr. Shorstein. “We separate the intracameral antibiotics by lots in case of any potential irregularity. Then, if the worst-case scenario occurs, we’ve decreased the risk of bilateral TASS or endophthalmitis because we’re using different lot numbers.”
Dr. Shorstein says that his practice setting isn’t currently separating viscoelastic by lot numbers in IBCS cases, however. The iSBCS goes further, recomending the separation of surgical products by lot number wherever it’s “reasonable…and possible.”3
Refractive Outcome Concerns
“Another concern about same-day cataract surgery has been about forgoing the opportunity to refract the first eye a few weeks postoperatively. Theoretically, you could adjust the IOL selection in the second eye if you missed the target uncorrected vision for the first eye,” says Dr. Shorstein. His research group decided to test that theory in a 2017 retrospective comparative study that looked at visual outcomes of 13,711 delayed sequential bilateral cataract surgery (DSBCS) patients and 3,561 immediate sequential bilateral cataract surgery (ISBCS) patients who had noncomplex surgeries performed as members of Kaiser Permanente Northern California from January 1, 2013 through June 30, 2015. They found no significant difference in postoperative BCVA or refractive error between the two groups, and no increase in the risk of complications, including endophthalmitis.4
“There’ve been a bunch of studies done in the past generally showing that if you were off on the first eye, then selecting an adjustment for the second eye of half the correction would likely get the second eye close to where you’d want to be visually,” explains Dr. Shorstein. “For example, if the first eye turned out to be -1 D (for a target of plano), then you’d want to select an IOL with 0.5 D less power for the second eye. But what we concluded was that it didn’t appear that a lot of correction was going on in the different-day patients. This wasn’t a prospective study, so we can’t say that there was absolutely no effect from giving up the ability to correct the second eye based on the first eye by doing bilateral same-day procedures: But we can say that given this retrospective look-back, there was no evidence that much correcting was happening. That’s because commercially available IOLs only come in half-steps to begin with, so you’d have to be off by a diopter or more in the first eye to really fiddle with your IOL selection in the second eye. To change it by a half-diopter, you’d have to be off by one or more.”
For two particular patient groups, Dr. DelMonte performs only delayed sequential bilateral surgeries. “I will always stagger the surgeries for patients who are getting premium IOLs and for post-refractive eyes, because I think it’s important to get information about the refractive outcome from the first eye to fine-tune power calculation and lens-selection considerations for the second eye. I’ve had some patients ask for a little more near for reading in the second eye, for example, so I’ll use the results from the first to help zero in on what those patients want. But I do understand that there are other surgeons who like to do premium IOLs at the same time in order to help their patients adapt more quickly to the technology in terms of depth of focus, stereopsis, etc. It’s really about what patients want when they’re getting premium lenses,” he says. “I also think that the first eye needs time to heal before you arrive at a stable refractive outcome, but I think that information becomes clear and reliable within about one week postop.”
The iSBCS recommends writing the target refractive information for both eyes on a board visible to everyone in the OR. Dr. Shorstein’s group says consent-form language should always clearly stipulate each eye’s IOL type and targeted working distance vision, and that it’s critical to clearly delineate these between the patient’s left and right eyes in ISBCS by keeping the fully signed consent form with a biometry printout for the operative eye in the OR, for only one eye at a time, during immediate bilateral procedures.4
Safety and Savings
In the Kaiser Permanente study, 25 cases of planned ISBCS became DSBCS because the first-eye surgery was not uncomplicated, and so the second-eye procedure was rescheduled. “In our organization, if there’s a complication in the first eye that could in any way impact the vision or healing of that eye, the consensus is to stop and not proceed to the second eye,” says Dr. Shorstein. “We let the first eye heal. It’s easier for the patient—and probably the surgeon as well.”
Same-day bilateral cataract surgery is still relatively uncommon in the United States, but for the right patients and with some extra precautions, advocates say it can save downtime and money, restoring patients to full visual function faster. “I think that as the procedure becomes safer and safer, we’ll see more people offering this,” says Dr. DelMonte. “I also think that statistically, the inherent risk of driving to your follow-up appointments for delayed sequential bilateral procedures is higher than that of complications stemming from same-day bilateral surgery.” REVIEW
Dr. DelMonte and Dr. Shorstein have no financial interests relevant to any products mentioned in this article.
1. Fukuoka H, Afshari NA. Importance of age-related cataract on of frailty in an aging global population. Curr Opin Ophthalmol 2017;28:1:93-7.
2. Li O, Kapetanakis V, Claoue C. Simultaneous bilateral endophthalmitis after immediate sequential bilateral cataract surgery: What’s the risk of functional blindness? Am J Ophthalmol 2014;157:749-51.
3. Arshinoff S, Claoue C, Johansson B. iSBCS General Principles for Excellence in ISBCS 2009; 2009. http://isbcs.org/wp-content/uploads/2011/03/2010-07-20-FINAL-ISBCS-SBCS-suggestions-from-ESCRS-Barcelona.pdf. Accessed March 5, 2018.
4. Herrinton LJ, Liu L, Alexeeff S, Carolan J, Shorstein NH. Immediate sequential vs. delayed sequential bilateral cataract surgery: Retrospective comparison of postoperative visual outcomes. Ophthalmol 2017;124:1126-35.