In an effort to make surgery a more comfortable and predictable experience for the patient, refractive surgeons have progressed from procedures such as RK and PRK, which elicit a healing response with all its attendant issues, to LASIK, a procedure that minimizes the role of healing. Now, some surgeons are taking this idea even further by perfecting femtosecond intrastromal treatments that involve minimal manipulation of the corneal surface. Here’s a look at how the procedures work and their current outcomes.
Intracor
Intracor is an intrastromal treatment for presbyopia that was originally developed by Colombian surgeon Luis Ruiz using the Technolas Perfect Vision femtosecond laser.
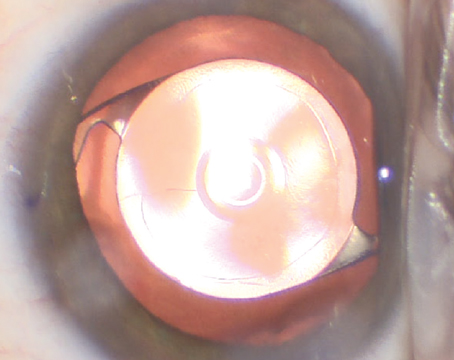
In Intracor, which takes about 20 seconds to perform, the surgeon uses the laser to create five concentric rings of different depths, centered on the pupil, in the cornea of the patient’s non-dominant eye. The inner ring is approximately 0.9 mm in diameter and the outer ring is 3.2 mm. “None of the rings perforates the cornea,” explains Intracor surgeon Tobias Neuhann, MD, of Munich, Germany. “They are beneath Bowman’s and above Descemet’s membrane, so they’re truly intrastromal. The goal of the rings is to create a little steepening of the central cornea.”
Intracor currently is indicated for emmetropic presbyopes, though it can work for patients with between +0.5 and +1.5 D of error. “If the patient is more hyperopic than that or is myopic, we can’t do it,” Dr. Neuhann says. “This is because the treatment induces a little myopia.”
Researchers from Heidelberg, Germany, did a prospective, multicenter study on 63 presbyopes who underwent Intracor.1 The researchers report that the median uncorrected distance visual acuity of 20/25 (r: 20/63 to 20/20 preoperatively and 20/63 to 20/16 postoperatively) and the best-corrected distance acuity of 20/20 (r: 20/32 to 20/12.5 preop and 20/40 to 20/16 postop) remained stable. Median spherical equivalent changed from +0.63 D preop to plano postop. The median uncorrected near visual acuity increased significantly from 20/100 preop (r: 20/200 to 20/32) to 20/32 postop (r: 20/125 to 20/16) and eyes gained a median of four lines (r: one to nine lines). The study surgeons noted a loss of two lines of best-corrected vision in 7.1 percent of eyes, and that the rings were faintly visible at a year postop.
The procedure also doesn’t have a negative effect on future intraocular lens calculations the way LASIK does. “We haven’t specifically studied Intracor in patients with cataracts or who are having cataract surgery, because cataract is an exclusion criterion for our Intracor studies,” explains Dr. Neuhann. “But if an Intracor patient develops a cataract later on, we have found that the use of a customized aspheric, monofocal IOL, corrected for distance as usual, works well. Plus, we can just use the normal IOL calculation formulas.”
|
Ideally, when you create the five circular rings, you will separate each layer from the next. In these underperformers, however, there are a lot of tissue bridges that seem to keep the corneal layers in place. So the problem becomes, how can you break apart the layers without being able to touch the incisions? After studying these patients, we’ve begun an enhancement procedure that involves massaging the cornea in an effort to break the tissue bridges. In two underperforming patients, we got a dramatic enhancement with the massage. However, these results are just a clinical observation at this point, and the massage enhancement technique isn’t CE-marked.” Dr. Neuhann says that, in one of the underperformers, the postop massage took his reading vision from J7 to between J1 and J2 in one day.
The challenge with the massage enhancement technique is standardizing it. “Based on my favorable clinical impression, we now ask, ‘OK, how can we develop a treatment protocol that everyone can do?’ ” says Dr. Neuhann. “In other words, right now, I do a hard massage while some surgeons might do a soft one—this isn’t the way to go. We have to find a simple, effective procedure to use on non-performers at one or two weeks postop.” He says it’s also not feasible to massage everyone’s cornea because that would result in the successful patients actually experiencing an overcorrection.
Looking to the future, Dr. Neuhann says one of the next steps is developing an Intracor treatment for low myopes. “For them, we add intrastromal, radial-like incisions in the corneal periphery,” he explains. “However, it doesn’t work very well right now. It seems to be the same problem as with the underperformers: We do a nice incision but have no effect, probably because there are tissue bridges that form due to the cornea being much thicker in the periphery.”
Though postoperative problems such as tissue bridges persist, Dr. Neuhann thinks they’ll eventually be overcome with the art of surgery as well as the science. “There’s a lot of ‘music’ in this technique,” he says. “It takes time.”
ReLEx FLEx and SMILE
Another approach to intrastromal ablations is refractive lenticule extraction, an approach taken by users of the Carl Zeiss Meditech VisuMax laser. ReLEx uses the laser to carve out an intrastromal lenticule, which is then removed in one of two ways in order to bring about a change in refraction.
The first ReLEx method that was devised, known as femtosecond lamellar extraction or FLEx, involves using a LASIK-like flap to gain access to the lenticule in order to remove it. The second method, called small-incision lenticule extraction, is less invasive, and involves teasing out the lenticule through a small corneal incision, between 2 and 4 mm wide, leaving the rest of the cornea intact.
“FLEx has started to disappear,” says Marburg, Germany’s Walter Sekundo, MD, who, along with Marcus Blum, MD, of Erfurt, Germany, introduced the ReLEx FLEx procedure around five years ago. “People are extremely keen on going through a small-incision for ReLEx, because that’s what makes the procedure so attractive and truly different from LASIK. In some ways, FLEx is a transitional procedure that was developed first and was further elaborated upon to create ReLEx SMILE.” Currently, ReLEx can treat myopia up to approximately -11 D and astigmatism up to about -5 D.
“I like the SMILE procedure better than FLEx because, from a biomechanical standpoint, it leaves a much stronger cornea compared to one in which you’ve made a flap,” says Aarhus, Denmark, surgeon Jesper Hjortdal, MD, PhD, who has done hundreds of ReLEx procedures. “Also, studies will soon begin to emerge that show that you have a better preservation of corneal sensitivity in the first weeks or months after surgery with SMILE, which probably will result in less dry eye. And then there are the potential complications related to having a flap on the eye: late trauma; flap dislocation; epithelial downgrowth with a large flap, etc. You won’t have any of these potential complications after a SMILE procedure.”
Surgeons say experience has brought a knowledge of tips and tricks to improve outcomes. “SMILE is slightly more manual compared to femto-LASIK or microkeratome-based LASIK because you have to get into this small corneal tunnel to extract the lenticule,” says Dr. Hjortdal. “If the lenticule isn’t completely free, you have to go in with a small spatula and break the remaining small tissue bridges, so this process involves some manual manipulation. It can help to place the removed lenticule on top of the cornea to make sure you’ve removed every part of it. Also, if you have to go in and loosen a lenticule, it’s important to loosen the tissue above the lenticule first before loosening it below. This is because if the lenticule is sort of stuck on the anterior cap, it can be difficult to free it.”
|
“For patients in whom I’m doing a SMILE procedure, I still use a 4-mm incision,” adds Dr. Sekundo. “Some surgeons use 2-mm incisions, but if you run into trouble, a 2-mm incision might become difficult to handle.”
Surgeons say the results of FLEx and SMILE are comparable to LASIK, and may have the potential to be better. In one study, surgeons performed SMILE on 51 eyes of 41 patients with a mean spherical equivalent of -4.87 D. Six months postop, the SE was +0.03 D, and refractive stability had been achieved by the first month. Seventy-nine percent of the eyes saw 20/25 or better uncorrected, and the surgeons say the six-month postop best-corrected vision was the same or better than the preop best-corrected vision in 95 percent of eyes. Two eyes lost a line of best-corrected vision.2
Dr. Hjortdal thinks ReLEx is an attractive option for high myopes because, though it has a certain amount of error associated with it, as any treatment would, the small amount of error stays constant from low to high myopes. “So you can’t say it’s more precise with low myopia,” he says. “But you can turn it around and say that it’s as precise with high myopia as it is with low. At my center, we predominantly treat high myopia with it, -6 D to -11, so if there’s one group that could benefit from this more than the others it would be the high myopes.” He says in his practice, in the 800 ReLEx patients he’s done (mean error: -7.5 D) there’s been an undercorrection of 0.1 ±0.4 D. For astigmatism, he says it undercorrects by 25 percent of the target value on average, but adds that this could be improved upon by modifying the nomogram down the road.
Dr. Sekundo says his long-term outcomes have been very stable, possibly surpassing LASIK. “After five years, regression in my ReLEx patients is only 0.07 D,” he says. “I’m not saying femto-LASIK can’t provide these numbers—you could get close with it—but you probably couldn’t achieve this low level of regression with LASIK, as it is essentially nothing. The problem with excimer ablation is the higher you go in terms of refractive error, the more keratocyte activation there is because it’s not a cold laser. It warms up tissue. When you start to cook keratocytes, they react by producing extracellular collagen, which thickens the cornea and gives you regression. With ReLEx surgery, when I do -10 D, I get the result of -10 D without having to fight the regression to the extent I would if I had performed excimer laser ablation.”
As surgeons have mentioned, one of the possible challenges is handling an enhancement in a SMILE patient, since there is no flap to lift. “In SMILE, one option is to do PRK on top of the cornea, because it’s usually a low amount of correction,” says Dr. Hjortdal. “We’ve done that in two cases. We’ve also done one case using femto-LASIK where we make a traditional LASIK flap and treat the bed. The last possibility, which we haven’t tried, is to cut down to that space where you removed the SMILE lenticule and then lift up the flap.”
The next frontier with ReLEx is hyperopic treatments, and Dr. Sekundo and Dr. Blum have already applied for approval to begin a second study of it. “For hyperopia, the lenticule’s shape is different,” Dr. Sekundo explains. “It’s thicker on the edge than in the center, so, theoretically, it should be easier to grasp. But the challenge is the transition zone. You don’t need a transition zone for myopia, but you do for hyperopia, and it’s probably a key issue in terms of preventing regression.”
Intrastromal AK
In the spring of 2012, AMO/Visx’s IntraLase laser received 510(k) clearance to perform intrastromal astigmatic keratotomy, giving surgeons a less-invasive option for patients with astigmatism.
Steven Schallhorn, MD, is medical director for the U.K.-based refractive surgery chain Optical Express, and says the company’s centers have performed more than 100 intrastromal AKs. “My initial take is that it works. It’s titratable and safe, and it effectively reduces cylinder, at least in our analysis of it,” he says.
Dr. Schallhorn took part in a study of 110 eyes of 93 patients with astigmatism after cataract or refractive surgery who underwent intrastromal AK. Their mean preop cylinder was -1.27 D (r: -3.5 to -0.5 D). The IntraLase created the incisions beginning at 60 µm below the surface down to 80 percent depth at a 7-mm optical zone. At three months, the mean cylinder was -0.61 ±0.5 D (r: -2.75 to 0), and 55 percent of the eyes could see 20/20 or better uncorrected vs. 17 percent preop. Fifty-nine percent had no more than 0.5 D of cylinder postop. On average, the treatments achieved 78 percent of the intended cylinder correction. “It indicates an undercorrection,” says Dr. Schallhorn. “But it was similar across the different levels of preop cylinder, which means we could titrate the results.” (Schallhorn J, et al. IOVS 2012;53:ARVO E-Abstract 1504)
Dr. Schallhorn says intrastromal AK may find a niche. “In cataract surgery, you have patients in that low to moderate range of astigmatism where you may not want to place a toric lens but where the corneal astigmatism is visually significant,” he says. “The advantage of intrastromal incisions is that there’s no epithelial break, which means fast recovery and stability. However, the potential advantage of incisions that go from the epithelium downward is that if you don’t get the effect you like, you can go back a week later, for example, and open the incisions with a Sinskey hook and you’re likely to get more of an effect. With that approach, though, I’m concerned about the predictability.”
Dr. Schallhorn notes that, because of the way the IntraLase is doing the incisions, in a non-cataract patient the spherical equivalent refraction must be zero or close to zero preop, because the incisions’ coupling effect will leave the SE the same.
The next step for intrastromal AK will be honing the nomogram. “It needs refinement,” says Dr. Schallhorn. “But it shows the procedure is titratable, meaning you can correct more cylinder in a controlled fashion than with the simple nomogram we’re using. My approach to this has been to use a simple nomogram, evaluate it carefully and scientifically, then move on to the next step. We’re in the process of seeing how we can refine the treatment now that we have a substantial amount of data.” REVIEW
1. Holzer MP, Knorz MC, Tomalla M, Neuhann TM, Auffarth GU. Intrastromal femtosecond laser presbyopia correction: One-year results of a multicenter study. J Refract Surg 2012;28:3:182-188.
2. Shah R, Shah S, Sengupta S. Results of small incision lenticule extraction: All-in-one femtosecond laser refractive surgery. J Cataract Refract Surg 2011;37:1:127-37.