Thoughts and opinions on LASIK flap creation are just one of the topics tackled by surgeons in this month’s e-mail survey on refractive surgery. The survey e-mail was opened by 1,509 of 10,000 subscribers to Review’s electronic mail service (15-percent open rate), and 69 surgeons responded. Here’s what they had to say.
The Tale of the Tape
On the survey, 59 percent of surgeons say they use flaps of 100 to 119 µm for most of their cases, followed by 24 percent who like a thickness between 120 and 130 µm. Six percent make flaps thinner than 100 µm, 6 percent like flaps that are between 131 and 149 µm and 6 percent make flaps thicker than 150 µm. For flap-making, two-thirds of the surgeons use a femtosecond laser, with the rest using a microkeratome.
“The 100- to 119-µm thickness is a good balance of a stable flap and a good stromal thickness for ablation,” says Los Angeles surgeon Uday Devgan. A surgeon from Memphis agrees. “It’s a good compromise,” he says. “It’s thin enough to get the maximum amount of stroma available to ablate, but thick enough to avoid striae after repositioning.” A surgeon from Indiana says this thickness range may be the threshold at which any thinner flaps might start causing issues. “It’s thick enough to prevent sub-epithelial haze,” he says.
 |
Procedure Volume
Every surgeon has a procedure that he trusts more than the others, and for the refractive surgeons on our survey it’s custom LASIK, chosen by 43 percent as their procedure of choice. Twenty-eight percent say they use conventional LASIK the most, followed by PRK at 15 percent and wavefront-optimized LASIK at 13 percent.
In terms of LASIK volume, surgeons report that things are still sluggish. Forty-eight percent of the surgeons do between five and 20 cases per month and 28 percent perform fewer than five. Eleven percent do between 21 and 50 cases and 2 percent perform between 51 and 75. On the high-end of volume, 6 percent of surgeons report doing between 76 and 100 cases, and 6 percent say they do more than 100 monthly. Surgeons say that they charge an average of $2,452 per eye for LASIK and $2,404 for PRK.
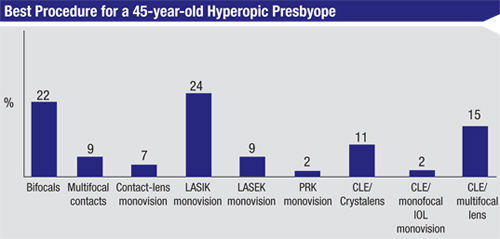
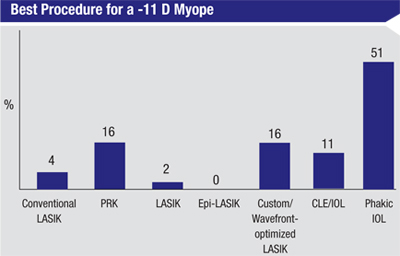
The procedures that surgeons favor change, however, when faced with cases that are outliers. For a high-myope (-11 D), about half (51 percent) say they think a phakic IOL is best; 16 percent like either custom or wavefront-optimized LASIK; 16 percent prefer PRK; 11 percent like using clear-lens extraction/intraocular lens implantation; 4 percent prefer conventional LASIK; and just 2 percent like LASEK. “A -11 correction is beyond the scope of good LASIK,” says Dr. Devgan. “Phakic IOLs are OK, but the best option—and lowest risk—is to stick with contact lenses.” A surgeon from Wisconsin thinks a phakic lens is the best option. “Optical aberrations occur with excessive corneal flattening,” he says. “Although it’s a small risk, retinal detachment is a risk in high myopes with clear-lens extraction/IOL implantation.”
Some surgeons, however, think ablation has some benefits in these patients. “Femtosecond wavefront LASIK has been excellent for higher myopes, with accurate and quicker visual recovery and no haze concern,” says Dr. Andreason. “However, corneal thickness may limit us to using custom PRK—which is good—but not my preference in this case.” Clifford Salinger, MD, of Palm Beach Gardens, Fla., thinks LASEK fills the bill better, and outlines his course of action and the reasons why he likes LASEK. “Preoperatively, have the patient screened by a retinal specialist to rule out any peripheral retinal pathology; otherwise, the patient and his attorney will point to surgery as the causative factor,” he says. “LASEK allows more residual stromal bed thickness; 250 µm is an arbitrary thickness advised by the FDA that does not guarantee corneal structural integrity that would avoid long-term corneal ectasia. In addition, LASEK avoids applying a suction ring or Intralase suction to the eye that can induce structural changes to the vitreous and possibly increase the likelihood of retinal detachment.”
 |
Robert Epstein, MD, of McHenry, Ill., will alter his course of action depending on the patient. “If the patient is otherwise a LASIK candidate, wavefront-guided LASIK would be done on the distance eye and possibly PRK on the near eye to minimize the risk of late ectasia,” he says. “[For] 48-year-olds the answer would be a bifocal procedure on the non-dominant eye, so there are some people whom I tell to wait until they are older. But hyperopic presbyopes have a lot to gain from refractive surgery and are the most appreciative.”
For the patient in need of an enhancement of her LASIK, surgeons are divided nearly down the middle: 50 percent will lift the previous flap and ablate and 45 percent will perform a surface procedure on top of the flap. Five percent will re-cut a flap and ablate. For his part, Dr. Epstein prefers to take the surface ablation route. “I prefer PRK over the LASIK flap only,” he says. “After many episodes of cells in the interface over the past 23 years since I started LASIK I just find it easier to go with the slower healing of PRK for the sake of the predictability of having no problems with cells. When we used to do LASIK reoperations we did find a lower rate of epithelial cells in the interface when suturing the flap with the Barraquer eight-bite, anti-torque suture, and cells could be squirted from the interface postoperatively, but it is just too much trouble. PRK is fine.” Dr. Salinger, however, thinks a procedure that involves lifting the flap is better in the end. “I prefer it if the available corneal thickness allows for this option,” he says. “If the patient chose LASIK for the initial procedure, then lifting the flap and performing another LASIK is the fast-healing alternative that he is probably hoping for in terms of a second vision correction procedure.” REVIEW



