Punctal Plugs
According to Robert Latkany, MD, founder of the New York Eye and Ear Infirmary’s Dry Eye Clinic, it can be argued that punctal plugs are a natural treatment because their sole purpose is to keep patients’ own tears on their eyes longer. “You can use a temporary plug just to give it a shot and see if it works,” he says. “You can always move on to a silicone, non-dissolvable plug afterwards. These are a wonderful option, especially if the patient doesn’t have allergies or rosacea.”
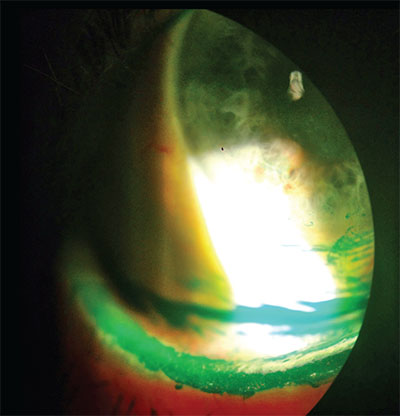 |
| Classic lissamine green staining two minutes after instillation. These staining patterns show both the patient’s lid wiper epitheliopathy and dry-eye disease. Some physicians are turning to organic treatments in addition to traditional tears and prescription medications to treat these patients. |
Nutritional Supplements
Nutritional supplements are widely used and have also been found to be an effective therapy for dry eye. “Nutritional supplements for dry eye have been around for 10 or 15 years,” notes Dr. Latkany. “They are part of my regimen, and I usually start out with 1,000 mg of fish oil a day. Some people are opposed to the fish component, so they use flaxseed oil instead. Patients can titrate upwards based on their response rate.”
A number of studies have demonstrated that oral nutritional supplements are an effective treatment for dry-eye symptoms. In one recent report, sponsored by nutraceutical-maker Brudy Technology (Barcelona, Spain), a total of 1,419 patients with dry-eye syndrome who were using artificial tears participated in a 12-week prospective study.1 Patients were instructed to take three capsules/day (1.5 g) of the company’s nutraceutical formulation Brudysec. The following variables were assessed: dry-eye symptoms (scratchy and stinging sensation, eye redness, grittiness, painful and tired eyes, grating sensation and blurry vision); conjunctival hyperemia; tear breakup time; Schirmer I test; and Oxford grading scheme.
At 12 weeks, all dry-eye symptoms improved significantly, and artificial tear use decreased significantly from 3.77 times per day at baseline to 3.45 times per day. In addition, the Schirmer test scores and the TBUT increased significantly, and there was an increase in patients grading 0 to I on the Oxford scale and a decrease of those grading IV to V. Additionally, significant differences in improvements in dry-eye symptoms were found between compliant and noncompliant patients as well as between those with moderate/severe and those with none/mild conjunctival hyperemia. In another study, oral administration of re-esterified omega-3 fatty acids (Dry Eye Omega, Physician Recommended Nutraceuticals) resulted in a statistically significant improvement in tear osmolarity, as well as improvements in such secondary endpoints as corneal staining and tear breakup time.2 (Several of the study’s physicians received compensation from PRN.)
It’s Dr. Sheppard’s belief that inflammation is the underlying cause of dry eye. “Essential fatty acids are a non-pharmaceutical way of producing an anti-inflammatory effect,” he says, noting that balanced essential fatty acid therapy has been found to significantly improve signs and symptoms of dry eye. “I’ve also found that gammalinoleic acid is very important for the ocular surface and is universally tolerated. It can be found in some commercial preparations, but it is also readily available in supermarkets and health-food stores as primrose, borage or black currant seed oil.”
A recent study sponsored by Taiwanese neutraceutical company Acrobio Healthcare found that oral antioxidant supplements may increase tear production and improve tear-film stability by reducing tear reactive oxygen species.3 This study employed a vegetable-based antioxidant supplement that’s safe and can be used as an adjuvant therapy to conventional artificial tear therapy for patients with dry-eye syndrome.
This prospective, randomized, double-blind study evaluated the effects of an antioxidant supplement (containing anthocyanosides, astaxanthin, vitamins A, C and E, and several herbal extracts, including semen Cassiae and Ophiopogonis japonicus) on patients with dry eye. The investigators assessed dry-eye symptoms, visual acuity, Schirmer’s test, TBUT, cornea and conjunctiva fluorescein staining, serum anti-SSA/anti-SSB antibodies, and the level of reactive oxygen species in tears. Patients took the supplements for eight weeks, and they were evaluated every four weeks for 16 weeks.
Forty-three patients (20 in the treatment group and 23 in the placebo group) completed the study. Patients’ liver and renal functions were normal. Diastolic blood pressure decreased in the treatment group; however, there were no significant differences in systolic blood pressure, dry-eye symptoms, serum anti-SSA and anti-SSB, visual acuity, intraocular pressure or fluorescein corneal staining among the groups. In the treatment group, TBUT scores and Schirmer’s tests without topical anesthesia significantly improved. Tear reactive oxygen species level differed between the groups and decreased after treatment. Additionally, patients’ overall subjective impression revealed a significant improvement with treatment compared with placebo.
Dr. Stonecipher says that the key to any therapy is making sure that patients are compliant. If patients are going to take a nutritional supplement, he says, it must be easy for them to purchase. He has also found that certain brands work better than others because they are more readily absorbed. “For an over-the-counter omega-3, I recommend PRN, Nordic Naturals or HydroEye,” he states. “I give patients a specific brand, and I send them to a specific website to order it online. You’ve got to make it easy. We used to sell supplements in our office to make it more convenient, but we’ve found that ordering it online is even easier. Our office has a computer in every lane, and either I or the technician walk through how to order nutraceuticals. When you are recommending an out-of-the-box product, it must be accessible.”
“Our patients have welcomed ready access to all of our recommended dry-eye products through our own practice-specific retail website at myeyestore.com,” Dr. Sheppard notes.
Masks and Goggles
 |
| Eyeseal 4.0 goggles from Eye Eco help protect patients’ eyes while they sleep. |
Warm Compresses & Lid Scrubs
According to Dr. Sheppard, meibomian gland awareness and therapy has become a significant area of interest over the past few years. “Now, we are all imaging the meibomian gland and producing more intelligent therapy than traditional baby shampoo,” he says. “When we understand that meibomian gland physiology is subject to geriatric and inflammatory degradation like everything else in the body, we can not only document morphologic changes in the meibomian glands, we can incorporate patients enthusiastically into the treatment paradigm, especially when they see that there are anatomical changes.”
Several topical scrubs are now available that are not only antiseptic, but also anti-inflammatory. “We have found this to be extremely beneficial, and we now recommend specific scrubs for all of our preoperative patients to sterilize the ocular surface or reduce the floral load and also to improve meibomian gland function and, therefore, provide an alternative therapy for ocular surface disease,” Dr. Sheppard adds.
Dr. Stonecipher also recommends the use of anti-dandruff shampoos and lid scrubs. “I use three anti-dandruff shampoos: Head and Shoulders; Selsun Blue; and T/Gel—specifically yellow T/Gel,” he avers. “A lot of people have a mixed-mechanism dry eye. Sometimes, this can affect the natural bacteria that are on the face and around the eyes. It is simple to wash your face with an anti-dandruff shampoo while in the shower. Just make sure not to get it in your eyes. I am also a huge fan of lid scrubs like Avenova by NovaBay.”
Warmth and Electricity
Alternative therapies in this area, such as LipiFlow, are becoming popular. “They are becoming a centerpiece for practice growth and patient awareness,” says Dr. Sheppard. “Additionally, in many cases, it is more readily adopted by patients [than prescription therapy]. All of the alternative methods that we have discussed and the many others that are out there are synergistic and complementary to prescription therapy, as well.”
Also, a recent study found that the therapy known as transcutaneous electrical stimulation can improve patients’ dry eye, both subjectively and objectively, without any adverse effects, so it may be a potential addition to the ophthalmologist’s dry-eye armamentarium.4
In this study, 27 patients with dry eye underwent transcutaneous electrostimulation. Electrodes were placed on the periorbital region of both eyes along with manual stimulation with a hand-piece conductor moved by the operator. Each patient underwent 12 sessions that lasted 22 minutes each. Sessions were spread over two months, with two sessions per week in the first month and one session per week in the second month. Ocular Surface Disease Index questionnaire, TBUT, fluorescein staining of the cornea, Schirmer I test and adverse events were assessed at baseline, at the end of treatment, and at six and 12 months after treatment.
Patients’ OSDI improved from 43 ±19.2 at baseline to 25.3 ±22.1 at the end of treatment, and this improvement was maintained at both six-month and 12-month follow-up evaluations. There was TBUT improvement in the right eye at the end of treatment and after 12 months in the left eye. The Oxford scores changed in both eyes at the end of treatment and at the six-month visit. Additionally, Schirmer I scores improved significantly at the end of treatment in the left eye and in both eyes at the 12-month evaluation. At the end of treatment and during the follow-up period, there was a significant reduction of the use of tear substitutes. No complications were reported.
“There is also excitement in the dry-eye community regarding neurostimulation therapy to stimulate natural tear production, which may be approved as early as the first quarter of 2017,” Dr. Sheppard notes, referring to the Allergan/Oculeve intranasal tear neurostimulator device.
One study of intranasal neurostimulation included 40 patients with mild to severe dry eye disease who were provided with a nasal stimulation device and instructed to use it at home four times daily.5 The study was sponsored by the device’s maker, Oculeve. The nasal stimulation device is noninvasive with probes that are placed in the nose to stimulate the lacrimal glands to produce tears. Patients were followed for up to 180 days. Schirmer scores were used to determine the difference between unstimulated and stimulated tear production. The study found that the mean stimulated Schirmer scores were significantly higher than the unstimulated scores at all visits. Additionally, corneal and conjunctival staining and symptom scores from baseline to day 180 were significantly reduced.
Also, a study has found that intense pulsed light therapy effectively treats evaporative dry eye disease. IPL has been used by dermatologists as a rosacea treatment for years, and now it is being used to treat meibomian gland disease and evaporative dry eye. The treatment consists of delivering 10 to 15 treatment spots to the upper cheek and lateral canthal area with an intense pulsed-light handpiece. The physician usually makes two passes. In a study of IPL, researchers reviewed clinical data from 100 patients who were diagnosed with evaporative dry eye.6 On average, patients underwent four IPL sessions during the two-year study period, and there was a significant decrease in scoring of lid margin edema, facial telangiectasia, lid margin vascularity, meibum viscosity and OSDI score. Additionally, there was a significant increase in oil flow score and TBUT.
As far as the future of alternative dry-eye therapies, Dr. Sheppard says: “The fact that the marketplace is expanding tells us that these therapies are working.” REVIEW
Dr. Sheppard is a consultant for Allergan, Alcon, Novartis, Abbvie, Science Based Health, TearLab, Tear Science, Shire and Bausch + Lomb. Dr. Latkany has a licensing agreement with Eye Eco for his eye mask. Dr. Stonecipher is a consultant for AMO, Alcon, Allergan, Bausch + Lomb, Ellex, Nidek, Presbia, Refocus and Shire.
1. Gatell-Tortajada J. Oral supplementation with a nutraceutical formulation containing omega-3 fatty acids, vitamins, minerals, and antioxidants in a large series of patients with dry eye symptoms: Results of a prospective study. Clin Interv Aging 2016;19:11:571-578.
2. Epitropoulos A, Donnenfeld E, Shah Z. Effect of oral re-esterified omega-3 nutritional supplementation on dry eyes. Cornea 2016;35:9:1185-1191.
3. Huang JY, Yeh PT, Hou YC. A randomized, double-blind, placebo-controlled study of oral antioxidant supplement therapy in patients with dry eye syndrome. Clin Ophthalmol 2016;9:10:813-820.
4. Pedrotti E, Bosello F, Fasolo A, et al. Transcutaneous periorbital electrical stimulation in the treatment of dry eye. Br J Ophthalmol 2016 Sept 22. Epub ahead of print.
5. Friedman NJ, Butron K, Robledo N, Loudin J, Baba SN, Chayet A. A nonrandomized, open-label study to evaluate the effect of nasal stimulation on tear production in subjects with dry eye disease. Clin Ophthalmol 2016;10:795-804.
6. Gupta PK, Vora GK, Matossian C, Kim M, Stinnett S. Outcomes of intense pulsed light therapy for treatment of evaporative dye eye disease. Can J Ophthalmol 2016;51:4:249-253.



