In 1873 Charles Blackley, a general practitioner, wrote, "Hay fever is said to be an aristocratic disease, and there can be no doubt that, if it is not almost wholly confined to the upper classes of society, it is rarely, if ever met with but among the educated."1 His initial observations of allergy patients included only members of the clergy, military, medical men and merchants. Today, with articles in the literature such as "Asthma and Atopy—The Price of Affluence?"2 how far have we come from Blackley's investigations? Here, we'll consider whom allergy affects, and why.
Mechanisms of Allergy
Though some of Blackley's 19th-century postulations may seem amusing today, many of his observations hold true. While several of his contemporaries hypothesized that hot weather, the aromas released by flowers and grasses or even the "diminishing of clothing" during the summer months were the causes of allergy, Blackley drew conclusions from his experimentation and observations of hay-fever allergies.
He accurately concluded that, "Pollen of all kinds will give rise to some of the symptoms of hay-fever, and all the other so-called causes have little or nothing to do with the disease." His suggested treatment included a "sojourn at the seaside" or a "cruise in a yacht," to remove the individual from the influence of pollens based inland.
|
Today, the basic tenets of many of Blackley's conclusions still apply, and we've amassed a wealth of knowledge regarding the immune-system actions and mechanisms controlling allergic conjunctivitis.
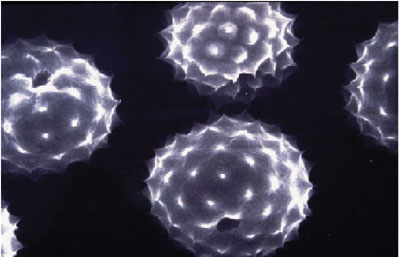
The pathogenesis of allergic conjunctivitis, a Type-I hypersensitivity reaction, is facilitated by Th2 cells, a specific subset of Th helper cells that produce many of the interleukins involved in the allergic response and promote mast cell and eosinophil growth. Stimulation of Th2 promotes B-cell production of IgE, via the influence of Th2-specific interleukins (IL-4, IL-13). The end result is production of IgE, the immunoglobulin responsible for triggering an allergic reaction. IgE binds to and cross-links on the surface of mast cells, signaling the cell to degranulate and release its allergic mediators, including histamine, to cause the itching, redness, chemosis, lid swelling and tearing characteristic of an ocular allergic reaction.
• Allergens. For sensitized individuals, the spring becomes a battle against these signs and symptoms. Consider that the exposed surface of each eye is approximately 200 mm2 and is constantly bombarded by particles. Depending on the season, these foreign bodies include pollen from trees, grasses, ragweed and other allergens. Dust, pet hair and dander, and mite and mold allergies can present an aggravation as well. One recent study found that nearly all of the homes it analyzed contained pet allergens, though less than half of them actually had pets.3 This indicates the mobility of allergens and their ability to accumulate in our environment.
Typically, clinical studies employ pollen counters on rooftops to measure the quantity and type of allergens in the air. However, it's not clear that the information gathered by a counter on a roof accurately reflects the pollen exposure of individuals on the ground. To more accurately record pollen exposure, some studies attempt to record data closer to the individual. Samplers can be placed in homes or yards, and small pollen counters can be worn on the body.4 Another technique is to track pollen levels indirectly via periodic assessment of signs and symptoms of individuals not taking an allergy treatment, using symptom severity as a measure of pollen severity.
While the ocular surface is protected by the nonspecific barrier of the tear film, some allergens will eventually penetrate this shield and trigger the IgE-mediated reaction. The exposed ocular surface can be thought of as the uppermost extremity of the respiratory system, with the ocular mucosa extending in one continuous membrane from the eye through the nasolacrimal ducts and the inferior turbinate to the nose, and then from the nose to the lungs. Thus, it's easy to see how conjunctivitis and rhinitis often coexist, and 70 percent of allergy patients note that their ocular symptoms are as bad as or worse than their nasal allergies.5 Even in patients diagnosed only with rhinitis, conjunctivitis can be present.
In a recent study that enrolled rhinitis patients, results from quality-of- life questionnaires revealed that more than 90 percent of the patients also experienced previously undiagnosed ocular allergy signs or symptoms at least one day per week.6 These studies give evidence of a rhinoconjunctivitis condition that's different from that of either conjunctivitis or rhinitis alone. An increased awareness of both the ocular and nasal allergic reaction can impact our quality of care.
Allergy's Prevalence
The prevalence of allergy varies. It's on the rise in most industrialized countries, and one study estimates the prevalence to be as high as 25 or 30 percent.7 The following factors may provide the key to understanding why.
• The hygiene hypothesis. This widely known theory states that reduced exposure to immune challenge such as infection and disease early in life results in the IgE-based defense mechanism reacting to other substances such as environmental pollens. This hypothesis is based on the idea of the immune system's balance of Th2 and Th1. The differentiation of less specialized Th0 cells into either Th2 or Th1 influences whether individuals will develop an allergic response. In the development of an allergic sensitivity, the production of Th2 is stimulated, while that of Th1 is suppressed. This shifts the balance of these two mediators in favor of Th2, which stimulates IgE production. This hypothesis holds that the Western lifestyle of increased personal hygiene is what brings about a shift toward Th2.8
This hypothesis is supported by studies showing that children with greater exposure to immune-challenging situations, such as daycare or exposure to farm animals, develop less atopy than children kept in more sterile environs.9 Additionally, children having infections of the upper respiratory tract have a decreased incidence of allergy.10
However, this theory can't explain why prevention of pertussis infection through vaccination lowers the occurrence of atopic disease, or why populations in unsanitary living situations in developing countries have a relatively high allergy prevalence. Clearly, there is much evidence in favor of this hypothesis, but the idea is still clouded by controversy, and conflicting research has poked holes in the theory. It appears that it alone cannot provide a complete explanation of allergy's initial causes.11
• The environment's impact. This is a crucial component in determining allergy, and to some degree is wrapped up with hygiene.
For example, a rural environment can be protective due to exposure to farm animals, providing early challenges to the Th1 immune system. Blackley even noted, "One very curious circumstance in connection with hay fever is that the persons who are most subjected to the action of pollen belong to a class which furnishes the fewest cases of the disorder, namely, the farming class." The opposite is true of urban life, in which pollutants can exacerbate the effects of pollen. Many studies have examined the effects of diesel exhaust on the immune system, finding that IgE production is elevated with exposure to diesel exhaust.12 In rhinoconjunctivitis, studies have linked symptoms to pollution levels, suggesting that the susceptibility to allergens could be increased by pollutants.13 In addition, the atmospheric changes caused by pollution may be changing the patterns of pollen release and increasing the duration of time it stays in the urban air.14
Considering these urban-rural contrasts, it appears Blackley may not have been far off in declaring allergy an "aristocratic disease." Even today, studies indicate that children of "academic" parents have a greater risk of developing allergy,15 perhaps due at least in part to these urban-rural contrasts, as well as factors such as the later average age of childbirth for couples with a high level of education.11
Beyond the larger classification of urban vs. rural environment, numerous factors in an individual's environment can increase or decrease the incidence of allergy or his exposure to allergens. These factors include: the number of children in a household (with fewer children meaning greater allergy risk);16 pets in the home; smoking; a sedentary and indoor lifestyle of children that increases their exposure to indoor allergens; and eating exotic foods and fatty acids.11,17 Some of these, such as fewer number of children, have been documented to increase susceptibility to allergy. Others, such as fatty acid intake and smoking, have been correlated with certain types of allergy. Data on some factors, such as pets in the home, remain inconclusive, with some research indicating increased allergy in these situations and other studies indicating the opposite.
• Heredity. In addition to environment, genetic influence in any disease pathology cannot be denied. It's long been evident that atopy is more likely to run in families. An excellent example is that of many allergic individuals from the northeastern United States who have moved to Arizona and surrounding desert areas. The arid Southwest provided an environment virtually free of the allergens that plagued them in their Eastern habitat. However, when they moved, they brought with them their house plants and pets, but most importantly, their genes. Perhaps they married other allergic individuals and then had children predisposed to atopy. This region now has a relatively high rate of allergy as compared to other areas.
Specific research in allergy has also supported involvement of genetic factors. Polymorphisms have been found at several gene loci that produce allergy-related molecules, further indicating the influence genetic factors have in determining allergy susceptibility.11 These factors include genes coding for cytokines, interleukins and TNF-alpha, which all influence IgE levels.
Treatment
While we no longer recommend sojourns by the seaside as Blackley did, we're able to treat the ocular allergic reaction more effectively. The topical approach continues to be best for topical disease such as rhinoconjunctivitis: A potent anti-allergy eyedrop for treatment of the ocular signs and symptoms forms the foundation of allergic conjunctivitis treatment. A drop can also help relieve nasal symptoms via drainage of the medication to the nose and/or by stopping the release of allergic mediators in the eye, impeding their drainage.18,19
Topical ocular treatment has proven superior to oral antihistamines for allergic conjunctivitis,20 as it allows for drug delivery directly to the eye. Additionally, oral antihistamines can actually dry the ocular surface,21 decreasing the barrier and flushing away of allergens provided by the tear film.
Researchers continue to study each potential contributing factor to the increasing prevalence of allergy. As Blackley put it in 1873, "I cannot but think that for those who have the courage to enter this path of investigation, as well as the patience and the perseverance necessary to pursue it steadily, there is a rich harvest of facts waiting to be gathered."
Dr. Abelson, an associate clinical professor of ophthalmology at Harvard Medical School and senior clinical scientist at Schepens Eye Research Institute, consults in ophthalmic pharmaceuticals. Ms. Fink is manager of medical communications at Ophthalmic Research Associates.
1. Blackley CH. Experimental Research on the Causes and Nature of Catarrhus Æstivus. Oxford: Oxford Historical Books 1988. First published: Great Britain: Baillière, Tindall and Cox 1873.
2. Von Hertzen LC, Haahtela T. Asthma and atopy—the price of affluence? Allergy 2004;59:2:124-37.
3. Arbes SJ, Cohn RD, Yin M, et al. Dog allergen and cat allergen in U.S. homes: Results from the National Survey of Lead and Allergens in Housing. J Allergy Clin Immunol 2004;114:1:111-7.
4. Frenz DA, Interpreting atmospheric pollen counts for use in clinical allergy: allergic symptomatology. Ann of Allergy Asthma & Immunol 2001;86:150.
5. Wuthrich B, Brignoli R, Canevascini M, Gerber M. Epidemiological survey in hay fever patients: Symptom prevalence and severity and influence on patient management. Schweiz Med Wochenschr 1998; 31:128:139-43.
6. Berger WE. Evaluation of the effect of an adjuvant therapy of olopatadine HCl ophthalmic solution 0.1% on quality of life of patients with allergic rhinitis using systemic and/or nasal therapy. Presented at American College of Allergy, Asthma and Immunology meeting, 2004; Boston.
7. Bielory L. Update on ocular allergy treatment. Expert Opin Pharmacother 2002;3:5:541-53.
8. Maggi E. The TH1/TH2 paradigm in allergy. Immunotechnology 1998; 3:4:233-44.
9. Von Ehrenstein OS, Von Mutius E, Illi S, et al. Reduced risk of hay fever and asthma among children of farmers. Clin Exp Allergy 2000;30:2:187-93.
10. Illi S, von Mutius E, Lau S, et al. Early childhood infectious diseases in the development of asthma up to school age—a birth cohort study. Allergy Clin Immunol Int 2001, 13: 99-106.
11. Ring J, Kramer U, Schafer T. Why are allergies increasing? Curr Opin Immunol 2001;13:6:701-8.
12. Heo Y, Saxon A, Hankinson O. Effect of diesel exhaust particles and their components on the allergen-specific IgE and IgG1 response in mice. Toxicology 2001;159:3:143-58.
13. Riediker M, Monn C, Koller T, et al. Air pollutants enhance rhinoconjunctivitis symptoms in pollen-allergic individuals. Ann of Allergy Asthma & Immunol 2001;87:311-318.
14. Behrendt H, Becker WM, Friedrichs KH. Interaction between aeroallergens and airborne particulate matter. Int Arch Allergy Immunol 1992;99:425-428.
15. Heinrich J, Popescu M, Wjst M, et al: Atopy in children and parental social class. Am J Public Health 1998;88:1319-1324.
16. Marshall AH, Owen V, Jones NS. More siblings, less hay fever. Clin Otolaryngol 2002;27:5:352-8.
17. Wakai K, Okamoto K, Tamakoshi A, et al. Seasonal allergic rhinoconjunctivitis and fatty acid intake: A cross-sectional study in Japan. Ann Epidemiol 2001;11:1:59-64.
18. Abelson MB, Turner RD. A randomized, double-blind, parallel-group comparison of olopatadine 0.1% ophthalmic solution versus placebo for controlling signs and symptoms of SAC and rhinoconjunctivitis. Clin Ther 2003; 25: 931-47.
19. Crampton HJ. A comparison of the clinical efficacy of a dose of ketotifen fumarate 0.025% versus placebo in inhibiting allergic rhinoconjunctivitis as induced by the CAC model. Clin Ther 2002:24:1800.
20. Abelson MB, Welch DL. An evaluation of onset and duration of action of Patanol compared to Claritin in acute allergic conjunctivitis in the CAC model. Acta Ophthalmol Scand Suppl 2000;230:60.
21. Ousler GW, Wilcox KA, Gupta G, Abelson MB. An evaluation of the ocular drying effects of two systemic antihistamines: loratadine and cetirizine hydrochloride. Ann of Allergy Asthma & Immunol 2004;93:5:460-4.