Refractive surgery patients can be the most demanding kind, since they're choosing to have the surgery done to enhance their way of life. To help keep them happy, and our outcomes good, we rely on research such as that offered at ARVO. At this year's meeting, you can learn how to screen patients, use the right procedure for a particular patient and manage complications confidently, all under one roof. Here are this year's refractive surgery highlights.
Complications Management/Screening
St. Petersburg, Fla., surgeon Stephen Updegraff may have found a new adverse event after LASIK. He calls the entity "reactive epithelium syndrome," and uncovered it in a retrospective review of LASIK patients with surgery dates between August of 2001 and August 2002.
Out of 1,750 eyes, 22 (1.25 percent) had intraoperative epithelial sloughing and postop reactive epithelium syndrome defined by dot and map epithelial findings at the slit lamp in the area of sloughing. There was no evidence of anterior basement membrane disease before surgery. All of the eyes lost two lines of best-corrected vision on postop day one. Over a three-week period, the topographic surface regularity index improved for all eyes, and all of them were undercorrected at three months. Two eyes with no evidence of dot epithelial changes at three months showed recurrence in the identical region of primary sloughing and undercorrection following a lift retreatment. All 22 eyes underwent superficial keratectomy and showed no reactive changes following a lift retreatment.
Though, in his abstract, Dr. Updegraff notes that more research is necessary in order to prevent this complication, a thorough history, including reactive epithelium syndrome in the differential diagnosis of irregular astigmatism, is important. 3840
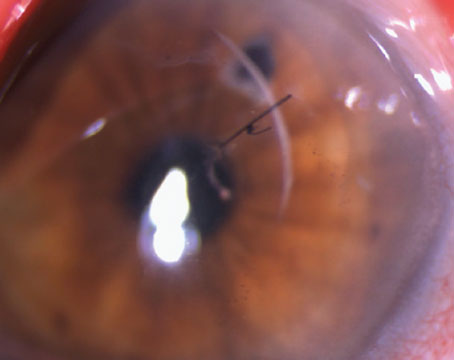
In another study of epithelial sloughing, researchers from Brazil and the University of Washington School of Medicine say that, despite a surgeon's best efforts, LASIK patients may have subtle subepithelial basement membrane dystrophy that can cause epithelial defects. They studied the corneal epithelia with electron microscopy and light microscopy with methylene blue staining in four cases of epithelial sloughing during LASIK, one case of PRK in the eye of a patient who had an epithelial defect during LASIK in the opposite eye, two cases of PRK in eyes that had clinical signs of epithelial basement membrane dystrophy and three normal PRK eyes.
In the eyes with sloughing during LASIK, as well as in the eye that had PRK associated with EBMD and epithelial sloughing in the fellow eye, a thick multilaminated basement membrane was attached to the basal epithelium. The researchers didn't find this membrane in the normal controls.
The researchers say that, in the eyes that sloughed, there was a smaller number of hemidesmosomes and the anchoring fibril system appeared abnormal. They add that the break leading to the epithelial sloughing occurred between the epithelial basement membrane and the anterior stroma in each case. They postulate that the sloughing eyes may have had epithelial basement membrane dystrophy that went undetected before surgery. 3840
Researchers at Rush-Presbyterian-St. Luke's Medical Center in Chicago say that the administration of prophylactic mitomycin-C during PRK or LASEK cases that are at a high risk for haze can help stave off haze formation.
The surgeons studied 47 eyes of 24 patients with an average preop spherical equivalent of -5.9 D who underwent PRK or LASEK with a Visx S2, S3 or a Technolas 217 laser. All eyes received a single intraoperative application of MMC 0.02% for two minutes after laser ablation.
Five eyes (11 percent) developed visually insignificant haze (an average haze score of 0.07 on a scale of 0 to 4) during a mean follow-up of 8.5 months. All eyes reepithelialized in a normal amount of time and none experienced toxicity. 2616
Researchers at Cedars Sinai Medical Center in Los Angeles performed a prospective study to find out if and when the fellow eye of a patient with unilateral keratoconus also develops the condition. They recruited 778 patients with keratoconus and 252 normal control eyes. One hundred and sixteen of the 778 (15 percent) had clinically unilateral keratoconus. The doctors then followed the patients for eight years.
Thirty out of 85 fellow eyes (35 percent) available for follow-up developed keratoconus, with 25 of them (83 percent) developing it within the first six years of the first eye's diagnosis. The eyes took a median of about 16.6 years to develop the condition. Fellow eyes with a higher inferior:superior ratio had a higher risk. Based on this data, researchers estimate that about half of the fellow eyes of keratocones will develop the condition within 16 years, and that videokeratography indices and patterns can be useful in predicting those at the highest risk. 1311
In some cases, increases in posterior corneal curvature observed after LASIK may not be a result of bulging in the central cornea, say researchers from Ohio State University. Rather, they postulate that it's due to backward swelling of the corneal periphery into the anterior chamber.
The researchers retrospectively studied the corneal behavior in 2,380 eyes of 1,255 myopic LASIK patients at the Hong Kong Sanatorium and Hospital. Patients underwent preop and six-month postop Orbscan (software version 2.0) exams. They found significant increases in central posterior elevation for corrections greater than -4 D. These increases, however, corresponded with significant peripheral decreases in posterior elevation of similar magnitudes. They say this is consistent with one of three hypothetical models for the bulging they had devised, namely inward peripheral movement of the posterior cornea, possibly due to swelling. They note that this would be consistent with a stable remodeling of the corneal shape due to a surgically-induced change in structure, as opposed to ectasia.2556
Instrument Variability
After a small retrospective study, researchers at Ohio State University advise surgeons to be wary when using the Orbscan II for pachymetry and posterior corneal measurements.
The scientists retrospectively studied 12 eyes of six LASIK patients in whom Orbscan II had taken pre- and one-month postop topographic images. They then reprocessed the device's slit images using version 3.0 of the software after disabling the unit's autoeditor in order to evaluate the performance of the system's edge tracker.
They also reprocessed a set of images with both software versions 2.0 and 3.0.
The researchers found that the slit images showed more corneal scatter postop, which caused the version 3.0 edge extraction algorithm to identify and begin tracking a low contrast posterior corneal edge outside of the pupil and then "get lost" when it crossed the pupil margin where contrast in the posterior edge sharply increased. For the case in which both versions were used, there was a greater than 40-µm difference in the central elevation of the extracted posterior surface that the paper's authors attribute to inaccurate tracking by the algorithm used in version 3.0. Ultimately, they say the posterior surface edge tracker in version 3.0 of the Orbscan software is not "tuned" to the higher scatter conditions in the post-LASIK cornea, which generate artificially "low" pachymetry values, as well as artificially "high" central elevation in the posterior cornea which might be misinterpreted as ectasia. The edge tracker has adequate performance in preoperative slit images, as well as in software version 2.0 which is, unfortunately, no longer available.2543
To get the most accurate scotopic reading of pupil dilation, researchers from the University of California, San Francisco, say that a couple of measurements taken at one sitting may not be enough.
In their study, two examiners measured the pupils in the right eyes of 69 patients under low light and dark conditions (T1), then repeated the measurements at one hour (T2) and 24 hours (T3). They calculated the limits of agreement for measurements between examiners (interexaminer) and between different time points measured by the same examiner (intraexaminer) as the mean difference between measurements ± 2 standard deviations.
At T1, there was a 98- and 93-percent chance of two different examiners producing readings within 0.5 mm under mesopic and scotopic conditions, respectively. The chances of finding a pupil difference greater than 0.5 mm over one hour was 14 percent and 15 percent for mesopic and scotopic conditions, respectively. When they got to the 24-hour visit, however, the chance of one examiner finding a difference greater than 0.5 mm than the last exam was 38 percent and 41 percent for mesopic and scotopic conditions. Because of this, the researchers say serial office measurements may be necessary to assess any possible risk-associated pupil size before performing any refractive surgery. 2595
Myopia
In a small-scale, prospective study, surgeons from the Netherlands found that uncorrected visual acuity and patient satisfaction are significantly better with LASEK than with PRK.
The researchers randomized 36 myopic eyes of 21 patients (range:
-1.75 D to -6.5 D) for LASEK or PRK with the relatively old Keracor 217 laser (from the now defunct Chiron). They measured the patients at the one day and three day and one-, three- and six-month visits.
Using a visual analog pain scale, the average pain perception at three days wasn't statistically significantly different between the procedures. At one month, patient satisfaction, as measured by a 100-mm visual analog scale, was 86 mm for LASEK and 60 mm for PRK. It increased to 96 mm and 76 mm for LASEK and PRK at three months, respectively. Translating the average LogMAR uncorrected acuity into Snellen equivalents, at one month it was between 20/20 and 20/25 for LASEK and between 20/25 and 20/32 for PRK. At three months, it had gotten a little closer to 20/20 for LASEK, but it stayed relatively static for PRK. And, at six months, the average acuity was actually better than 20/20 for the LASEK group, while it was better than 20/25 for the PRK group. As for uncorrected acuity, at six months it was better than 20/20 for the LASEK group, but between 20/20 and 20/25 for the PRK group. 2664
Tackling higher-order aberrations may be tougher than it looks, say doctors at Walter Reed Army Medical Center and Oregon's Pacific University.
The researchers used a Hartmann-Shack aberrometer to image 19 consecutive eyes undergoing LASIK enhancement over a 10-month period for undercorrection of simple myopia or myopia with astigmatism. They then compared the difference in total preop and one-month postop higher order wavefront aberrations from the initial procedure to the enhancements.
Both procedures increased the value of total higher-order aberrations as expressed by the RMS. For the initial procedure, RMS error went from 0.08 preop to 0.12 postop. Then, the RMS went from 0.12 pre-enhancement to 0.16 afterward. This amounted to a statistically equal amount of aberrations generated by both procedures.
The researchers say that, since their results suggest that enhancements generate as much higher-order aberrations in eyes as initial treatments, the limiting step in achieving aberration-free vision may involve factors beyond the technical limit of simply identifying and treating higher-order aberrations. They submit that corneal healing and varying corneal surface characteristics over time could be possible causes. 2610
Researchers at the Cleveland Clinic have drawn connections between particular higher-order aberrations and specific visual complaints.
They evaluated 105 eyes of 58 patients who had undergone LASIK, taking wavefront measurements with the Alcon LADARWave. They compared manifest, cycloplegic and topographical data to the wavefront measurements, and correlated any reported visual symptoms to higher-order aberrations at three different pupil diameters (5 mm, 7 mm and scotopic).
The analysis of visual symptoms showed a correlation of:
• double vision with total coma and with horizontal coma for the 5-mm and 7-mm pupils, respectively;
• starburst and total coma for the
7-mm pupil;
• glare with spherical aberration and with total aberrations, and;
• starburst with spherical aberrations in the scotopic pupil (which was negatively associated with double vision).
The researchers say that a wavefront device may be valuable in diagnosing symptomatic LASIK induced aberrations.2651
Researchers at New York University and Manhattan Eye Ear and Throat Hospital performed a prospective study of mild and moderate wavefront-guided myopic ablations with the WaveLight Allegretto Laser and were pleased with the results.
In the study, the surgeons performed 150 consecutive LASIK cases for myopic astigmatism, and followed the patients for three to seven months. The average refractive error before surgery was -3.8 D (-0.5 D to -6.75 D), and the average preoperative cylinder was -0.85 D (0 to -3.75 D).
In the 146 eyes available at three months, 92 percent saw 20/20, 57 percent saw 20/15 and 34 percent saw 20/10. One hundred percent were within ± 0.5 D of the refractive target, and there was no loss of best-corrected vision. The wavefront error, measured by a root mean squared value, decreased from 0.25 to 0.15, though four eyes saw their RMS errors increase. 2603
Hyperopia
In a small study, researchers at the University of Texas Southwestern Medical Center in Dallas found that visual results with the LADARVision laser system were statistically significantly better at six months in hyperopes than those produced by the Visx S2 or S3.
The surgeons studied 105 eyes with an average spherical equivalent error of +6 D for six months. All three lasers were comparable in terms of refractive stability and predictability, with the LADAR, S2 and S3 resulting in 88 percent, 88 percent and 86 percent of eyes within 1 D of the intended correction, respectively. The LADAR group had consistently better uncorrected visual acuities over the follow-up period, however. At six months, the researchers say the LADAR patients had statistically significantly better visual results than the S3 at both the 20/25 and the 20/20 level. The only statistically significant difference between LADAR and the S2 was at the 20/25 level. The study was independent and not sponsored by any laser maker.2619
LASEK appears to be safe and effective for hyperopia up to +4.5 D, according to a study from London.
In the study, surgeons treated 36 eyes with hyperopia (mean: +3.3 D, range: +1 to +6 D) and hyperopic astigmatism (cylinder range: -0.5 D to -3 D) with LASEK using an old Summit Apex Plus laser. To create the epithelial flap, they used 15% alcohol applied for 20 seconds.
The average follow-up was 8.5 months. At the last visit, of the 28 eyes with preop hyperopia less than 4.5 D, 72 percent were within 0.5 D of emmetropia and 90 percent were within 1 D. Predictability was significantly poorer for higher levels of correction. The surgeons were able to achieve an intact epithelial flap in 77 percent of the cases, and re-epithelialization occurred in all eyes by day four. There was significant ocular discomfort for the first day. In eyes with corrections greater than +3 D, there was a peripheral ring of corneal haze that didn't affect vision.2607
Researchers at Stanford say that, despite some regression, conductive keratoplasty appears to be safe and effective for low-to-moderate hyperopia after a two-year follow-up period.
In a small, prospective study, the surgeons performed CK on 25 eyes of 14 patients with errors ranging from +0.75 D to +2.75 D (mean: +1.58 D). At two years, 64 percent of the eyes saw 20/20 or better, and 95 percent saw 20/40 or better. The refraction was within 0.5 D of the target in 64 percent, and no eye lost two or more lines of best-corrected vision or had induced cylinder of 1 D or more.
At two years, the average manifest refraction was +0.48 D, a 29-percent regression from plano and a 43-percent regression from the initial overcorrection. The researchers point out, however, that the rate of regression appears to be low and is decreasing, measuring +0.024 D per month between years one and two. 2683
Odds and Ends
Researchers from Mexico City say the refractive surgeon's eye may be as good as a computerized eye tracker.
In a comparative study, the doctors looked at 280 LASIK eyes, half from surgery with the Technolas 217 with assisted ablation and half done manually with the Visx STAR S2.
Twenty-four and 31 of the eyes were off center with assisted ablation and manual ablation, respectively. Moderate decentrations were more frequent with the computer-assisted group, while mild ones were more frequent with the manual patients. Superior decentration was the most common variety. Most of the decentered eyes had moderate or severe myopia, but there were no decentered hyperopes. Overall, the researchers say that they couldn't find an advantage to using assisted ablation over manual. 2580
Researchers in the departments of ophthalmology and biostatistics at the Mayo Clinic in Rochester, Minn., have found that subbasal corneal nerves that are lost within the first year after LASIK return by two years, and stromal nerves return by three.
In the study, the doctors used confocal microscopy to examine 17 corneas of 11 patients who had undergone LASIK for myopia from -2 D to -11 D.
They say that the number of visible subbasal nerves per exam that initially decreased by 90 percent from 3.4 before LASIK returned to 1.5 at one year and to numbers that weren't significantly different from preop at two (2.5) and three (2.3) years. In Abstract 2680, Mayo researchers, some of whom participated in this LASIK study, also found similar results for subbasal nerves in PRK. After LASIK, the number of visible stromal nerves per exam decreased from 2.3 preop to 1.0 at one year and two years postop. By three years, the number of stromal nerves increased to 1.5, which wasn't significantly different from preop.2586
In a small prospective study from Italy, researchers have found that the accommodative lenses 1CU (HumanOptics, Erlangen, Germany) and the CrystaLens (C & C Vision, Aliso Viejo, Calif.) give a small but measurable amount of accommodation.
The surgeons implanted the CrystaLens in 14 eyes of 10 patients, and the 1CU in 10 eyes of seven patients. The preop best-corrected acuity ranged from 20/63 to 20/32.
At one month, they measured accommodation by adding a negative sphere to the far-distance correction until 4/5 letters of the smallest detectable line were properly identified. Masked observers also measured anterior-chamber depth and the amplitude of the scleral-ciliary process angle with ultrasound during accommodation and in a relaxed state. The acuity at one month ranged between 20/25 and 20/16 for distance. The accommodative and ultrasound results appear in Table 1.252
Dr. Hannush is attending surgeon at the Cornea Service of Wills Eye Hospital, and assistant professor in the Department of Ophthalmology at Jefferson Medical College.