Though epithelial basement membrane dystrophy isn’t difficult to diagnose, deciding on the proper course of treatment for the cases that warrant it can be a challenge. In this article, cornea experts review their approaches to managing these cases, and how the type and severity of symptoms play into their decision-making process.
When to Treat
Most patients with epithelial basement membrane dystrophy don’t experience pain or visual symptoms and don’t require treatment, but some cases will require your intervention. Symptoms range from corneal erosion to pain and diplopia, surgeons say.
 |
“Epithelial basement membrane dystrophy can manifest with a few different symptoms,” says Toronto’s Raymond Stein, MD. “It can interfere with vision when the abnormal epithelial basement membrane appears over the pupil. The other, probably more common, symptom is that patients can have recurrent corneal erosions in which the epithelial cells slough off from the cornea, causing severe pain.”
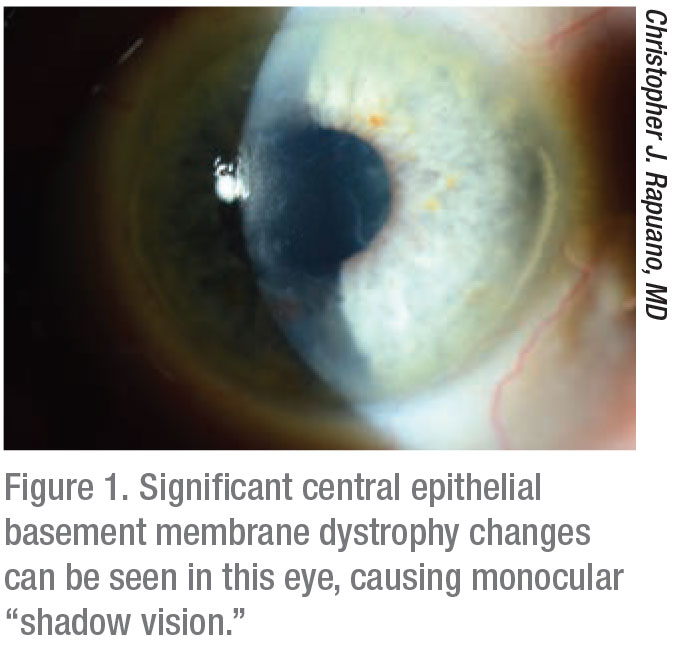
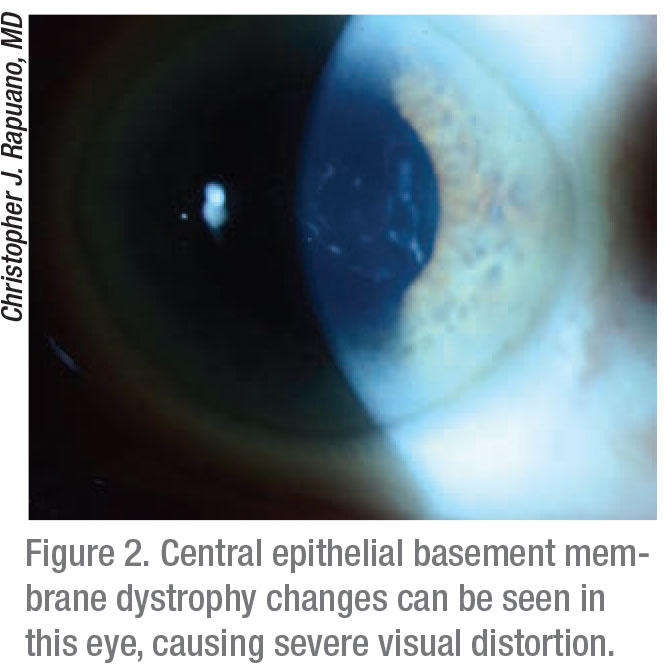
Christopher J. Rapuano, MD, Chief of Wills Eye Hospital Cornea Service in Philadelphia, agrees. “Patients with these two main symptoms will often complain of poor vision or ‘double vision,’” he notes. “The irregularities can cause what I call ‘shadow vision,’ because patients see an image with a shadow next to it, as opposed to two equally distinct images. In addition to visual symptoms, this condition can also cause recurrent erosions. Pain from irregular loose epithelium typically presents at nighttime or upon awakening in the morning. This is because epithelial basement membrane dystrophy causes the epithelial layer to not adhere properly. It can be painful for just a few seconds after waking up or it can cause a big scratch on the cornea that can be painful for days.”
Michael B. Raizman, MD, who is in practice in Boston, says there is a third reason to treat. “I also treat when the basement membrane dystrophy affects my ability to calculate a lens implant power prior to surgery,” he adds.
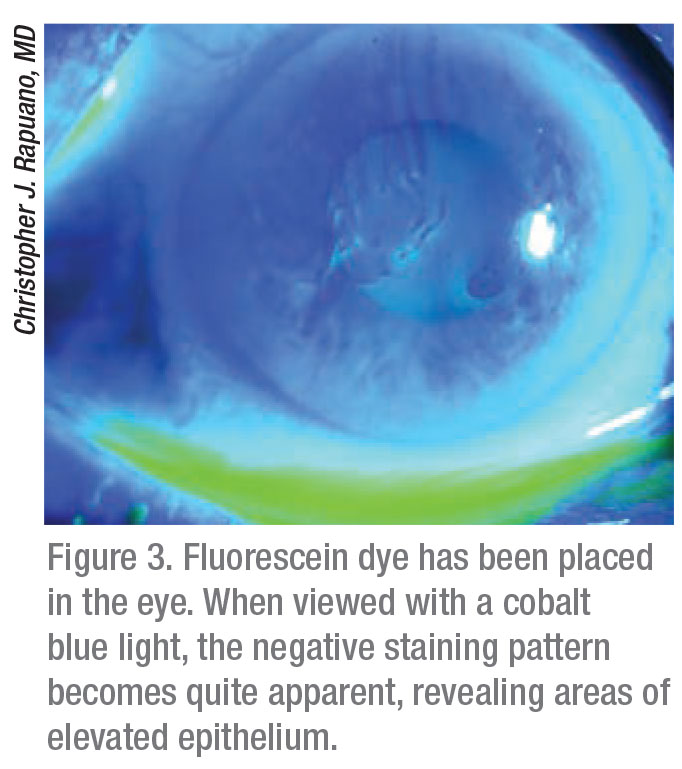
Dr. Rapuano adds that many patients have asymptomatic epithelial basement membrane dystrophy in the corneal periphery. “If they don’t have painful episodes, you don’t have to do anything about it,” he says. “But, once they have visual symptoms or recurrent erosions, then we’ve got to go look for it. One way to do this is to instill fluorescein and then look for negative staining, where you put the fluorescein in and look with the cobalt blue light to see where the mild lumpy bumpiness is lifting the epithelium up off the cornea, and the yellow dye is kind of pulled off those areas. It basically highlights the epithelial basement membrane dystrophy problem. I would suggest that if you suspect an epithelial basement membrane dystrophy problem, but you really can’t see it, put fluorescein in and look for negative staining. If there’s negative staining in the visual axis, then it could be causing visual symptoms. If there’s negative staining in a patient with recurrent erosions, then that might be an area where they had a recent erosion,” he says.
How to Treat
Visual complaints can be treated medically or by removing the affected part of the epithelium.
 |
Dr. Rapuano agrees. “If the vision is irregular from a ‘lumpy bumpy’ cornea right in the center, you can try lubrication, which doesn’t usually do very much,” he says. “Basically, you need to remove it. You can do a simple epithelial debridement, where you just scrape off all of the loose epithelium. This usually works well. Sometimes, a microscopic irregular basement membrane is left underneath the epithelium, and if you want to remove that, you can use a diamond burr polisher. Usually, I remove the epithelium, and then I sand down the cornea gently for five to 10 seconds. This removes any part of the microscopic basement membrane that’s there. Then, I treat the patient with a bandage soft contact lens, antibiotic drops, lubrication, ice packs for the pain and pain pills—which may include narcotics. Then, I’ll see patients the next day and then a couple of days later. Usually I’ll take the contact lens out on day four or five, and the epithelial defect will be healed. But then they still use ointment every night for three to six months, just to let the epithelium tack down.”
Dr. Raizman uses either a round blade, a spatula, a diamond burr or an excimer laser to remove the epithelium down to Bowman’s layer. “If I’m removing the epithelium to improve the quality of vision or to create a smoother cornea to allow more accurate keratometry readings prior to surgery, I prefer to use a round metal blade, and I scrape off the epithelium without affecting Bowman’s layer,” he explains. “I generally remove between 5 and 7 mm of the epithelium centrally. I remove a little bit more when I’m doing this for lens calculations because the mid-periphery can affect my keratometry readings. If I’m doing it simply to let the patient see better, then, depending on the size of his or her pupil, sometimes I can get away with removing just 4 or 5 mm centrally. Additionally, the basement membrane dystrophy is occasionally associated with Salzmann’s nodules, which are in the mid-periphery or even the periphery, and despite the nodules being out of the visual axis, they can disturb the tear film and may affect the vision or the keratometry measurement. So, I sometimes have to also remove nodules that are more peripheral. I also remove those with the blade.”
 |
For patients with recurrent corneal erosions, Dr. Stein says he tries medical management first. “Typically, we use hypertonic salt solutions,” he explains. “For example, I use a medication called Muro 128 (Bausch + Lomb), which comes in both drop and ointment forms. It draws water out of the epithelium and decreases epithelial swelling, which results in a decrease in corneal erosions. That’s the mainstay of treatment.”
Unfortunately, many patients have recurrent corneal erosions that start to interfere with their daily activities. “It’s one thing to have an erosion once every six months, but if the erosions are occurring a number of times each month, and the pain is persistent for 15 to 30 minutes or longer, then the patients need additional treatment, which is typically superficial keratectomy,” says Dr. Stein. “In the operating room, with a lid speculum in place, under topical anesthesia, I use a Merocel spear and just touch the epithelium. If it’s loose, it comes off very easily. If the epithelium is normal, it’s quite adherent. We basically take off the epithelium that’s really loose, and we’ll often use a diamond polisher to polish the surface of Bowman’s layer. This very quick procedure is followed by instilling an antibiotic drop and a non-steroidal drop and then fitting the patient with a bandage soft contact lens, which we keep in place typically for a few weeks. And with that treatment, there’s a very high probability of permanent success. We’ve found that about 85 percent of patients don’t have recurrent erosions after that. The remaining 15 percent could still have some erosions, but, in most cases, they’re less severe and less frequent.”
For recurrent corneal erosions, Dr. Raizman also tries a simple debridement first. “However, in my experience, that is only effective about 50 percent of the time,” he says. “I like anterior stromal puncture for erosions if the recurrent erosions are out of the visual axis. I prefer not to do puncture in the visual axis because the puncture creates scars that can be permanent. While those scars aren’t often visually significant, they can be. Because the results are unpredictable, if there are erosions in the visual axis, I would prefer to use a diamond burr or an excimer laser to treat those. I think the excimer laser is safer because there is a more controlled removal of Bowman’s layer and a more uniform removal. The downside is that the laser is more expensive, and insurance usually won’t pay for it, so patients have to pay out of pocket; there’s a cost to the surgeon to use the laser that has to be passed on to the patient.
“The diamond burr is inexpensive, simple, and easy to use in the office setting,” Dr Raizman continues. “However, if the burr is used too aggressively, you can remove more of Bowman’s layer in some areas than others or even remove some stroma, and that can create irregular astigmatism and affect the patient’s vision sometimes. But I should emphasize the burr is quite practical, and it’s not hard to use it safely, so it’s often a good choice for surgeons who don’t have access to the excimer laser or for patients who can’t afford it.”
Dr. Raizman adds that while debridement is about 50-percent effective in these cases, the excimer laser is 90 to 95 percent effective for resolving the recurrent erosions with a single treatment. “I don’t personally have enough experience with the diamond burr, but from the medical literature, it’s probably equally as effective as the excimer laser,” he says.
For recurrent erosions, Dr. Rapuano prefers a diamond burr treatment. “You can perform excimer laser phototherapeutic keratectomy, but I don’t usually do that,” he says. “I usually use the diamond burr, which I find to be as effective as the excimer laser and much faster, easier to schedule, and less expensive. However, if you’ve got some scarring on the anterior part of the cornea due to multiple erosions, then you can do excimer laser phototherapeutic keratectomy. In that case, I strip the epithelium off and then, instead of using a diamond burr to polish it, I use the excimer laser. The nice thing about the excimer is that it will polish a big area pretty uniformly.”
 |
Pearls
According to Dr. Stein, refractive surgeons should always be looking for epithelial basement membrane dystrophy. Most patients with this condition are asymptomatic, but it can have a significant impact on the outcome of refractive surgery. “If patients have epithelial basement membrane dystrophy, they are far better off having PRK than LASIK,” he says. “If they have loose epithelium that goes undetected, and they have LASIK, the epithelium can slough off during the procedure, and the healing can be very delayed. So, it’s important to rule out cases of epithelial basement membrane dystrophy in patients who are interested in laser vision correction. Often, the best way is the use of fluorescein dye and a blue light using the slit lamp to look for abnormal breakup in focal areas of the cornea. That’s very suggestive of epithelial basement membrane dystrophy.” He adds that all LASIK surgeons need to ask about patients’ past history of corneal erosions.
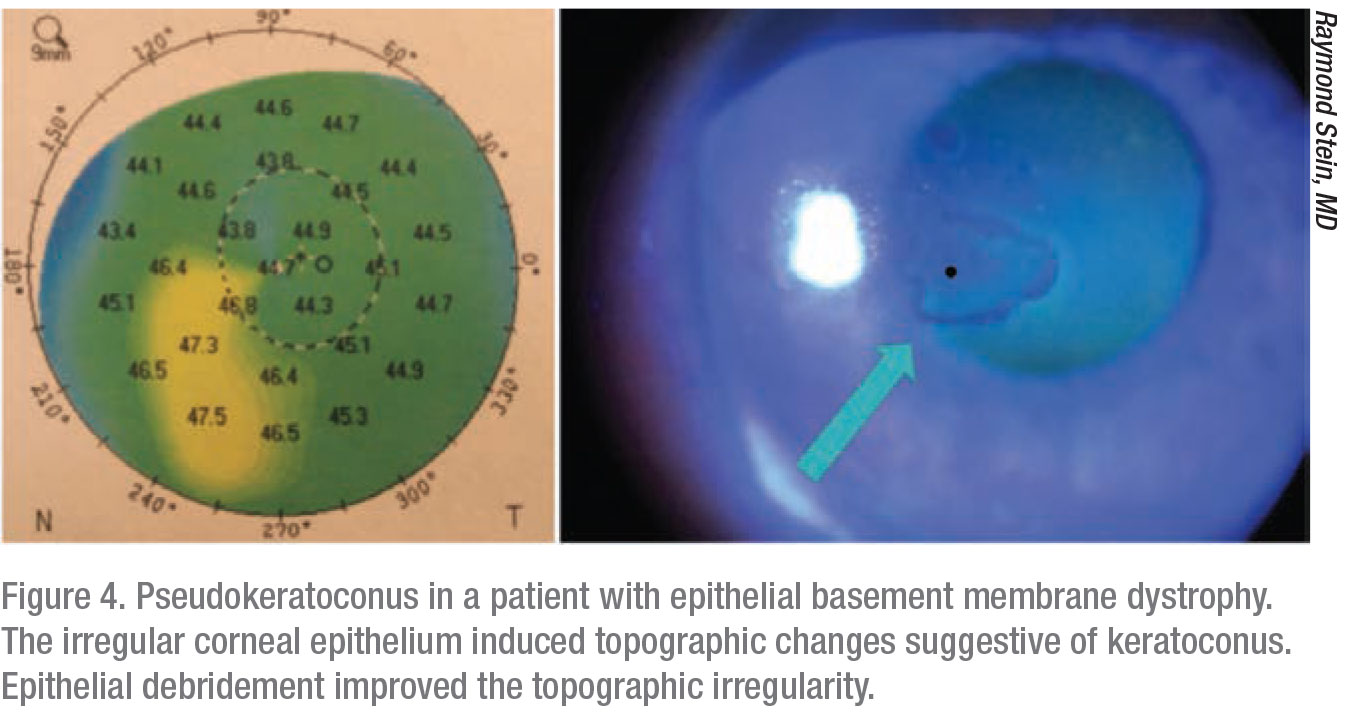
Epithelial basement membrane dystrophy can also mimic other conditions. “These patients can have false ectasia or pseudokeratoconus, and it’s very important that the surgeon identify that it’s not keratoconus or pellucid marginal degeneration but is in fact epithelial basement membrane dystrophy,” says Dr. Stein, “and they don’t require corneal cross-linking. The rest of the cornea is totally normal, and these patients don’t need corneal stiffening.”
Dr. Raizman adds that he is referred a lot of patients with anterior basement membrane dystrophy for treatment prior to cataract surgery because the keratometry readings are a little bit irregular. “These patients often say that they don’t really mind wearing glasses after their surgery,” he says. “They’re not necessarily looking for the best uncorrected vision after cataract surgery. And in that case, if the vision isn’t significantly affected by the basement membrane dystrophy, there’s not really a reason to do a debridement prior to your IOL calculations. But for patients who want the best possible uncorrected vision and are looking for a specific refractive outcome, those patients should have a debridement prior to measuring the cornea. My point is that it’s not mandatory, so it doesn’t have to be done on every patient. It depends on the patient’s postop needs.” REVIEW
None of the physicians quoted in the article have financial interest in any of the products or procedures mentioned.



