Presentation
A 57-year-old woman presented to the Wills Eye Oculoplastic and Orbital Surgery Service complaining of recurrent swelling of her right lower lid. The swelling began one month after she had undergone a four-lid blepharoplasty at an outside institution. Prior to her presentation at Wills, the patient had been treated with oral amoxicillin and ciprofloxacin with no improvement in symptoms. Two brief courses of oral corticosteroids moderately improved the swelling. However, her symptoms returned immediately after stopping the steroids. Otolaryngology consultation revealed no evidence of sinusitis. The patient also had undergone root canal surgery for a presumed dental source of a presumed infection, with no postoperative improvement. The patient denied any decreased vision, foreign body sensation or pain.
Medical History
The patient's past medical and past ocular histories were otherwise unremarkable. Her family and social histories were non-contributory.
Examination
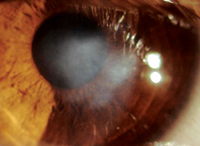
The visual acuity was 20/20 OD and 20/20 OS. Her pupils were round, equal, briskly reactive, and without a relative afferent pupillary defect. Extraocular motility and confrontational visual fields were full in both eyes. Intraocular pressures were within normal range. Examination of the right lower eyelid revealed a non-tender, mobile, erythematous, firm nodule (See Figure 1). Otherwise the external exam, slit lamp and dilated funduscopic exams were unremarkable OU.

Diagnosis, Workup and Treatment
The patient's recent eyelid surgery increased suspicion for an inflammatory or infectious etiology. CT scan of the orbits was performed and revealed preseptal inflammation of the periorbital soft tissue. According to the initial surgeon, no sutures, alloplasts or fillers were used in the lower eyelids, making foreign body granuloma an unlikely diagnosis. Because of the indolent presentation and partial response to corticosteroids, atypical infection was suspected. The patient was taken to the operating room for an explorative biopsy and debridement of the mass. The orbital fat pads and inferior oblique muscle were grossly normal. The malar fat pad had firm, granular tissue that was debrided and sent for bacterial, fungal and acid fast stains and cultures. The pathological examination revealed chronic granulomatous inflammation (See Figure 2a) with multiple acid-fast bacteria (See Figure 2b). Cultures grew Mycobacterium chelonae. The patient was taken back to the operating room for further skin debridement. A peripherally inserted central catheter (PICC) line was placed, and the patient was treated with IV cefoxitan and amikacin for two months. She was also given oral doxycycline and clarithromycin for six months. Her right lower lid edema and erythema resolved completely.
Discussion
Three rapidly growing atypical mycobacteria are known to cause infections of periorbital tissue: Mycobacterium chelonae; Mycobacterium fortuitum and Mycobacterium smegmatis. A review of patients in the Wills Eye Oculoplastic and Orbital Surgery Service revealed five cases of periocular infection with atypical mycobacteria, four of which followed routine eyelid surgery. While uncommon, these infections can be difficult to diagnose and treat. Routine laboratory evaluations often do not include acid-fast staining, and the diagnosis may be missed. Furthermore, laboratories must keep the culture media for at least one week to allow these organisms to grow. 
Atypical mycobacterial infections tend to be subacute, presenting several weeks after surgery. Erythema and tenderness may be mild, and discharge, if present, may only be minimal. The lesions are generally firm and nodular, and may be multiple. The lesions may appear similar to chalazia, or the patient may not show any signs of inflammation. Patients often have a history of recent surgery, immunosuppression, implantation of a foreign material, or nasolacrimal duct obstruction. In a series of eight patients, infection was linked to the use of a surgical skin-marking solution, but most infections do not have a clear source.
Treatment of these atypical mycobacterial infections should involve excision of the lesion for tissue culture and debridement, as well as a protracted course of antibiotic therapy. Clarithromycin is often the drug of choice, but other antibiotic regimens may be used depending on culture results and sensitivities.
A high level of suspicion for atypical mycobacterial infections is of paramount importance in making this diagnosis. Otherwise, these infections may be missed as the patient's symptoms grow worse, leading to unnecessary morbidity. In any patient presenting several weeks after surgery or trauma with a firm nodular mass and varying degrees of inflammation, the surgeon should specify to the pathologist the need for special stains and culture media for these organisms in addition to routine cultures and stains. The specimen should be processed appropriately, and the culture media should be observed for an extended period of time. Once the diagnosis is made, the patient must undergo a long course of antibiotics as well as surgical removal and debridement. If the correct diagnosis is made, a complete resolution of symptoms can often be achieved.
Dr. Rosenthal would like to thank
Chang WJ, Tse DT, Rosa RH Jr., Miller D. Periocular atypical mycobacterial infections. Ophthalmology 1999;106:86-90.
Safranek TJ, et al. Mycobacterium chelonae wound infections after plastic surgery employing contaminated gentian violet skin-marking solution. N Engl J Med 1987;317:197-201.
Rootman DS, Insler MS,
Smith RE, Salz JJ, Moors R, Silverstein D, Lewis W. Mycobacterium chelonei and orbital granuloma after tear duct probing. Am J Ophthalmol 1980;89:139-41.
Mauriello JA Jr. Atypical Mycobacterial Study Group. Atypical Mycobacterial infection of the periocular region after periocular and facial surgery. Ophthal Plast Reconstr Surg 2003;19:182-8.