
Presentation
An 81-year-old female presented to her local ophthalmologist with a four to six week history of binocular, horizontal diplopia. She denied any recent changes in her visual acuity or any pain. In addition, she denied any headache, jaw claudication, fevers, chills, weight loss or myalgias. She was diagnosed at that time with a possible left cranial nerve VI palsy and was sent to a neurologist, who performed an MRI/MRA of the head and orbits (See Figure 1). The scans were read as consistent with thyroid eye disease, and the patient was referred to the Wills Eye Institute for further evaluation and management.
Medical History
The patient's medical problems included hypertension and atrial fibrillation. In addition, there was a remote history of a left Bell's palsy and shingles. She denied any history of diabetes, thyroid dysfunction or cancer. Her medications included warfarin, furosemide, ramipril, aspirin, glucosamine and a multivitamin. Her family history was noncontributory, and she denied smoking. On review of systems, she denied any constitutional symptoms or any history of cancer. Notably, she denied ever having a chest x-ray or mammogram.
Examination
Her examination in the Wills Eye Institute's Oculoplastic and Orbital Surgery Service revealed a best corrected visual acuity of 20/20 in the right eye and 20/50 in the left eye. Her confrontation visual fields and pupillary exam were normal. Anterior segment examination was only significant for bilateral pseudophakia. The dilated funduscopic exam was normal. Notably, she was found to have increased resistance to retropulsion in both eyes, and a Hertel's exophthalmometry reading of 16 mm in the right eye and 21 mm in the left eye with a base of 93 mm. There was no lid retraction, lid lag or lagophthalmos. Her ocular movements are shown below (See Figure 2).

Diagnosis and Workup
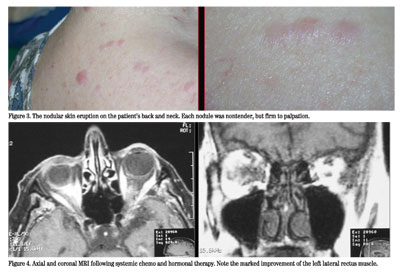
The patient presented with a restrictive strabismus, primarily causing an abduction deficit in the left eye, but also with poor infraduction. MRI evidence of bilateral orbital infiltration was present, inconsistent with
Discussion
Metastatic cancer to the orbit is relatively rare, ranging between 1 and 13 percent of orbital tumors. Conversely, uveal metastases are estimated to occur about 10 times more frequently. It is estimated that approximately 2 to 3 percent of patients with systemic cancer will have metastases to the orbit. In 19 to 42 percent of patients with metastatic disease to the orbit, the orbital findings are the initial manifestation of cancer. The most common primary tumor is breast carcinoma, followed by prostate and lung cancer. Other primary tumors include colon, kidney, skin melanoma, thyroid, liver, pancreas, choroidal melanoma and others. Women are more likely to have cancer metastasize to the orbit because of the higher likelihood of having breast cancer. Curiously, 20 percent of metastatic breast disease to the orbit is bilateral, as occurred in our patient. In addition, adults more commonly have cancer metastasize to the orbit, though occasionally neuroblastoma will do so in children.
Symptoms usually develop relatively rapidly over the course of a few weeks to months and most commonly include blurry vision, diplopia, blepharoptosis, and less frequently, pain around the eye. Examination will often reveal proptosis, resistance to retropulsion, blepharoptosis or a visible or palpable orbital mass. Enophthalmos may be seen in certain patients, especially those with scirrhous breast carcinoma, secondary to fibrosis and contraction of orbital contents. The diagnosis is made through a combination of history, physical exam, orbital imaging and biopsy. Both MRI and CT scanning can be useful in the diagnosis. Most orbital metastases involve the orbital soft tissues, and therefore MRI is typically more helpful than CT. However, in cases of prostate cancer, CT imaging may be more helpful, given the tendency of prostate cancer to invade bone. Ultimately, orbital biopsy is necessary to make the definitive diagnosis.
Treatment of orbital metastases varies depending on the patient. Well-circumscribed tumors within the anterior orbit may be completely excised without further ocular treatment. In other cases, systemic chemotherapy and/or hormonal therapy may adequately control the tumor, as was the case with our patient. Orbital radiation may be helpful in certain cases where other treatments fail to control symptoms. Unfortunately, because of the high doses necessary, radiation retinopathy, keratopathy and optic neuropathy may occur. Prognosis is poor in general, though dependent on the nature of the primary tumor and the extent of systemic metastases. Patients with metastatic carcinoid or breast cancer have a better overall prognosis than those with metastatic lung cancer.
Dr. Fenton is a second-year resident. He would like to thank Dr. Jurij Bilyk for his assistance with this case.



