
Presentation
A 22-year-old woman presented to the Wills Eye emergency room with the complaint of blurred vision in the right eye. The patient stated that she awoke three days earlier and noted that "part of her vision was missing" in the right eye. Over the following two days, this visual loss progressively worsened. She denied any pain, redness, or flashes or floaters. She had no history of ocular trauma or prior ocular surgery.
Medical History
Her past medical history was significant for a remote hernia repair as an infant. She smoked one pack of cigarettes per day, used alcohol occasionally, and never used intravenous drugs. She had no known drug allergies and was not taking any medications.
Examination
In the emergency room, uncorrected visual acuity was counting fingers at 2 feet in the right eye (no improvement with pinhole) and 20/20 in the left. Pupils were brisk, with no relative afferent pupillary defect. Extraocular motility and confrontational visual fields were full in both eyes. Intraocular pressures by applanation tonometry were 16 mmHg in both eyes. On slit-lamp examination, the anterior segment was within normal limits bilaterally. Her dilated fundus examination was normal in the left eye; however, the right was significant for extensive macular exudation and edema, as well as an elevated pink lesion in the inferotemporal periphery of the retina (See Figures 1 and 2). Figure 2. Color montage of the right fundus demonstrates a pink vascular lesion in the inferotemporal periphery.
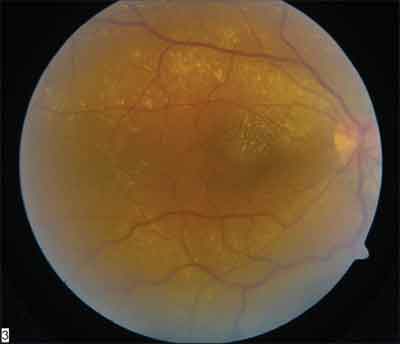
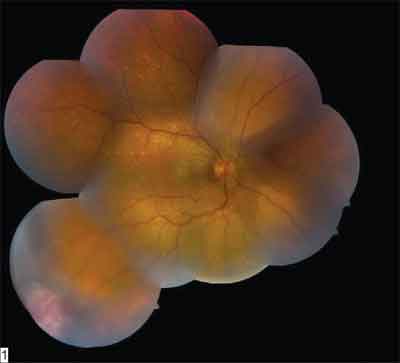
Figure 1. Color fundus photo of the right eye demonstrates extensive intraretinal exudation and macular edema.
Both images: Drs. Carol and Jerry Shields
Diagnosis and Workup
The patient's clinical findings of a pink-yellow vascular mass in the peripheral retina, associated with intraretinal exudates, macular edema, and the absence of tortuous, dilated feeder vessels are consistent with the diagnosis of a vasoproliferative tumor of the retina (VPTR). This diagnosis is one of exclusion. Specifically, one must rule out capillary hemangioma associated with von Hippel-Lindau syndrome (check for the VHL gene mutation). Other entities to consider in the differential include Coats' disease, retinal or choroidal metastases, choroidal melanoma with retinal infiltration, and peripheral exudative hemorrhagic chorioretinopathy.
Discussion
Vasoproliferative tumor of the retina is a relatively new term, coined in 1995 by Dr. Carol Shields and associates.1 VPTR is also known in the literature as hemangioma-like tumor, angiomatous mass, peripheral retinal telangiectasia and presumed acquired retinal hemangioma.
Presenting symptoms of VPTR vary from vision loss, floaters or photophobia to a blind painful eye (secondary to neovascular glaucoma). Some patients are asymptomatic. Clinical findings include the presence of a vascular, pink-yellow mass in the peripheral retina associated with intraretinal exudates, RPE hyperplasia adjacent to the tumor, secondary exudative retinal detachment, vitreous cells, vitreous hemorrhage and/or macular edema. Of note, a dilated, tortuous feeder vessel is not prominent with VPTR, in contrast to feeder vessels seen with capillary hemangiomas of the von Hippel-Lindau syndrome.
VPTR may be classified as primary/idiopathic (74 percent of tumors) or secondary (26 percent).1 In primary VPTR, no preexisting ocular disease is present. Secondary VPTR has been seen in association with several ocular conditions, including pars planitis, retinitis pigmentosa, toxoplasmic retinitis, toxocariasis, retinochoroidal coloboma, sickle cell retinopathy, retinopathy of prematurity, longstanding retinal detachment and Waardenburg's syndrome.
VPTR may manifest as a solitary tumor, multiple tumors or a diffuse tumor (defined as basal dimension >10 mm with an ill-defined multinodular pattern). Primary VPTR are usually solitary, while secondary VPTR are more likely to be multiple. Most (78 percent) VPTR are located in the inferior, inferotemporal or temporal retina, and 88 percent are within 6 mm of the ora serrata.
Additional studies to consider include fluorescein angiography (IVFA) and ultrasonography. Fluorescein angiography is often technically difficult secondary to the peripheral location of the lesions. The early phase of IVFA demonstrates rapid filling of the tumor through non- or minimally dilated feeder vessels. The venous phase shows diffuse leakage and staining of the tumor mass, which continues into the late phase. A-scan ultrasonography demonstrates high internal reflectivity, while B-scan shows an acoustic solidity without choroidal excavation.
Histologic examination of VPTR reveals retina thickened by diffuse gliosis, with cystic areas filled with pink exudates. Dilated, ectatic vessels with hyalinized vessel walls have been observed, as have preretinal neovascular membranes.2
The natural history of VPTR is highly variable. Some tumors demonstrate either cessation of growth or very slow progression, while others rapidly progress to tractional retinal detachment.
No firm guidelines exist for the treatment of VPTR. Most physicians agree to treat complications associated with visual loss. Some treat earlier because smaller lesions may be more easily treated. In addition, treating earlier may salvage visual acuity. One series found that patients with longstanding macular edema did not regain visual acuity after regression of the tumor and exudates.3
Treatment options include cryotherapy, plaque radiotherapy, laser and photodynamic therapy (PDT). Cryotherapy is best suited for small lesions (<3 mm in thickness). When used to treat larger lesions, increased exudation may result, leading to exudative retinal detachment. For larger lesions (>3 mm thick), plaque radiotherapy is preferred. Laser and PDT, while less commonly used, represent additional treatment modalities discussed in the literature.4
Dr. Young is a second-year resident at Wills Eye Hospital. She would like to thank the oncology service at Wills for their contribution to this case.
1. Shields CL, Shields JA, Barrett J, De Potter P. Vasoproliferative tumors of the ocular fundus. Classification and clinical manifestations in 103 patients. Arch Ophthalmol 1995;113:615-23.
2. Smeets MH, Mooy CM, Baarsma GS, Mertens DE, Van Meurs JC. Histopathology of a vasoproliferative tumor of the ocular fundus. Retina 2003;18:470-2.
3. Heimann H, Bornfeld N, Vij O, Coupland SE, Bechrakis NE, Kellner U, Foerster MH. Vasoproliferative tumours of the retina. Br J Ophthalmol. 2000 Oct;84(10):1162-9.
4. Barbezetto IA, Smith RT. Vasoproliferative tumor of the retina treated with PDT. Retina 2003;23:565-7.



