 |
A 41-year-old African-American male presented to the Wills Eye Emergency Department complaining of “a blood clot coming out of my left eye.” He reported episodic pain and redness in his left eye for approximately four months with less severe prior episodes in his right eye. Two days prior to presentation, he noted the abrupt onset of intense pain, decreased vision and photophobia in his left eye with no preceding trauma.
Medical History
The patient had a history of treatment for peripheral corneal thinning in the left eye. He had no history of eye surgery or contact lens wear. Review of systems was positive for debilitating joint aches, particularly in his knees that were worse in the morning. An extensive rheumatologic evaluation was notable only for a mildly positive anti-nuclear antigen (ANA 1:40). No definitive diagnosis was given by his treating rheumatologist. His medications included doxycycline, prednisone, methotrexate and infliximab. He denied tobacco or alcohol use. He had no family history of rheumatologic disease.
Examination
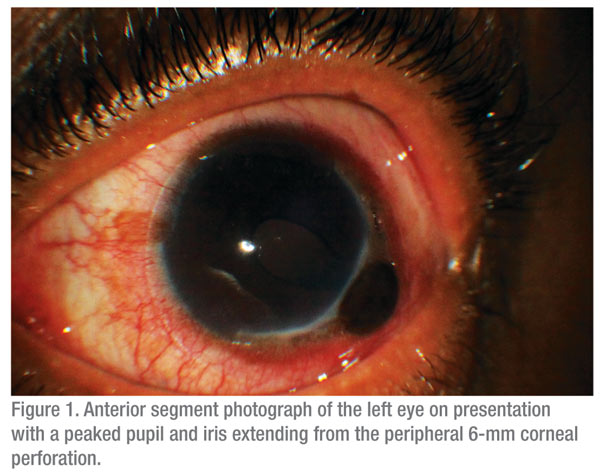
Visual acuity without correction was 20/20 in the right eye and 20/400 in the left eye. The patient was noted to have a saddle-nose deformity. On slit-lamp examination, the patient had two areas of peripheral stromal thinning of approximately 10 to 15 percent in the right eye. The examination of the right eye was otherwise unremarkable. In the left eye, there was 3+ conjunctival injection with peaking of the pupil and iris extending from a peripheral 6-mm corneal perforation (See Figure 1). The surrounding cornea had significant stromal thinning with an epithelial defect.
What is your differential diagnosis? What further workup would you pursue?



