 |
Background
Our patient, a 31-year old male, has struggled with various ailments since birth. His past is riddled with various doctor visits and numerous hospital stays battling his many afflictions: common variable immunodeficiency; craniosynostosis; seizure disorder; obstructive sleep apnea; and mild mental retardation. This time he was at the hospital for a fever where he also exhibited an altered mental status.
After some investigation and a thorough physical exam, the patient was found to have lower extremity cellulitis with compounded septic shock. Appropriately, his doctors started aggressive fluid resuscitation, pressors, broad spectrum antibiotics and intravenous immunoglobulins and his condition slowly improved.
The fifth day at the hospital brought forth complications. He developed conjunctival injection in his left eye. At first glance, the ocular irritation seemed to have developed secondarily to the oxygen face mask. However, upon further examination, the patient was found to have also developed HSV stomatitis.
 |
 |
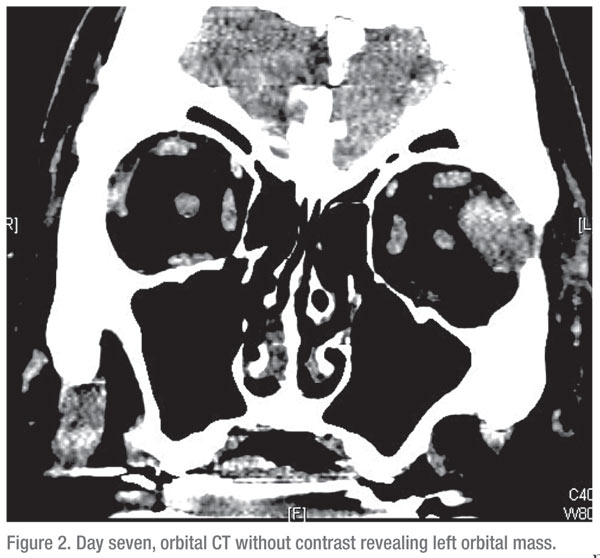
Orbital imaging in these patients may reveal a high density mass on CT.
Magnetic resonance imaging typically demonstrates hypointense lesions on
T1 and T2 sequences with marginal enhancement with gadolinium acutely
due to the presence of deoxy-hemoglobin, hyperintensity with a bright
peripheral ring increasing centripetally subacutely due to the presence
of methemoglobin, hypointensity chronically due to hemosiderin, and
ferritin formation.3
Transfer of Care
Transfer of Care
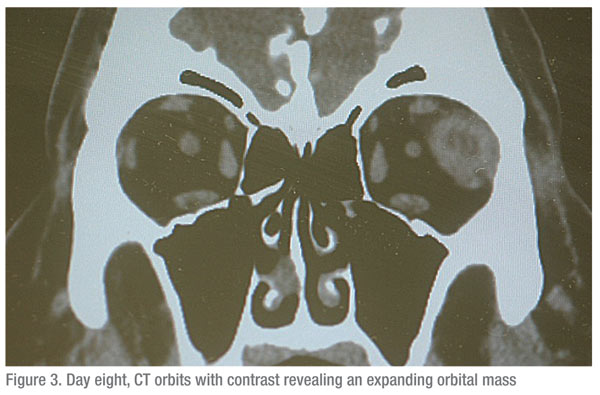
With his other co-morbidities under control, the patient was transferred to our institution on the ninth day to manage his expanding orbital mass. Our exam revealed restriction of the lateral gaze for the left eye with temporal chemosis. His visual acuity was 20/40 for the right eye and 20/30 for the left eye with no relative afferent pupillary defects noted. His intraocular pressure was within normal limits and a dilated fundoscopic evaluation did not show any significant pathology.
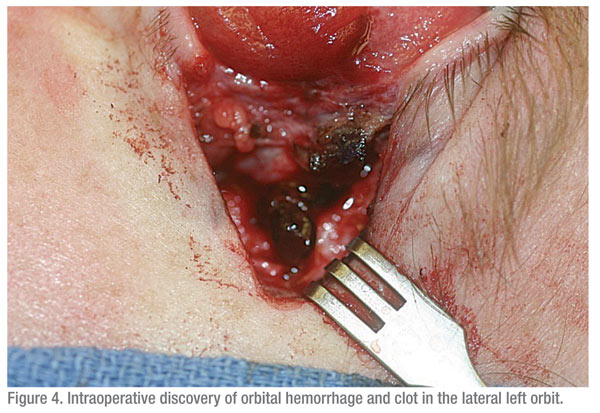 |
Initially, an orbital abscess, orbital lymphoma, or viral myositis was suspected in the context of his immunodeficiency, recent cellulitis, and sepsis. The neuroradiologist was consulted and stated that the CT images Were consistent with an orbital abscess given the interval increase in size, enhancement and patient’s history. A left orbitotomy was performed and, unexpectedly, a hemorrhage and a clot was discovered in the lateral orbit (See Figure 4).
Diagnosis and Treatment
Interestingly, pathological examination of the clot revealed no evidence
of infection or malignancy, including negative fungal, viral and
bacterial cultures. Postoperatively, the patient had significant
reduction in proptosis and was transferred back to his primary hospital
on the sixth postoperative day for the completion of his care. He was
diagnosed with a spontaneous atraumatic orbital hemorrhage.
Potential for Vision Loss
Potential for Vision Loss
While orbital hemorrhaging may look unsightly, most cases do not require surgical management and can be treated conservatively, with most resolving within four to six weeks. Due to the limited space of the orbit, however, hemorrhage can lead to the compression of the optic nerve or increased intraocular pressure. Both of these complications are serious and can lead to permanent vision loss. Therefore, clinicians should always assess for rapid or progressive vision loss as the first step in management where an emergent surgical decompression procedure may be necessary to save a patient’s vision.
The authors are affiliated with the department of ophthalmology and visual sciences at the University of Illinois at Chicago College of Medicine. Contact Dr. Aakalu at 1855 W. Taylor St., MC 648, Chicago, Ill. 60611. Phone: (312) 996-9120; fax: (312) 996-1934; or
vaakalu@uic.edu.
1. Sullivan TJ, Wright JE. Non-traumatic orbital haemorrhage. Clin Experiment Ophthalmol 2000;28:26-31.
2. Corl K, Jeffrey Hofmann R, Sutton E. Non-traumatic orbital hemorrhage. J Emerg Med 2010;38(3):378-80. Epub 2008 Mar 19.
3. Provenzale J. CT and MR imaging of acute cranial trauma. Emerg Radiol 2007;14:1-12



