The past several years have brought a rush of clinical insights into the management of glaucoma, such as the concept of central corneal thickness and its effect on intraocular pressure readings, and the patient's "OHTS" risk for developing glaucoma. Muncie, Ind., ophthalmologist and software developer Michael Hodkin observed all these new findings and thought they might be easier to put to use in everyday practice if he had a computer remember them all for him.
With this thought in mind, he developed an inexpensive glaucoma program for Palm-compatible devices and Pocket PCs called EyeOP. Here's a look at what the program can do.
Inside EyeOP
Dr. Hodkin says the idea behind the program is for it to be a cover sheet that can accompany a patient's record and make it easier for a clinician to manage new glaucoma patients and suspects. He cautions that it's not an electronic medical-records program, nor is it designed to track progression of the disease. It's made to be a digital way to jog one's memory so clinicians don't need to refer to back issues of journals and texts frequently throughout their day.
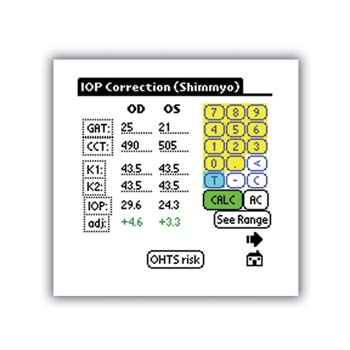 |
| Figure 1. EyeOP will adjust the IOP based on central corneal thickness. |
Some of its main features include the following:
• Risk factors and screening. When you first see a patient, EyeOP gives you a checklist of probable and possible glaucoma risk factors that you can check off if they're present. Probable factors include elevated IOP and large cup-to-disk ratio, while possible ones include a family history of glaucoma and diabetes.
The medical screening menu allows you to check off systemic, ocular or medical factors, such as arrhythmias, that might be contraindications for certain treatment options.
Help screens are available throughout the program. Clicking on any dotted text or a question mark, such as one next to arrhythmias, will explain more about that concept or aspect of the program.
• Intraocular pressure index. The IOP Correction section of the program is a calculator you can use to "correct" the Goldmann applanation tonometry reading for a given central corneal thickness. To use this feature, you enter in both eyes' IOP readings and corneal thicknesses, and the program will use a published nomogram1 to calculate a more accurate IOP. (See Figure 1.) Dr. Hodkin is quick to point out that, although no definitive formula or nomogram has been established for this calculation, all of the published nomograms are very close to one another, including the one EyeOP is based on.
A handy offshoot of the IOP correction page is the IOP range that the program calculates. This range takes the form of a conversion table of "true" IOPs for a patient's given central corneal thickness for a range of measured IOPs, from 5 mmHg to 40 mmHg. It can be saved or printed out and kept in the patient's chart. Then, when the patient returns and his IOP has changed, you don't have to repeat the IOP correction calculation to get an adjusted IOP, you just refer to the table.
There is also a button titled "OHTS Risk" on the IOP Correction page. Clicking on this button will give you the percentage risk for an ocular hypertensive eye to develop glaucoma, based on the corneal thickness and IOP, according to the criteria established by the Ocular Hypertension Treatment Study.
• IOP Target. This screen is based on the findings of a panel of glaucoma experts.2 It's a calculator that will help establish a target pressure, given the initial untreated, unadjusted IOP and your classification of the patient's glaucoma. You choose the glaucoma classification from a drop-down list of definitions. The program gives you an absolute IOP reduction target in mmHg as well as a percentage.
Since Dr. Hodkin wanted to base his program on published data, the target page uses the unadjusted IOP. "The concept of target IOPs was established prior to the current, in-vogue use of CCT correction factors," he explains. "Ideally, adjusted IOPs should be used for determining target IOPs, but the literature has yet to catch-up to this.
"I presented this so clinicians have a guide to go by," says Dr. Hodkin. "So they can at least have a firm number in their minds as they follow up with the patient. If the patient's IOP drops, the doctor will be able to see if he's reached his goal."
• Medical reference. This is a handheld database of all the key information about the 48 drugs currently used to treat glaucoma, sorted by brand name or class. The data provided include the dosing frequency, efficacy, ocular and systemic side effects and the average cost per month to a patient. Dr. Hodkin says the last bit of information can be helpful when trying to find the most cost-effective drug for a patient with limited means. Depending on how well the program is received, Dr. Hodkin plans to post updates for new glaucoma drugs on his website (palm4eyes.com) as they're approved.
"This is my favorite part of the program," says Dr. Hodkin. "Some pocket drug references are great for looking up general medicines, but I've found them lacking in the world of eyes. I took information from several different texts to get all the medical information for the glaucoma drugs."
EyeOP runs on all Palm-compatible and Pocket-PC devices. You can get more information about it, download a demo copy or buy the full version (for $29) at palm4eyes.com.
1. Shimmyo M, Ross AJ, Moy A, Mostafavi R. Intraocular pressure, Goldmann applanation tension, corneal thickness, and corneal curvature in Caucasians, Asians, Hispanics, and African Americans. Am J Ophthalmol 2003 Oct;136:4:603-13.
2. Workgroup on Evidence-based Treatment Recommendations for Glaucoma. Evidence-based management of glaucoma: Recommendations of an expert panel. Glaucoma: Disease Management Guide. In: 2004 Physicians' Desk Reference, 1st ed. Montvale, N.J.: Thomson 2003.



