Diagnosing patients’ dry eye, and following its progress after you initiate therapy, can sometimes be an involved process if you choose to use staining or other tests. However,
Elizabeth Yeu, MD, a cornea/anterior segment and refractive surgery subspecialist from the
Baylor College of Medicine in Houston, says you can use certain features of your corneal topographer to help diagnose these patients and monitor the effectiveness of your treatments. Here’s her advice on how to do it.
The Ring’s the Thing
“Even though there are different topographers you can use to help diagnose ocular surface disease, most of them have a particular type of view that’s important,” explains Dr. Yeu. “This key view is the keratometry image. This view is important because you don’t use it just for the K values, but also for the mires’ appearance, as well.”
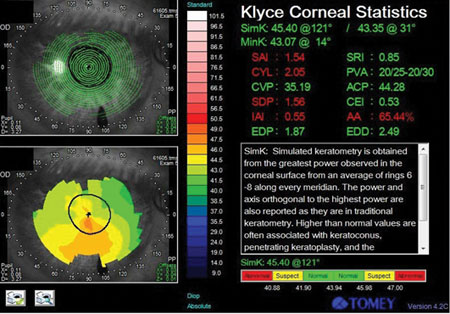 |
“For someone with a very dry eye, there can be missing mires or missing keratometry data,” she continues. For instance, when you’re looking at the SimK values on an elevation map or other views, there will be points that are completely missing. And, on the keratometry view, instead of seeing smooth rings the mires will be warped or ‘squiggly,’ and a very dry eye can even give a forme fruste keratoconus appearance due to the irregular tear film. Also, instead of appearing bright or sharp, the mires may be dull.”
The other type of patient the keratometry view will pick up is someone whose eye has been overly filled with drops. “If someone has been inundated with drops,” warns Dr. Yeu, “and you’re bringing up simulated K values, the machine may pull up irregular astigmatism that’s not actually there.”
Over time, the clinician can also use topography to get an idea how well treatment is working in a less-invasive way. “You can see how well the patient responds to treatment,” says Dr. Yeu. “This can be helpful in those patients with dry eye in whom you don’t want to use a lot of diagnostic drops in the clinic due to the possible toxicity of drops such as lissamine green and fluorescein. If you can evaluate these patients using just topography, especially in follow-up, that’s helpful.”
As a supplement to the topographer’s keratometry and simulated K data, surgeons who use an anterior segment optical coherence tomographer can also make use of the device to check the ocular surface. “An anterior segment OCT can help detect conjunctival chalasis, and can also give data on tear-film height and area,” says Dr. Yeu. “If the tear-film height is low, that suggests an aqueous-deficient condition. And the tear-film area can help you delineate between a normal surface and an abnormal one.”
The Use of Indices
Some topographers have indices that compare certain aspects of the cornea to each other to yield a number that tells a user how normal or abnormal the corneal shape is, usually with an eye toward catching keratoconus. Dr. Yeu says, however, that these same indices can also be helpful in diagnosing an ocular surface condition, not just an irregular corneal shape. “Clinically, these indices, such as the surface regularity index and the surface asymmetry index on the Tomey unit, can be useful. To use them for the ocular surface, image the patient before you instill drops. An in-house study we did demonstrated that an SRI >0.15 is highly sensitive and specific for identifying dry-eye patients. Also, the severity of the ocular surface disease appears to correlate well with larger SRI values. Topography and surface regularity indices can be helpful, non-contact methods for tracking your management of the patient’s ocular surface.”
Limitations
Dr. Yeu notes that using your topographer doesn’t obviate the need for further tests. “These methods don’t seem to be as helpful for evaporative dry eye, unless the eye is severely evaporative and can’t maintain any tear film,” she says. “This is because when we perform topography, the patient blinks and we capture the image; so as long as the patient can maintain the tear film for two to three seconds, you’ll capture a clean surface. This also highlights the discrepancy that can exist between signs and symptoms.” However, though topography is more suited to identify an aqueous deficiency problem, Dr. Yeu says that the device will catch an evaporative condition that’s gotten bad enough to cause corneal epitheliopathy. “You always have to ask the patient about his symptoms, as well,” she says.



