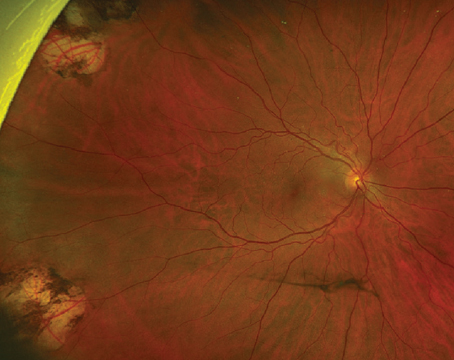
An estimated 8 million individuals in the United States have age-related macular degeneration; among them approximately 1 million have the neovascular form of the disease (See Figure 1).1 AMD remains the leading cause of blindness among individuals age 55 and older in industrialized countries,2 though its pathogenesis remains poorly understood.
Age is clearly a risk factor, and family history probably is as well. Several large population-based studies have evaluated the association of other systemic risk factors with AMD.3,4,5 Although smoking, systemic hypertension, atherosclerosis, diabetes, obesity, alcohol consumption and UV light exposure have all been postulated as possible risk factors in the incidence and progression of AMD, no consistent relationship has been demonstrated across multiple epidemiological studies.6
Statins
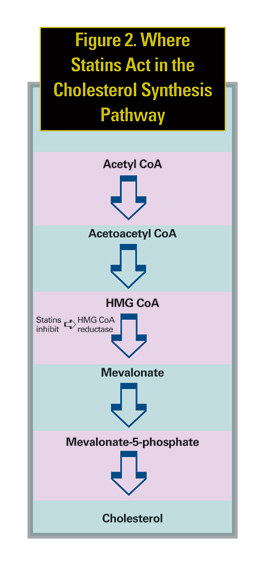
Recently, several studies have suggested that cholesterol-lowering drugs, particularly statins, protect against AMD.7,8 Statins are a class of lipid-lowering medications that inhibit 3-hydroxy-3-methyglutaryl coenzyme A (HMG CoA) reductase, the enzyme that catalyzes the rate-limiting step in cholesterol synthesis (See Figure 2). In addition to their lipid-lowering mechanism, statins also may possess anti-inflammatory properties, and if they alter AMD risk, it could be via this mechanism.9
Numerous prospective studies have shown that statins reduce cardiovascular mortality.10,11 Currently, statins are the most frequently used medication for the treatment of hypercholesterolemia and the prevention of atherosclerosis and coronary heart disease. Statins are generally well-tolerated, and the most common side effects associated with these medications are nausea, upset stomach, constipation or diarrhea.12 More rare but potentially severe side effects that have been reported are elevated liver enzymes, myopathy with possible rhabdomyolysis and polyneuropathy.
Atherosclerosis, which is associated with cardiovascular disease, has also long been postulated to be a risk factor for AMD. In the Rotterdam study, investigators found that individuals with carotid plaques were five times as likely to have advanced AMD as those without carotid plaques.13 Although other epidemiological studies have not confirmed such a relationship,3,4,5 there is still much interest in evaluating the potential association between AMD and atherosclerosis.
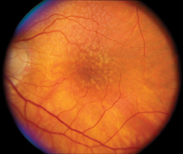
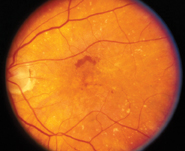
Figure 1A and B. Fundus photographs of (A) non-neovascular age-related macular degeneration with large drusen and (B) neovascular age-related macular degeneration with subretinal hemorrhage and fluid.
Histopathology of Bruch's Membrane
Histological study of human eyes with grossly normal maculas revealed a linear, age-related accumulation of cholesterol within Bruch's membrane.14 In addition, cholesterol was found to accumulate in both choroidal arteries and drusen. These findings are similar to those seen in atherosclerosis, a disease of the vascular system in which extracellular cholesterol deposition also increases with aging. It has been hypothesized that hypercholesterolemia, oxidative damage and endothelial dysfunction, which is postulated to occur in atherosclerosis, may contribute to the development and progression of AMD as well.14 If this hypothesis is true, then statins may have a role in the prevention of AMD.
Studies Showing A Protective Effect
In a recent retrospective consecutive case series of 326 patients at the San Francisco Veterans Affairs Hospital, among the 104 individuals who had choroidal neovascularization, 21 (20 percent) used statins compared with 77 (38 percent) of non-neovascular AMD subjects without GA (hazard ratio=0.51, P=0.01).8 Eligible subjects were age 60 or older with AMD, and 309 (95 percent) participants were men. The authors concluded that therapy with statins is associated with decreased rates of CNV in subjects with AMD.
Another study also found a beneficial effect of statins.7 The authors performed a cross-sectional study of 379 elderly individuals, of whom 27 (7 percent) reported taking statins. Although the total number of participants taking statins was small, the authors found a statistically significant reduction in the odds of having AMD of 86 percent in those taking the lipid-lowering medicine.
 |
These three studies are limited by their retrospective nature and small number of participants. Retrospective studies may have inherent bias that influences patient inclusion, management, and follow-up. Moreover, a relatively small sample size limits one's opportunity to recognize infrequent events, or to provide ample power to distinguish outcomes. Two of the studies were conducted at a Veterans Affairs Medical Center and contained a predominantly male population, which makes the results less applicable to the general population. Even with these limitations, however, these studies suggest that statins may have a protective effect on the development of AMD.
Studies Demonstrating No Effect
Researchers examined the association between statins and the five-year incidence of AMD among participants in the Beaver Dam Eye Study, a large, population-based cohort study.16 Between 1993 and 1995, 118 participants were using statins. While controlling for age and sex, statin use was not found to be associated with the five-year incidence of early AMD (odds ratio=1.12 [95-percent confidence interval 0.47-2.67], P=0.80), progression of AMD (OR=1.22 [95-percent CI 0.54-2.76], P=0.63), or incidence of late AMD (OR=0.41 [95-percent CI 0.12-1.45], P=0.23).
In the Rotterdam study, a large population-based cohort study of 4,822 individuals, 457 patients used cholesterol-lowering drugs. In this study, there was no association between exposure to statins and the risk of AMD.17 In addition, in the Blue Mountains Eye Study, another similar population-based cohort study, there was no protective effect of statins on the incidence of AMD.18
| Table 1. Studies Evaluating the Statins/ AMD Association | ||
| Study | Number of subjects Using Statins | Association Between Statins and AMD |
| Retrospective Authors: Wilson et al. | 21 | Risk of Neovascular AMD Hazard ratio = 0.51 95% CI = 0.31 – 0.86 |
| Retrospective Authors: Hall et al. | 27 | Risk of AMD Odds ratio = 0.14 95% CI = 0.02 – 0.83 |
| Retrospective, case control Authors: McGwin et al. | 37 | Risk of AMD Odds ratio = 0.30 95% CI = 0.21 – 0.45 |
| Prospective, population-based Authors: Klein et al. | 118 | 5-year incidence of AMD Odds ratio = 1.12 95% CI = 0.47 – 2.67 |
| Prospective, population-based Authors: van Leeuwen et al. | 457 | Incidence of AMD Hazard ratio = 1.0 95% CI = 0.7 – 1.5 |
| Prospective, population-based Authors: van Leeuwen et al. | 260 | Incidence of early AMD Odds ratio = 1.0 95% CI = 0.6 – 1.6 |
| 95% CI = 95% Confidence Interval | ||
| Adapted from references 7,8,15,16,17,19 | ||
Pooled findings from all three population-based cohort studies (Beaver Dam Eye Study [n=3,012], Rotterdam Study [n=3,434], and Blue Mountains Eye Study [n=2,203]) assessed the association between medication use with the incidence of early AMD.19 The investigators specifically chose not to evaluate the incidence of advanced AMD because they believed the relative infrequency of late AMD would not provide enough power to perform such an analysis. Rather, they concentrated on the incidence of early AMD, defined as the presence of intermediate soft distinct drusen (> 63 µm) with retinal pigment epithelial depigmentation or hyperpigmentation, soft indistinct drusen (> 125 µm), or reticular drusen.
Among the pooled cohort, 260 (3 percent) subjects used lipid-lowering agents. While adjusting for age, gender, and time of follow-up, there was no association; the odds ratio between lipid-lowering agents and incidence of early AMD was 0.9 (95-percent CI 0.6 to 1.5). If the authors adjusted for body mass index, systolic and diastolic blood pressure, smoking, and total and high-density lipoprotein cholesterol, the OR was 1.0 (95 percent CI 0.6 to 1.6). The pooled data from these three large, population-based studies therefore found no association between lipid-lowering drugs and incidence of early AMD.
Neither these individual large, prospective cohort studies nor the pooled data from these studies revealed an association between statin use and the development of AMD. Although these studies do not contain the possible inherent biases that are found in retrospective studies, they do have limitations. These studies are limited by their relatively short follow-up period (five-year follow-up in the Beaver Dam and Blue Mountains Eye Studies, and 6.5-year follow-up in the Rotterdam Study). AMD is a disease of aging, and a longer duration of follow-up is needed to allow for the detection of more incident cases.
In addition, these studies did not look at duration of statin use, nor did they evaluate the medication dosage. This type of information may be helpful in determining whether lipid-lowering agents have an effect on AMD. Despite these limitations, these three population-based studies contain a large number of participants, and therefore are more adequately powered to find a statistically significant association between statins and AMD incidence.
The association between the use of cholesterol-lowering drugs and the incidence of AMD remains unclear. Retrospective studies have suggested a protective effect of statins, yet prospective, population-based cohort studies have failed to reveal an association between statins and the development of AMD (See Table 1).
Although well-tolerated, statins do have the potential to cause harmful side effects and should not be prescribed unless medically indicated. The medical literature certainly shows a statistical benefit of statin use for the prevention of atherosclerosis and coronary heart disease, but the ophthalmic literature does not provide definitive proof that statins retard the incidence of AMD.
A randomized, controlled clinical trial would be the ideal method for investigating the association between statins and AMD. However, such a trial would require a Herculean effort since the sample size needed would be extremely large, confounding factors would have to be accounted for, and the follow-up period would need to be long enough to include a sufficient number of incident cases of AMD.
In summary, the relationship between cholesterol-lowering agents and AMD remains unsettled. There is no definitive evidence to suggest that statins are protective against the incidence of AMD. For now, ophthalmologists should consider the Age-Related Eye Disease Study supplementation of antioxidants and zinc to be the only proven preventive treatment for reducing the risk of advanced AMD for patients with intermediate or advanced AMD.20 Statins should not be included in our armamentarium until more conclusive evidence is obtained.
The authors have no proprietary interest in any of the products mentioned in this article. Dr. Do is a fellow in medical and surgical retina at the Wilmer Eye Institute, Johns Hopkins University School of Medicine. She is supported by the Heed Ophthalmic Foundation Clinician-Scientist Award and the Ronald G. Michels Fellowship Foundation Award. Dr. Schachat is the Karl Hagen Professor of Ophthalmology at Wilmer. Contact him at aschachat@jhmi.edu.
1. Age-Related Eye Disease Study Research Group. Potential public health impact of age-related eye disease study results: AREDS report No. 11. Arch Ophthalmol 2003;121:1621-1624.
2. Klein R, Wang Q, et al. The relationship of age-related maculopathy, cataract, and glaucoma to visual acuity. Invest Ophthalmol Vis Sci 1995;36:182-191.
3. Klein R, Klein BE, Tomany SC, et al. Ten-year incidence and progression of age-related maculopathy: The Beaver Dam Eye Study. Ophthalmology 2002;109:1767-1779.
4. van Leeuwen R, Klaver CC, et al. The risk and natural course of age-related maculopathy: Follow-up at 6 and a half years in the Rotterdam study. Arch Ophthalmol 2003;121:519-526.
5. Wang JJ, Foran S, Smith W, Mitchell P. Risk of age-related macular degeneration in eyes with macular drusen or hyperpigmentation: The Blue Mountains Eye study cohort. Arch Ophthalmol 2003;121:658-663.
6. Klein R, Peto T, Bird A, Vannewkirk MR. The epidemiology of age-related macular degeneration. Am J Ophthalmol 2004;137:486-495.
7. Hall NF, Gale CR, Syddall H, et al. Risk of macular degeneration in users of statins: cross sectional study. BMJ 2001;323:375-376.
8. Wilson HL, Schwartz DM, et al. Statin and aspirin therapy are associated with decreased rates of choroidal neovascularization among patients with age-related macular degeneration. Am J Ophthalmol 2004;137:615-624.
9. Albert MA, Danielson E, et al. Effect of statin therapy on C-reactive protein levels: The pravastatin inflammation/CRP evaluation (PRINCE): A randomized trial and cohort study. JAMA 2001;286:64-70.
10. Randomized trial of cholesterol lowering in 4,444 patients with coronary heart disease: The Scandinavian Simvastatin Survival Study (4S). Lancet 1994;344:1383-1389.
11. Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: A randomized placebo-controlled trial. Lancet 2002;360:7-22.
12. www.pdr.net
13. Vingerling JR, Dielemans I, et al. Age-related macular degeneration is associated with atherosclerosis. The Rotterdam study. Am J Ophthalmol 1995;142:404-409.
14. Curcio CA, Millican CL, et al. Accumulation of cholesterol with age in human bruch's membrane. Invest Ophthalmol Vis Sci 2001;42:265-274.
15. McGwin G, Owsley C, Curcio CA, Crain RJ. The association between statin use and age related maculopathy. Br J Ophthalmol 2003;87:1121-1125.
16. Klein R, Klein BEK, Tomany SC, Danforth LG, Cruickshanks KJ. Relation of statin use to the 5-year incidence and progression of age-related maculopathy. Arch Ophthalmol 2003;121:1151-1155.
17. van Leeuwen R, Vingerling JR, Hofman A, de Jong PTVM, Stricker BHCh. Cholesterol lowering drugs and risk of age-related maculopathy: prospective cohort study with cumulative exposure measurement. BMJ 2003;326:255-266.
18. Klein R, Klein BEK. Do statins prevent age-related macular degeneration. Am J Ophthalmol 2004;137:747-749.
van Leeuwen R, Tomany SC, et al. Is medication useassociated with the incidence of early age-related maculopathy: Pooled findings from 3 continents. Ophthalmology 2004;111:1169-1175.
20. Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS Report No. 8. Arch Ophthalmol 2001;119:1417-1436.