Partly, this is a problem of casting too wide a net—if one screens for all diabetic retinopathy, one is likely to find a lot of diabetic retinopathy that does not need intervention, ironically increasing the burden on the same physicians it is intended to be assisting. A notable exception has been for retinopathy of prematurity screening. This application has worked for three simple reasons: 1) the remote screening is highly effective at identifying a treatment intervention time point; 2) the disease is self-limited in that it will either spontaneously resolve or result in retinal detachment and blindness within a 15-week time frame; and, 3) all neonatal intensive care units (NICUs) are required to perform screening in order to maintain accreditation, removing most of the financial uncertainty. These three components give us great insight into greater application of telemedicine in ophthalmology. First, let us review the ROP scenario.
ROP Telemedicine
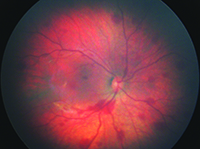
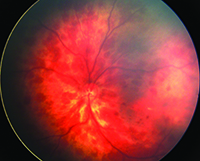
|
Universal Screening of Newborns
Pediatric vitreoretinal surgery physicians have been looking to expand upon the success of telemedicine screening for ROP. One potential opportunity is universal screening of newborn infants. In China, Brazil, Hungary and Spain, universal screening has been practiced in single-hospital settings for up to seven years.
| The telemedicine experience in pediatric retinal diseases has been successful because it has avoided the pitfalls of casting too wide a net. |
Other strategies that are being employed are assessment of axial length, refraction, optical coherence studies of the macula, and, potentially, intraocular pressure assessment in the near future. While the NEST program is currently being evaluated as a prospective study with longitudinal follow-up with pediatric ophthalmology/retina specialists, it is evident from early data that commercialization and widespread adoption will be offered in the future.
The telemedicine experience in pediatric retinal diseases has been successful because it has avoided the pitfalls of casting too wide a net. Instead, we have identified niche markets with well-defined intervention points that are easily identified using the technology. These markets, whether in ROP or congenital ocular pathology, have a limited timeframe in which therapy is beneficial, but can result in life-long benefit. Therefore, the societal and patient benefit is large from these screening programs. As ophthalmologists, we need to continue to define very narrow ranges of targeted telemedicine screening that will offer immediate relief and benefit, while still maintaining economic feasibility. REVIEW
Dr. Moshfeghi is an associate professor of ophthalmology at Stanford University School of Medicine where he is the director of the vitreoretinal surgery fellowship program and director of pediatric vitreoretinal surgery as well as director of telemedicine (ophthalmology). He may be reached at dariusm@stanford.edu.
1. Silva PS, Cavallerano JD, Aiello LM. Ocular telehealth initiatives in diabetic retinopathy. Curr Diab Rep 2009;9(4):265-71
2. Kumar S, Giubilato A, Morgan W, Jitskaia L, et al. Glaucoma screening: Analysis of conventional and telemedicine-friendly devices. Clin Experiment Ophthalmol 2007;35(3):237-43.
3. AREDS2-HOME Study Research Group, Chew EY, Clemons TE, Bressler SB, Elman MJ, Danis RP, Domalpally A, Heier JS, Kim JE, Garfinkel R. Randomized trial of a home monitoring system for early detection of choroidal neovascularization home monitoring of the Eye (HOME) study. Ophthalmology 2014;121:535-44.
4. Tsui I, Drexler A, Stanton AL, Kageyama J, Ngo E, Straatsma BR. Pilot study using mobile health to coordinate the diabetic patient, diabetologist, and ophthalmologist. J Diabetes Sci Technol 2014 Jul;8(4):845-9.
5. http://www.novartis.com/newsroom/media-releases/en/2014/ 1824836.shtml (accessed 1/25/15)
6. http://abc7news.com/health/stanford-implant-could-fight-glaucoma/485552/ (accessed 1/25/15)
7. Schwartz SD, Harrison SA, Ferrone PJ, Trese MT. Telemedical evaluation and management of retinopathy of prematurity using a fiberoptic digital fundus camera. Ophthalmology 2000;107:25-8.
8. Photographic Screening for Retinopathy of Prematurity (Photo-ROP) Cooperative Group. The photographic screening for retinopathy of prematurity study (photo-ROP). Primary outcomes. Retina 2008 Mar;28(3 Suppl):S47-54.
9. Fijalkowski N, Zheng LL, Henderson MT, Wang SK, Wallenstein MB, Leng T, Moshfeghi DM. Stanford University Network for Diagnosis of Retinopathy of Prematurity (SUNDROP): Five years of screening with telemedicine. Ophthalmic Surg Lasers Imaging Retina 2014;45(2):106-13.
10. Quinn GE, Ying GS, Daniel E, Hildebrand PL, Ells A, Baumritter A, Kemper AR, Schron EB, Wade K; e-ROP Cooperative Group. Validity of a telemedicine system for the evaluation of acute-phase retinopathy of prematurity. JAMA Ophthalmol 2014;132:1178-84.
11. Fierson WM; American Academy of Pediatrics Section on Ophthalmology; American Academy of Ophthalmology; American Association for Pediatric Ophthalmology and Strabismus; American Association of Certified Orthoptists. Screening examination of premature infants for retinopathy of prematurity. Pediatrics. 2013 Jan;131(1):189-95.
12. Fierson WM, Capone A Jr.; American Academy of Pediatrics Section on Ophthalmology, American Academy of Ophthalmology, and American Association of Certified Orthoptists. Telemedicine for evaluation of retinopathy of prematurity. Pediatrics 2015 Jan;135(1):e238-54.
13. Li LH, Li N, Zhao JY, Fei P, Zhang GM, Mao JB, Rychwalski PJ. Findings of perinatal ocular examination performed on 3573, healthy full-term newborns. Br J Ophthalmol 2013 May;97(5):588-91.