Scientists evaluated the efficacy of time outdoors per school day over two years on myopia onset and shift, as part of a prospective, cluster-randomized, examiner-masked, three-arm trial.
They included 6,295 students ages 6 to 9 from 24 primary schools in Shanghai, China, stratified and randomized by school in a 1:1:1 ratio to control (n=2,037), test I (n=2329) or test II (n=1,929) group.
An additional 40 or 80 minutes of outdoor time was allocated to each school day for test I and II groups. Children in the control group continued their habitual outdoor time. Objective monitoring of outdoor and indoor time, and light intensity each day was measured with a wrist-worn device during the second-year follow-up.
Main outcome measures included the two-year cumulative incidence of myopia (defined as cycloplegic spherical equivalent [SE] of ≤-0.5 diopters at the right eye) among the students without myopia at baseline and changes in SE and axial length (AL) after two years.
Here are some of the findings:
- The unadjusted two-year cumulative incidence of myopia was 24.9 percent for controls, 20.6 percent for the test I group, and 23.8 percent for test II group.
- The adjusted incidence decreased by 16 percent [Incidence Risk Ratio (IRR)=0.84; CI, 0.72 to 0.99; p=0.035] in test I and 11 percent (IRR=0.89; CI, 0.79 to 0.99; p=0.041) in test II when compared with the control group.
- The test groups showed less myopic shift and axial elongation compared with the control group:
– test I: -0.84 D and 0.55 mm;
– test II: -0.91 D and 0.57 mm;
– control: -1.04 D and 0.65 mm.
- No significant difference was found in the adjusted incidence of myopia and myopic shift between the two test groups.
- The test groups had similar outdoor time and light intensity (test I: 127 ±30 minutes/day and 3,557 ±970 lux/minute; test II: 127 ±26 minutes/day and 3,662 ±803 lux/minute), but significantly more outdoor time and higher light intensity compared with the control group (106 ±27 minutes/day and 2,984 ±806 lux/minute).
- Daily outdoor time of 120 to 150 minutes at 5,000 lux/minutes or cumulative outdoor light intensity of 600,000 to 750,000 lux significantly reduced the IRR by 17 to 31 percent.
Scientists wrote that increasing outdoor time reduced the risk of myopia onset and myopic shifts, especially in nonmyopic children. They added that the protective effect of outdoor time was related to the duration of exposure as well as light intensity. Finally, they noted, the dose-response effect between test I and test II wasn’t observed probably due to insufficient outdoor time achieved in the test groups, suggesting that proper monitoring on the compliance of outdoor intervention is critical to see the protective effect.
Ophthalmology 2022. June 29. [Epub ahead of print].
XiaHe X, Sankaridurg P, Wang J, et al.
GCC Thinning and Vision QOL
Researchers wrote that faster structural changes may be associated with worse vision-related quality of life in patients with glaucoma. As such, they evaluated the association between the rate of ganglion cell complex (GCC) thinning and the Visual Function Questionnaire in glaucoma.
This retrospective analysis of a longitudinal cohort was designed in October 2021. Patients were enrolled from the Diagnostic Innovations in Glaucoma Study and the African Descent and Glaucoma Evaluation Study. Two hundred thirty-six eyes of 118 patients with diagnosed or suspected glaucoma were followed up with imaging for a mean of 4.1 years from September 2014 to March 2020.
The Visual Function Questionnaire was evaluated using the 25-item National Eye Institute Visual Function at the last follow-up visit. GCC thickness was derived from macular optical coherence tomography scans and averaged within three circular areas (3.4 degrees, 5.6 degrees and 6.8 degrees from the fovea) and superior and inferior hemiregions. Linear mixed-effects models were used to investigate the association between the rate of GCC thinning and Rasch-calibrated Visual Function Questionnaire score.
The mean (SD) age was 73.2 (8.7) years, 65 participants (55.1 percent) were female, and 53 participants (44.9 percent) were African American. Race was self-reported by the participants. Here were some of the findings:
- Mean composite Rasch-calibrated National Eye Institute Visual Function Questionnaire score was 50.3 (CI, 45.9 to 54.6).
- A faster annual rate of global GCC thinning in the better eye was associated with a higher disability reflected by the composite National Eye Institute Visual Function Questionnaire score (-15 [CI, -28.4 to -1.7] per 1 µm faster; p=0.03).
- When stratified by degrees from the fovea, the 5.6-degree and 6.8-degree areas were associated with the composite National Eye Institute Visual Function Questionnaire Rasch-calibrated score (-14.5 [CI, -27 to -2] per 1 µm faster; R2=0.201; p=0.03; and -23.7 [CI, -45.5 to -1.9] per 1 µm faster; R2=0.196; p=0.02, respectively), and -8 (CI, -16.8 to 0.8) per 1 µm faster for the 3.4-degree area (R2=0.184; p=0.07) after adjusting for confounding factors.
Researchers wrote that the findings suggested that faster and sectoral central location of ganglion cell complex thinning provided useful information in determining the risk of vision-related quality of life in glaucoma. They added that monitoring macular structure may be useful for determining the risk of functional impairment in glaucoma.
JAMA Ophthalmol 2022. June 4. [Epub ahead of print].
Nishida T, Moghimi S, Mohammadzadeh, et al.
RUBY Trial: Mixed Results of Combination Therapy for DME
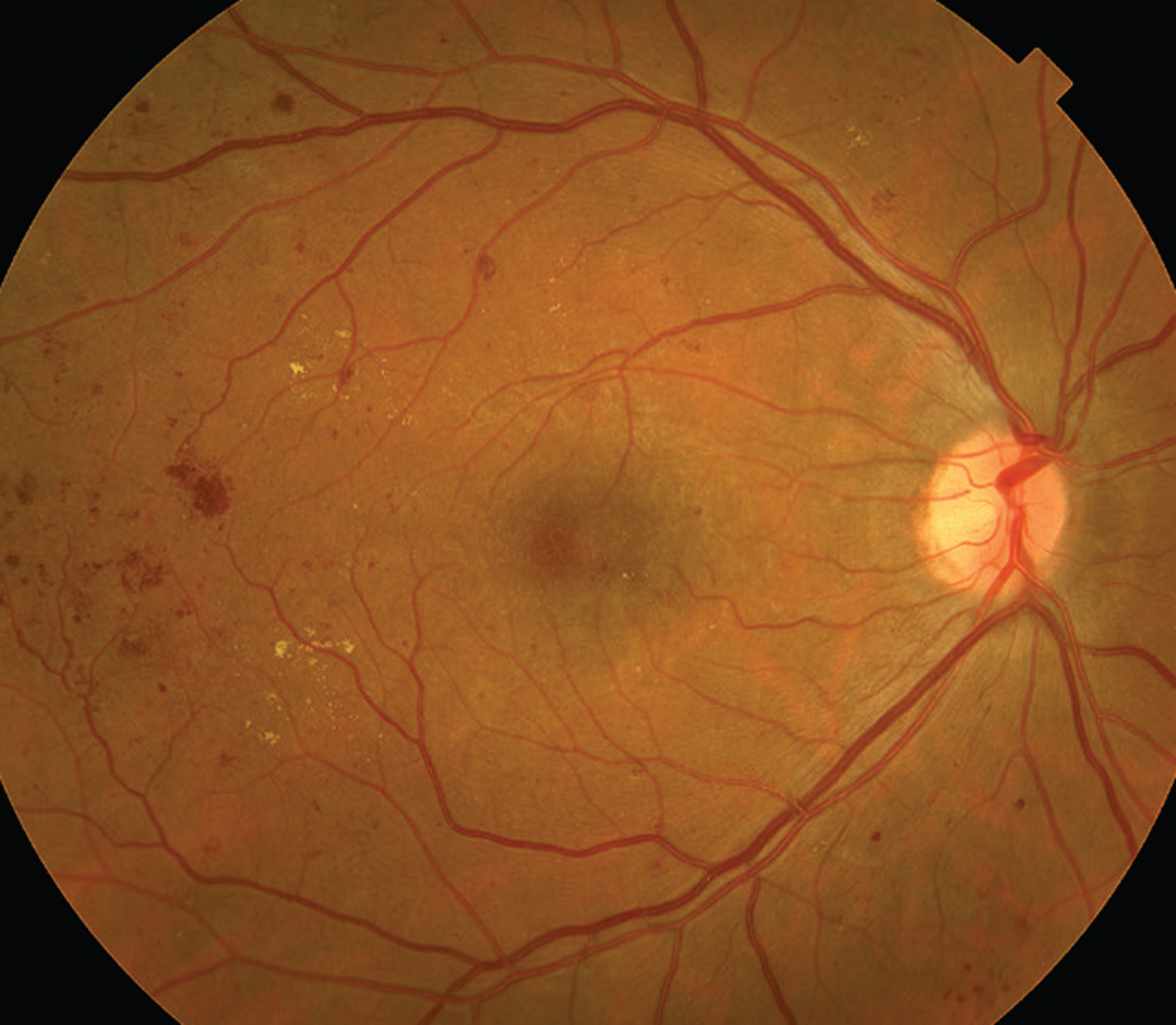 |
| DME proved to be a tough opponent to an aflibercept-nesvacumab combo. |
When paired with aflibercept, nesvacumab, an investigational human antibody that inhibits angiopoietin 2 (Ang2), has shown no additional visual benefits in patients with diabetic macular edema after 36 weeks, according to published results of the Phase II RUBY randomized trial, funded by Regeneron Pharmaceuticals and Bayer HealthCare.1
The reported efficacy, and subsequent Food and Drug Administration approval, of the bispecific antibody faricimab has generated interest in retinal treatments that target both the Ang2 and vascular endothelial growth factor pathways.
Despite the visual acuity findings, the RUBY study authors, led by David M. Brown, MD, said that a combination using a high dose of nesvacumab with aflibercept showed a signal of greater efficacy in reducing central subfield thickness than intravitreal aflibercept injections (IAI) alone. Dr. Brown is with the Retina Consultants of Texas in Houston, and also consults for Regeneron.
The trial randomized 302 eyes 1:2:3 to nesvacumab 3 mg and aflibercept 2 mg (low dose, LD/IAI), nesvacumab 6 mg plus aflibercept 2 mg (high dose, HD/IAI) or IAI 2 mg at baseline and weeks four and eight. The LD/IAI arm continued at q8 weeks; the HD/IAI arm was rerandomized at week 12 to q8- or q12-week dosing; and the IAI arm continued on q8- or q12-week dosing or switched HD/IAI combination q8 weeks through week 32.
At week 12, improvements in best-corrected visual acuity for the LD/IAI and HD/IAI and IAI arms were 6.8, 8.5 and 8.8 letters, respectively. Changes at 36 weeks were similar.
CST changes (standard deviation) at week 12 for the three respective arms were -169.4 (155.86), -184 (143.69) and -174.6 µm (160.36, p=0.0183 HD/IAI vs. IAI). At week 36, the changes were:
- -210.4 µm for the LD/IAI arm (p=0.004);
- -223.4 µm for the q8-week HD/IAI arm (p=0.0365);
- -193.7 µm for the q12-week HD/IAI arm (p=0.0454);
- -161.9 µm for the IAI q8-week arm (no p value);
- -210.4 µm for the IAI q12-week arm (p=0.9266); and
- -203.7 µm for the IAI to HD/IAI arm (p=0.4116).
Other key 36-week outcomes reported for the LD/IAI, HD/IAI and q12-week IAI arms were:
- Proportion of eyes with complete resolution of fluid at the foveal center: 75.6 (p=0.2029), 86.4 (p=0.0188) and 70.8 percent (p=0.5604).
- Proportion of eyes with CST ≤300 µm: 66.7 (p=0.0125), 72.7 (p=0.0041) and 54.2 percent (p=0.3139).
- Proportion of eyes with a more than two-step improvement in Diabetic Retinopathy Severity Scale score: 26.7 (p=0.8896); 34.1 (HD/IAI q8-week, p=0.5021), 34 (HD/IAI q12-week, p=0.5273) and 25.5 percent (p=0.8683).
Over the 32-week treatment period, the mean number of intravitreal injections administered was 7.2 ±0.92 for LD/IAI q8 weeks; 5.9 ±0.35 for HD/IAI q8 weeks; 5.1 ±0.58 for HD/IAI q12 weeks; 5.9 ±0.45 for IAI q8 weeks; 4.8 ±0.63 for IAI q12 weeks; and 5.8 ±0.44 for IAI converted to HD/IAI q8 weeks.
Rates of ocular adverse events were similar across the three treatment protocols throughout the 36-week study, with one or more ocular AD reported in 30 percent in the LD/IAI patients, 31 percent in the HD/IAI arm and 25.7 percent in the IAI patients. The most common AE was conjunctival hemorrhage, reported in 8, 2 and 7.2 percent of patients, respectively. Two serious ocular AEs were reported in the HD/IAI group: a case of iridocyclitis and another of retinal artery occlusion, which the authors considered related to the study treatment.
Researchers acknowledged that findings of the RUBY study contrast with those of the BOULEVARD study of faricimab (10), a bispecific antibody targeting Ang2 and vascular endothelial growth factor that showed significantly greater improvements in BCVA compared with ranibizumab monotherapy. They gave a number of reasons for the RUBY findings, including how treatment-naïve patients were distributed across treatment arms. They also noted the ocular and systemic safety profiles of nesvacumab/IAI was in line with IAI monotherapy.
While RUBY didn’t show any additive benefit in vision with nesvacumab, the anatomic signals were noteworthy. “The indication of positive anatomic effects may warrant further investigation of the role of anti-Ang2 agents in combination with anti-VEGF therapy,” Dr. Brown and colleagues wrote.
1. Brown DM, Boyer DS, Csaky K, et al, on behalf of the RUBY Investigators. Intravitreal nesvacumab (antiangiopoietin 2) plus aflibercept in diabetic macular edema: Phase 2 RUBY randomized trial. Retina 2022;42:1111.
2. Sahni J, Patel SS, Dugel PU, et al. Simultaneous inhibition of angiopoietin-2 and vascular endothelial growth factor-A with faricimab in diabetic macular edema: BOULEVARD Phase 2 randomized trial. Ophthalmology 2019;126:1155.



